* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download File
Survey
Document related concepts
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Rheumatic fever wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Atrial septal defect wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
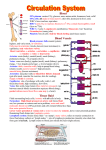
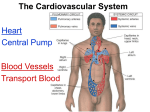
Cardiovascular System • Consists of blood, heart and blood vessels • Cardiology – study of the heart The Heart • Located in the mediastinum – mass of tissue that extends from the sternum to the vertebral column • Rests on the diaphragm • Approx. the size of closed fist • Apex – pointed end (leans toward left) • Base – rounded end (toward right) • Mass: females ~ 250g males ~ 300g Function of the Heart • Pump oxygenated blood to the tissues and deoxygenated blood to the lungs Coverings of Heart • Pericardium – double layered sac that covers the heart oParietal pericardium – outer layer oVisceral pericardium – inner layer (also called epicardium) oPericardial cavity – fluid filled space between the two layers; contains fluid to decrease friction Layers of the Heart Wall • Epicardium – thin, protective outer layer • Myocardium - thick middle layer; makes up most of heart; function is to pump blood • Endocardium - smooth, inner lining; also forms valves of heart Chambers of the Heart • 4 chambers o2 atria – (upper, thin-walled) receive blood • Have auricles – pouches that increase the surface area of the atria so it can hold a greater volume of blood • Separated by interatrial septum o2 ventricles – (lower, thicker) pump blood • Separated by interventricular septum • Right atrium -receives deoxygenated blood from superior vena cava, inferior vena cava & coronary sinus oSuperior vena cava – returns blood to heart from head, neck & arms oInferior vena cava – returns blood to heart from chest, abdomen, pelvis & legs oCoronary sinus – returns blood to right atrium from myocardium • Left atrium - receives oxygenated blood from the lungs via the pulmonary veins • Right ventricle - receives blood from the right atrium & pumps it out to the lungs via the pulmonary arteries • Left ventricle - forms apex oReceives blood from left atrium & pumps it out to tissues of the body via the aorta Features of Ventricles • Trabeculae carneae – ridges in the ventricle • Papillary muscle - masses of myocardium that project into the ventricles Heart Valves • Function is to keep blood flowing in one direction (prevents backflow) • 2 types of valves o1. Atrioventricular valves (AV) o2. Semilunar valves (SL) Atrioventricular Valves • Tricuspid valve – between right atria & right ventricle (3 cusps) • Bicuspid valve – between left atria & left ventricle (2 cusps) o Also called the mitral valve • Chordae tendineae - connective tissue strands that connect papillary muscle to cusps of atrioventricular valves Semilunar Valves • valves at the base of large vessels that carry blood from the ventricles • Pulmonary semilunar valve –at exit of right ventricle in base of pulmonary trunk • Aortic semilunar valve – at exit of left ventricle in base of ascending aorta • Valves open & close in response to pressure: • Atria fill with blood…causes increased pressure on AV valves. Atria contract, AV valves open, blood flows into ventricles. • Ventricles fill with blood…causes increased pressure on SL valves. Ventricles contract, SL valves open, blood flows into vessels. Coronary Circulation: Blood Supply for the Heart • Coronary arteries - surround the heart like a crown oBranch off the ascending aorta oSupplies heart cells with oxygen & nutrients • Coronary sinus – returns blood to the right atrium Fetal Circulation • Blood doesn’t need to go to lungs in a fetus • 2 shunts: o Foramen ovale – an opening on the interatrial septum of fetal heart • Closes to form the fossa ovalis o Ductus arteriosum – shunts blood from the pulmonary trunk to the aortic arch • Closes to form the ligamentum arteriosus (connects arch of aorta and pulmonary trunk) o Both shunts close by birth or w/in 1st year o If shunts don’t close, surgery is required Conduction System • Cardiac muscle is autorhythmic – it generates its own action potentials for muscle contraction • Both atria contract simultaneously, followed by both ventricles • Specialized cardiac muscles act as nerve tissue to distribute the impulse • 1. Excitation begins in sinoatrial node (SA node…also known as the pacemaker) in the right atrium. • 2. Action potential spreads to left atrium, allowing both atria to contract simultaneously • 3. Action potential spreads to atrioventricular node (AV node) located between right & left atria o Action potential slows at AV node so atria can fully empty and ventricles can fill; also AV node has smaller fibers • 4. Action potential spreads to Atrioventricular bundle, then to right & left bundle branches within the interventricular septum • 5. Purkinje fibers send the action potential to the ventricles, causing them to contract 0.2 seconds after atria contract Electrocardiogram (EKG or ECG) • Recording of electrical activity of heart to check the conduction system • Uses multiple electrodes attached to body • Stress test – EKG during strenuous exercise; compares resting heart to stressed heart • P wave – atrial contraction (depolarization); SA node activity • PQ interval – impulse delay at AV node • QRS complex – ventricular contraction (depolarization);Purkinje fiber activity oIt’s so much larger due to greater muscle mass of ventricles • T wave – ventricular relaxation (repolarization) **why can’t we see atrial relaxation??** EKG Abnormalities • Large P Wave - enlarged atria • Large Q wave – myocardial infarction (heart attack) • Large R wave - enlarged ventricles • Flat T wave - coronary artery disease • Wider PQ interval - abnormal conduction • Arrhythmia – abnormal beating of heart due to malfunction of conduction system o Tachycardia - fast heart rate o Bradycardia - slow heart rate o Asystole - lack of heart rate Cardiac Cycle • All the events associate with one complete heart beat • Systole – contraction Diastole – relaxation Atrial systole = ventricular diastole atria contract, ventricles relax AV valves open, SL valves closed ventricles fill with blood Atrial diastole = ventricular systole atria relax, ventricles contract AV valves close, SL valves open atria fill with blood Heart Sounds • Caused by the turbulence of blood when heart valves close • Stethoscope – instrument used to listen to heart sounds • Lubb – first sound heard; AV valves closing after ventricular systole begins • Dupp – second sound heard; SL valves close at beginning of ventricular diastole Heart Murmur • Abnormal heart sound • Gurgling noise before, between or after lubb-dupp sound • Most murmurs indicate a valve disorder • Mitral stenosis – narrowing of the mitral valve • Mitral valve prolapse – part of mitral valve is pushed back into the atria o Occurs in 10-15% of population ( 65% are female) Heart Disorders • 1. Ischemia – partial block of blood flow due to constriction or obstruction of a vessel • 2. Hypoxia – lack of O2 to heart muscle • 3. Angina – chest pain • 4. Myocardial infarction – heart attack due to myocardial cells dying • 5. Sudden cardiac death – conduction system stops; heart stops beating • 6. Congenital defects – present at birth Nervous System Control • Autonomic nervous system – no conscious control o Heart controlled by two branches of ANS • 1. Sympathetic Nervous System – increases heart rate & force of contractions due to release of norepinephrine • 2. Parasympathetic Nervous System – decreases heart rate due to the release of acetylcholine • Both work together to maintain homeostasis