* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Termination of the Acute Inflammatory Response
Survey
Document related concepts
Rheumatic fever wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Immune system wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Atherosclerosis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Transcript
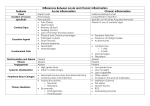
Termination of the Acute Inflammatory Response To stop elimination we must stop the stimulus. The stimulus will have started a reaction in the body and our body needs to stop that reaction as well. How are these reactions stopped? The mediators produced are quickly broken down (They have a very short half-life). They are degraded. If the stimulus is still present, mediators will be replaced. This is why we need to remove the stimulus first. To make sure the mediators are broken down as soon as possible. Another reason is that neutrophils have very short life spans (half-lives) and will die within hours of being in the circulation. If the stimulus is still there the neutrophils will also be replaced. After resolving the stimulus, we have other stop signals such as: Switching the type of arachidonic acid metabolite produced. Liberating anti-inflammatory cytokines (TGF-B and IL-10). Anti-Inflammatory Lipid Mediators (Resolvins and Protectins). (Cholinergic discharge) Neural impulses to inhibit TNF production in macrophages. These are very important because there will still be inflammation and we need to stop it after resolving the stimulus. We know that mediators cause vasodilation and vascular leakage, but now we need to know what mediators actually are. Mediators of Inflammation Mediators are either cell derived or from plasma proteins. The cells they are made of can be mast cells or macrophages. The first things in the body that recognize a stimulus are macrophages. The macrophages react by producing mediators. These mediators recruit more leukocytes and fight microbes. Remember, we know that in order to kill microbes there must be receptors on the macrophages that recognize them (E.g. toll-like receptors, g-protein receptors, opsonin receptors, cytokine receptors). 1 All these receptors are not only present in macrophages they are also present in other inflammatory cells. The macrophage will recognize the microbe and start the secretion of cytokines. This means that the cytokine will go to other inflammatory cells, bind them and activate them. Earlier we said mediators can be produced from cells or plasma proteins. They can also be produced by endothelial cells, vascular smooth muscle cells, epithelial cells and fibroblasts if these cells are induced. Cell derived mediators: Pre-synthesized: stored in granules inside cells (E.g. histamine and mast cells) and released upon stimulation by exocytosis. OR De-novo: Made from scratch upon stimulation (E.g. Prostaglandins). Plasma protein derived: Are synthesized in the liver and will be found in the circulation in their inactive form. They are activated upon stimulation (in the presence of a stimulus). Active mediators are produced in response to various stimuli. This is very essential because this will guarantee that there will not be a release of mediators when there is no need for them. It will protect us from any unnecessary inflammatory reaction. They will only be released if there is a harmful stimulus (toxins, microbes...anything that triggers an inflammatory response). One mediator can stimulate the release of another. Why is this useful? 1. Amplification of the reaction (stimulates another mediator with a similar reaction), such as TNF which can activate the release of interleukin-1 from endothelial cells. 2. Counteract the reaction of the first mediator (by having an opposite action to the first mediator), such as anti-inflammatory mediators. 2 Mediators vary in their range of cellular targets. Mediators can have various sites of action. They might have two different actions in two different cells OR they can have the same action in two different cells. (Mediate various actions) Once activated and released from the cell, most of these mediators are short-lived. These mediators will either decay (E.g. prostaglandins) or they will be deactivated by certain enzymes (kinases). Table notes: Prostaglandins: synthesized upon stimulation. Platelet-activating factor: activates expression of p-selectin. Cytokines: TNF decreases appetite and causes anorexia. 3 This table helps us understand the link between inflammation, thrombosis and cardiovascular disease. Outcomes of acute inflammatory reactions Complete Resolution: Everything returns to how it was before. Inflammation happened due to a stimulus; once the stimulus was removed everything will go back to normal. For this to happen, three conditions must be met: Injury is limited or short lived. Little tissue destruction. Parenchymal cells must be able to regenerate. How do we meet these conditions? Removal of cellular debris and microbes. They will be engulfed by macrophages. Resorption of edema fluid by lymphatics. However, if we have: Substantial tissue destruction. The tissue involved is incapable of regeneration. Abundant fibrin exudation in tissues or serous cavities. These tissues will be replaced by fibrous