* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CHAPTER 8 EMERGING AND RE
Nutrition transition wikipedia , lookup
Mosquito control wikipedia , lookup
Diseases of poverty wikipedia , lookup
Transmission and infection of H5N1 wikipedia , lookup
Antimicrobial resistance wikipedia , lookup
Antibiotic use in livestock wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Public health genomics wikipedia , lookup
Canine distemper wikipedia , lookup
Compartmental models in epidemiology wikipedia , lookup
Canine parvovirus wikipedia , lookup
Henipavirus wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Infection control wikipedia , lookup
Transmission (medicine) wikipedia , lookup
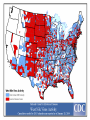
EMERGING AND RE-EMERGING INFECTIOUS DISEASES © National Museum of Health and Medicine, Washington, D.C., United States INFECTIOUS DISEASE • Infectious disease has played a prominent role in world history. – The Black Death in the Middle Ages killed 1/3 Europe’s population. – Measles destroyed the South American Aztec civilization. – Smallpox destroyed indigenous peoples of North and South America, facilitating the conquest of the New World. "Triumph of Death" (Black Plague) Painted in 1562 Infectious Disease- Trends • Receded in Western countries 20th century • Urban sanitation, improved housing, personal hygiene, antisepsis & vaccination • Antibiotics further suppressed Morb/Mort. • Since last quarter of 20th century- New & Resurgent infectious diseases • December 1967, Surgeon General William H. Stewart declared victory over infectious diseases Definition • Emerging infectious disease Newly identified & previously unknown infectious agents that cause public health problems either locally or internationally • Re-emerging infectious disease Infectious agents that have been known for some time, had fallen to such low levels that they were no longer considered public health problems & are now showing upward trends in incidence or prevalence worldwide JITMM, Bangkok, 12-14 December 2012 Infectious Diseases: A World in Transition AIDS Avian Influenza Ebola Marburg Cholera Rift Valley Fever Typhoid Tuberculosis Leptospirosis Malaria Chikungunya Zika Dengue JE Antimicrobial resistance UP ? DOWN Guinea worm Smallpox Yaws Poliomyelitis Measles Leprosy Neonatal tetanus Eradicated--smallpox EMERGING INFECTIOUS DISEASES • First transition (also referred to as crowd transition) – Occurs when people begin to live in much closer proximity to one another – Higher population density – Proximity between populations allows for easy transmission of disease EMERGING INFECTIOUS DISEASES • Second transition – Neighboring civilizations made contact with each other through war or trade – Contact allowed the exchange of pools of infectious organisms and vectors between populations. EMERGING INFECTIOUS DISEASES • Third transition – Worldwide exploration and colonization led to the identification of new populations – Newly identified populations came into contact with pathogens never seen before within their cultures. – Immunologically naïve and susceptible populations.(Alaska-measles/Native Americans smallpox) EMERGING INFECTIOUS DISEASES • Fourth transition – this is happening today. The ongoing causes are: – Globalization – – – – – – – – – – Global urbanization Increase in population density Poverty Social upheaval Travel New behaviours (medical / sexual tourism) Long distance trade Technology development Land clearance Weather / Climate Geographical Distribution of West Nile Virus Origin: Uganda Global Distribution of Cholera Origin: India Factors Contributing To Emergence AGENT • Evolution of pathogenic infectious agents (microbial adaptation & change) • Development of resistance to drugs • Resistance of vectors to pesticides • Environment • Climate & changing ecosystems • Economic development & Land use (urbanization, deforestation) • Technology & industry (food processing & handling) • International travel & commerce • Breakdown of public health measure (war, unrest, overcrowding) Summary of Climate Trends Temperature • Maine will warm statewide by 1.0 to 1.5˚C by 2060 – Warmer winters – Warmer summers • Warmer temperatures will be attained earlier in the year • Overall by 2050, Maine’s temperatures will resemble those seen today in Massachusetts Precipitation • Statewide precipitation will increase by 10cm by 2060 • Summer rainfall will remain steady in all parts of Maine except the central mountains Meaning for Vector-borne Diseases in Maine Factors Contributing To Emergence HOST • • • • • • • • Human demographic change (inhabiting new areas) Human behaviur (sexual & drug use) Unsafe sexual practices (HIV, Gonorrhoea, Syphilis) Changes in agricultural & food production patterns- foodborne infectious agents (E. coli) Increased international travel (Influenza) Outdoor activity Human susceptibility to infection (Immunosuppression) Poverty & social inequality Uncontrolled Urbanization & Population Displacement • Growth of densely populated cities- substandard housing, unsafe water, poor sanitation, overcrowding, indoor air pollution • Problem of refugees & displaced persons • Diarrheal & Intestinal parasitic diseases, ARI Lyme disease (B. burgdorferi)- Changes in ecology, increasing deer populations, suburban migration of population The global air network Sudden Acute Respiratory Syndrome (SARS) Emerged in 2003 – hotel in Hong Kong Rapid spread worldwide – 8098 persons within 3-4 months Last case in 2004 Person-to-person respiratory spread – droplets Source – wet markets (live animals) Reservoir – ferrets Agent – corona virus Severe Acute Respiratory Syndrome: SARS • SARS became readily transmissible in the 1990s. • First documented case was identified in mainland China. • It is transmitted by droplet aerosol and fomites deposited on the respiratory mucosal epithelium. • Pneumonia like disease. • 2002-2003 outbreak infected 8400+ with 916 confirmed dead. WEST NILE VIRUS • West Nile virus is caused by an arbovirus (arthropod borne, RNA viruses). • The virus is carried in the saliva of mosquitoes and is transmitted through bites. • Birds are the primary hosts (Crow and Cardinals) • Infection is spread from bird to bird by mosquitoes. WEST NILE VIRUS: Pathogenesis • Most infected people are asymptomatic unless the infection causes an invasive neurological disease called West Nile Fever. – Symptoms include fever, headache, myalgia, and anorexia. – Severe infection can cause profound fatigue, myocarditis, pancreatitis, and hepatitis. – Particularly severe cases can result in encephalitis or meningitis and death. – The illness can also be transferred through blood transfusions and transplantation. 21 Imported Arboviral Illnesses • Exotic Arboviruses are important public health risks for the United States – Competent vectors are present in parts of the United States – These arboviruses include • • • • • • • • Dengue Yellow fever Chikungunya Tick-borne encephalitis Japanese encephalitis Venezuelan equine encephalitis Rift Valley fever Zika • Dengue and Yellow Fever are nationally reportable illnesses • Travel history is extremely important in the diagnosis of arboviral illnesses Aedes aegypti mosquito 25 Distribution of mosquito Maine Center for Disease Control and Prevention ZIKA Virus • The latest plague (geographic spread due to global travel) • What we do and do Not know (is it more virulent due to mutations now) • Look at other viruses (rubella,CMV) 27 History • First isolated in 1947 from a rhesus monkey in the Zika forest of Uganda • First isolated from humans in 1968 in Nigeria • Outbreaks occurred in Africa, Southeast Asia, the Pacific Islands and the Americas • Americas – Chile (Easter Island), March 2014 – Brazil, May 2015 – Puerto Rico, December 2015 Maine Center for Disease Control and Prevention Transmission • Through mosquito bites – Primarily Aedes aegypti species(albopictus) – Humans are the reservoir • From mother to child--intrauterine – No reports from breastfeeding to date • Possibly through infected blood- and sexual contact – No reports from transfusions – 36 probable reports of spread through sexual contact Maine Center for Disease Control and Prevention Symptoms • About 1 in 5 people will become ill • Symptoms include: – – – – – Fever Rash Joint Pain Conjunctivitis Muscle pain, headache, pain behind the eyes, vomiting • Clinical illness is usually mild and lasts for several days to a week • Incubation typically 2-14 days Maine Center for Disease Control and Prevention Diagnosis/Treatment • Single-stranded RNA virus, genus Flavivirus • Differential diagnosis is broad and includes: dengue, leptospirosis, malaria, rickettsia, group A strep, rubella, measles, parvovirus, enterovirus, adenovirus, chikungunya • • Diagnosis by PCR in first 4 days—IgM 4-7 days Urine + PCR up to 14 days • Positive PCR suggests infectivity (not entirely clear) • Cross reaction with Dengue + Chik. Igm • There is no specific treatment Maine Center for Disease Control and Prevention Countries with past or current evidence of Zika virus transmission Maine Center for Disease Control and Prevention Map courtesy of ZIKA Virus in Pregnancy – Limited Information • No evidence of increased susceptibility • Infection may occur in any trimesterneurologic damage likely in first trimester • Incidence in pregnancy not known • No evidence that ZIKA is more severe 33 Latest Information on ZIKA • Enough evidence – ZIKA virus during pregnancy causes microcephaly—also other brain defects, eye defects, hearing loss, impaired growth • Birth defects most likely in first trimester • Women with ZIKA virus infection - wait 8 weeks after symptoms before attempting conception • A man infected with ZIKA can transmit – avoid 34 sex during pregnancy(condoms) Zika and Pregnant Women-DX • Pregnant women with symptoms—PCR1-4 days—urine up to 14 days • Pregnant Women IgM after 4 days • Ultasonography may be indicated • Amniocentesis guidelines 35 ZIKA and Guillain-Barre • New case control studies proves a link • Rates may be .24/1000 cases • Other neurologic syndromes under investigation 36 ZIKA in US as of November, 2016 • Travel associated ZIKA – 4496 • • • • • Pregnant – 1114(18 cases microcephaly) Sexually transmitted 36 Guillain-Barre – 13 Locally Acquired ZIKA – 14(Miami and Texas) Maine -12 cases—all travel • US Territories – 33,258 • Pregnant – 2561 • Guillain-Barre - 48 37 Updates on ZIKA • The virus is present longer in semen than blood(up to 62 days) • After ZIKA a man should wait 6 months before attempting conception • Natural infection likely gives long term immunity • FDA is developing a screening test for blood— defer donation if recent travel 38 Who should be tested for ZIKA • Symptomatic individuals with travel history to a Zika affected country • Pregnant women with travel history to Zika affected country • Partners of pregnant women with travel history to a Zika affected country 39 Public Health • Notify providers of Zika virus and how to test • Warn residents when traveling to ZIKA areas to avoid mosquito bites- use DEET/bed nets • Cruise ship destinations – Zika • Monitor for locally acquired transmission - in US – Miami Maine Center for Disease Control and Prevention What is new with ZIKA • • • • • • • • WHO downgraded Zika from PH emergency to threat ZIKA identified in Texas Zika epidemic may have peaked Severity of Zika in SA may be Due to coinfections Vaccine testing in full swing Zika funding passed by congress Zika may persist in vaginal fluid for weeks Female to male transmission documented ZIKA – The Future • Vaccine—active research now— phase I trials • Sterile mosquitoes - trials • Mosquito control – now---Brazil • Anti-virals- nothing yet available 42 Chikungunya (that which bends you over)- Epidemiology • Transmitted by Aedes aegypti and less albopictus • Monkeys, apes and rodents act as reservoirs • 3 genotypes – West Africa – East Africa – Asia • Described first in 1955 – Makonde plateau • 2013 first cases in Caribbean • 2014 cases transmitted in Florida 44 Chikungunya – Signs and Symptoms • • • • Incubation – 1-12 days, typically 2-3 Majority infected get symptoms Fever to 104° - petechial rash on trunk Systemic symptoms – headache, nausea, conjunctivitis, loss of taste, pedal edema • Fever resolves 2-3 days – joint pains persists weeks to years 45 Chikungunya - Diagnosis and Prevention • Diagnosis – RT-PCR, virus isolation – serology • Prevention – mosquito control – personal protection • Vaccine – not available – phase II trials • Treatment – symptomatic – NSAIDS • Chronic arthritis – Ribavirin might help – maybe Chloroquine - steroids not useful 46 Prevention of Arboviral Illnesses • At Home: – EPA approved repellents: DEET, Picaridin, oil of lemon of eucalyptus, or IR3535 – Wear protective clothing Permethrin-treated clothing – Limit outdoor activities in high-risk areas – Screens on windows and doors – Household source reduction • Abroad: – Use