tissue. This can either result in scar formation or fibrosis. Normally in acute inflammation, because the damage is small (in general), scar formation occurs. In chronic inflammation mainly fibrosis occurs because of the extensive damage. Fibrin oxidation will be produced as a result of inflammation, exudates will be formed and because there is a lot of destruction, cavities will be formed. The fiber exudates will fill these cavities. Connective tissue starts to grow into these cavities in what is called organization. However, this connective tissue is not functional. It only happens to fill the gaps. 4 So to sum up we have four outcomes: 1. Complete resolution 2. Healing by connective tissue (scar formation or fibrosis) 3. Both scar generation and fibrosis (most common) 4. Progression into chronic inflammation due to: Persistence of the injurious agent (E.g. peptic ulcer) Interference of the healing process (healing is not complete) Figure Notes: Pus formation: rich in microbes Angiogenesis: needed to achieve fibrosis (main way of healing). 5 Although inflammation has damaging effects, it is essential for human life. It protects us from microbes and other harmful stimuli. Sometimes we need to encourage or discourage inflammation: Warm compresses encourage inflammation (increase the strength of inflammation) o E.g. pharyngitis Cold compresses discourage inflammation (decrease the strength of inflammation) o E.g. traumatic injury If inflammation is not resolved and is prolonged (e.g. persistent stimulus) this acute inflammation can progress into chronic inflammation. Chronic Inflammation Inflammation of prolonged duration (weeks or months) in which inflammation, tissue injury and attempts at repair (through fibrosis) coexist in varying combinations. Chronic inflammation does not always result from acute inflammation. Sometimes we might have chronic inflammation to start with. Causes of chronic inflammation: 1. Persistent infections by microorganisms that are difficult to eradicate. (E.g. Tuberculosis) 2. Immune-mediate inflammatory diseases, we have two groups: Hypersensitivity (any excessive reaction of the immune system) Autoimmune diseases (react to something it shouldn’t, should not recognize self antigens) These two are chronic in nature to begin with, so cannot be cured. 3. Prolonged exposure to potentially toxic agents, either: Exogenous (from outside the body) such as silica, which can result in silicosis (chronic lung disease) if inhaled for a prolonged period of time. Endogenous (from inside the body) such as LDLs; once the concentration of these molecules are high enough they pass through the vascular wall, accumulate there, are 6 oxidized and then start to recruit macrophages (initiate an inflammatory reaction). This starts the formation of plaques which can continue to grow and compromise the blood supply to certain organs or they can rupture and result in thrombosis. Both can result in death, so they are very critical situations. Morphological Features Chronic inflammation is characterized by: Infiltration with mononuclear cells, which include: macrophages, lymphocytes and plasma cells. At this level, the immune reaction is much stronger and because of this the destruction is more. Tissue destruction, induced by the persistent offending agent or by the inflammatory cells themselves. Inflammatory cells have the same ability to kill microbes and kill normal tissue surrounding the microbes. Attempts at healing by connective tissue replacement of damaged tissue, accomplished by proliferation (formation) of small blood vessels (angiogenesis) and in particular, fibrosis. To achieve fibrosis, we need angiogenesis. Role of Macrophages The macrophage is the dominant cellular player in chronic inflammation (predominates 48 hours after the stimulus). They are components of the mononuclear phagocyte system. Where do macrophages come from? They are recruited from the circulation. They are called monocytes when in circulation, when they are recruited to the tissue they are then called macrophages. In different tissues they have different names. In the liver: kupffer cells, in the CNS: microglial cells, in the lungs: alveolar macrophages 7 Monocytes have a short half-life. They only have a 1 day half-life. Whereas the life span of tissue macrophages is several months or years. They come from the bone marrow as monoplasts, go to the circulation and are monocytes then they go to the tissue and are called macrophages. Macrophages may be activated by a variety of stimuli: 1. Microbial products that engage TLRs (toll-like receptors) and other cellular receptors like: G-protein coupled recepors Opsonin receptors: receptors that recognize opsonin (molecules that coat microbes through a process called opsinization, and then they will be bound to the opsonin receptors to be recognized). TLRS are the most important and are found on macrophages. Macrophages recognize microbes by the engagement of TLRS and activate the macrophages. 2. Cytokines (E.g. IFN-y) secreted by sensitized T lymphocytes and by natural killer cells. They can activate macrophages and any other inflammatory cells. These receptors are present in all inflammatory cells, not only macrophages. They activate inflammatory cells via engagement. 8 9