bed nets – Receive the YF vaccine – Use the same practices that you would use to prevent mosquito-borne illnesses at home Mosquito Protection Control Directed at the Immature Stages • Biological Control – Predators – Pathogens and Parasites – Genetic Control • Mechanical (Environmental) Control – Source Reduction – Environmental Manipulation • Chemical Control – – – – Oils Paris Green Insecticides Insect Growth Regulators (IGRs) Control Directed at the Adult Stages • Aerosols, Mists and Fogs • Ultra-low-volume applications • Residual house-spraying Ebola Virus Disease (EVD) Outbreak 2014 2014 West Africa Outbreak • The 2014 Ebola outbreak is the largest Ebola outbreak in history and the first in West Africa. • The current outbreak is affecting 3 countries in West Africa. 52 Current as of 10/2/2014 Ebola • Previously known as Ebola hemorrhagic fever • Ebola Virus Disease (EVD) is caused by infection with a virus of the family Filoviridae, genus Ebolavirus • Natural reservoir of Ebola virus remains unknown • Researchers believe that the virus is animal-borne and that bats are the most likely reservoir. General EVD Background • Ebola Virus Disease (EVD) is one of numerous viral hemorrhagic fevers (VHFs). • The first Ebola virus species was discovered in 1976 in what is now the Democratic Republic of the Congo near the Ebola River. • EVD is often severe in humans, with case fatality rates reaching 50-90% in developing countries. • After an incubation period of a few days, symptoms usually begin abruptly. • The natural reservoir host of Ebolaviruses remains unknown. However, evidence suggests it is a zoonosis (animal-borne) with bats being the most likely reservoir.. 54 Ebolavirus species • Ebola virus (Zaire ebolavirus) • Sudan virus (Sudan ebolavirus) • Taï Forest virus (Taï Forest ebolavirus, formerly Côte d’Ivoire ebolavirus) • Bundibugyo virus (Bundibugyo ebolavirus) • Reston virus (Reston ebolavirus) nonhuman primates EBOLA -Outbreak History--1976 • 1976 Zaire (Congo) • 318 Reported Cases • 280 Deaths (88%) • 1976 – South Sudan • 284 reported cases • 151 deaths(38%) • 1976 – England • 1 Case(no deaths) Outbreak History -1976-2013 • 33 Previous Outbreaks • 2,361 Reported Case • 1,548 Deaths (66%) 2014- 2015 Outbreak • 27,580 Reported Cases • 11,297 Deaths -probable, confirmed and suspected Impact on United States • On September 30, CDC confirmed the first travelassociated case of Ebola to be diagnosed in the United States in a person who had traveled to Dallas, Texas from Liberia. The patient did not have symptoms when leaving West Africa, but developed symptoms approximately five days after arriving in the U.S. (arrived Sept. 20). • Contact tracing, a standard public health procedure, is immediately employed in order to identify and monitor those who may have been potentially exposed to a sick patient. • Even with the first U.S. confirmed case, Ebola does not pose a significant risk to the United States. • Fear level very high. 60 General EVD Transmission • Ebola virus is spread from one person to another through direct contact with: o Ebola-infected blood or body fluids, such as, but not limited to, urine, saliva, feces, vomit, and semen o Objects, such as needles, that have been contaminated with infected body fluids • Healthcare workers, family and friends, and others who come into close contact with Ebola-infected patients (including corpses of those who expired due to EVD) have the highest risk of exposure. 61 General EVD Transmission 62 General EVD Presentation • Symptoms may appear anywhere from 2 to 21 days after exposure to Ebola virus, although 8-10 days is most common. • Only symptomatic Ebolainfected patients are able to transmit EVD; Patients without symptoms who are infected with Ebola virus are not contagious. 63 General EVD Assessment • Timely diagnosis and treatment of EVD is important but challenging because the disease is difficult to diagnose clinically in the early stages of infection. • Because early symptoms, such as headache and fever, are nonspecific to EVD, cases of EVD may be initially misdiagnosed. • It is important to obtain an accurate and complete history of travel or potential contact with an Ebola case from a patient exhibiting Ebola-like symptoms. 64 Excerpt from CDC checklist for Patients Being Evaluated for EVD in US General EVD Treatment • There is no specific cure for Ebola virus infection. • There are no specific medications (e.g., antiviral drug) that have been proven to be effective against Ebola. • Symptoms of Ebola are treated supportively, as they appear. The following basic interventions, when used early, can increase the chances of survival. – Providing intravenous fluids and balancing electrolytes (body salts) – Maintaining oxygen status and blood pressure – Treating other infections if they occur 65 Infection Prevention and Control Recommendations • CDC recommends protection with gowns, gloves, boots, masks to prevent any contact with infectious materials with known or suspected Ebola Viral Disease (EVD). • Though these recommendations focus on the hospital setting, the recommendations for personal protective equipment (PPE) and environmental infection control measures are applicable to any healthcare setting. . 66 Vaccines • Human trials of experimental Ebola vaccines have begun in U.S. • Canada is to ship 800 vials of its Ebola vaccine to the World Health Organization • Recent data shows some success What is New With Ebola • • • • • Chronic ocular disease identified Persistence of ebola in seminal fluid(500 Days) Treatment with Favipiravir an anti-viral Persistence of Ebola in West Africa Public concerns minimal (despite ebola cases) • Infectious brain disease confirmed in patient treated at Maine Med • The Portland hospital took the precaution this week of suspending elective surgeries in order to sterilize its surgical equipment and facilities PRIONS AND PRION DISEASES • These infectious diseases are not caused by microorganisms. • They are caused by infectious proteins called prions. • Diseases are called transmissible spongiform encephalopathies (TSE). PRION HYPOTHESIS • Prions are proteins normally found on nerve cells and are known as PrPc (prion protein cellular). • Infectious prions are folded improperly and are known as PrPsc (prion protein scrapie). – They are routinely found in scrapie (a neurological disease of sheep). PRION HYPOTHESIS • Prions are practically indestructible. – – – – – They can withstand cooking. They can withstand autoclaving. They are resistant to strong alkali treatment. They are resistant to disinfectants. They can survive in soil for years. • Inactivation requires autoclaving in an alkali solution (bleach containing 2% chlorine) for one hour. TSE • Infective prions can be ingested with prioncontaining material. • These prions can move through the intestinal wall rapidly and enter lymph nodes where they incubate – They are picked up by peripheral nerves and moved to the spinal cord and brain. • Infectious prions can be transmitted between species – Incubation time is significantly longer when they cross between species. TSE • Prions produce transmissible spongiform encephalitis (TSE). – – – – – It is a neurodegenerative disease. It can affect cattle and humans. There is no test for it in live organisms. There is no treatment. There is no cure. TSE • Symptoms include: – – – – – – Lack of coordination Staggering Slurred speech Dramatic mood swings Paralysis Death within one year of symptom onset TSE • “Mad cow” disease was first seen in Britain in 1984 – By the year 2000, there were 180,000 confirmed cases in cattle in Britain. • The infection in cattle has been attributed to sheep brain supplement included in cattle feed. • First human case documented in Britain was in 1996. – To date, there have been more than 120 cases documented in humans. • Estimates of the number of new cases in the next few decades vary from a few hundred to 150,000. SUPERBUGS An intro to bacteria, infectious diseases, and antibiotic resistance How abundant are bacteria? Bacterial Abundance Total bacteria on Earth Number of stars in the universe Age of the universe in seconds Bacteria in the human gut 5 x 1030 7 x 1022 4.4 x 1017 1 x 1014 Cells in the human body Texts sent in 2009 People on Earth 1 x 1013 1.5 x 1012 6.9 x 109 Introduction • Since the first use of antibiotics in the 1930s and 1940s, bacteria quickly adapted and developed mechanisms to escape their effects • Over the following decades, new antibiotics were developed to overcome resistance • Since the 1990s, new antibiotic development has fallen sharply while bacterial resistance continues to increase • Antibiotic resistance is responsible for countless human deaths and billions of dollars in healthcare expenses Introduction Resistance Beyond Typical Bacteria • Imidazole-resistant Candida spp. • Multidrug-resistant tuberculosis • Multidrug-resistant malaria • Anti-viral resistant influenza • Multidrug-resistant E. coli Antibiotic Use Leads to Antibiotic Resistance Inpatient Agriculture Outpatient Reasons for Antibiotic Overuse : Conclusions from 8 Focus Groups Patient Concerns • Want clear explanation • Green nasal discharge • Need to return to work Physician Concerns • Patient expects antibiotic • Diagnostic uncertainty • Time pressure Antibiotic Prescription Barden L.S. Clin Pediatr 1998;37:665 Antibiotic Use Leads to Antibiotic Resistance • Resistant bacteria or their genetic determinates are selected when colonizing or infecting bacteria are exposed to antibiotics • Resistant bacteria can then be transmitted between patients • Highest risk patients: – Immunocompromised – Hospitalized – Invasive devices (central venous catheters) Mechanisms Of Antibiotic Resistance • Bacteria are capable of becoming resistant through several mechanisms • One or many mechanisms may exist in an organism • Multidrug-resistant bacteria often have multiple mechanisms • Genes encoding resistance may exist on plasmid or chromosome Decreased Permeability Alteratio n in Target Molecule Community-Acquired Resistant E. Coli • Mostly UTIs • Young healthy women in addition to the elderly • 10-20% now resistant to fluoroquinolones • 30-50% resistant to trimethoprimsulfamethoxazole • CTX-M β-lactamases becoming more common – Cause cephalosporin resistance Antimicrobial Therapy Appropriate initial antibiotic while improving patient outcomes and heathcare Unnecessary antibiotics and adverse patient outcomes and increased cost A Balancing Act What is Antimicrobial Stewardship • Antimicrobial stewardship involves the optimal selection, dose and duration of an antibiotic resulting in the cure or prevention of infection with minimal unintended consequences to the patient including emergence of resistance, adverse drug events, and cost. Ultimate goal is improved patient care and healthcare outcomes Conclusion • Inappropriate and excessive use of antibiotics is a major factor contributing to emerging antibiotic resistance • Determinants of resistance are selected for by antibiotic use • Multiple mechanisms exist for bacteria to become resistant to antibiotics • Antibiotic resistance is a problem in outpatient and inpatient settings and is a factor in a wide variety of infections • Antibiotic resistance continues to emerge as a serious threat to public health The Global Threat of Epidemic Infectious Diseases Projected Global Trends • Asian countries will lead in economic growth • Asian Cities will lead in population growth Circular rural to urban migration • Increased globalization Increased trade Increased movement of people, animals and commodities Increased movement of pathogens • Increased probability of epidemic disease • Increased threat to global economic security Examples of recent emerging diseases Source: NATURE; Vol July CHATURVEDI 2004; Dr. 430; KANUPRIYA www.nature.com/nature Transmission of Infectious Agent from Animals to Humans • >2/3rd emerging infections originate from animalswild & domestic • Emerging Influenza infections in Humans associated with Geese, Chickens & Pigs • Animal displacement in search of food after deforestation/ climate change (Lassa fever) • Humans themselves penetrate/ modify unpopulated regions- come closer to animal reservoirs/ vectors (Yellow fever, Malaria) • Eco-Tourism Live Animal Importation into the USA - 2002 • 47,000 mammals 28 species of rodents • 379,000 birds • 2 million reptiles & Poisonous snakes • 49 million amphibians • 223 million fish Data from U.S. Fish & Wildlife Service Exotic Infectious Diseases That Have Recently Been Introduced to the US • • • • • • • • • West Nile Fever Dengue Fever Yellow Fever Mayaro Fever Chikungunya Epidemic Polyarthritis SARS Influenza Lassa Fever • • • • • • • • • • Monkeypox CJD/BSE HIV/AIDS Cholera E. coli O157 E. Coli 0104:H4 Malaria Leishmaniasis Chagas Disease Cyclospora Pathogens of Tomorrow From Whence They Will Come? From Asia From Animals Mostly Viruses 94 95