* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download I. Oral sustained release system
Survey
Document related concepts
Transcript
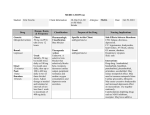
A REVIEW ARTICLE AN ANTIHYPERTENSIVE METOPROLOL SUSTAINED RELEASE DRUG S.Ashutosh Kumar*1, S.Manidipa1, Dr. Y. Indira Muzib2, Dr. J.V.L.N.Seshagiri Rao3, Dr.V. Raghu Murthy4 1. A.K.R.G College of Pharmacy, Nallajerla, West Godavari, 534112 2. Institute of Pharmaceutical Technology, Sri Padmavati Mahila Visvavidyalayam, Tirupati, A.P 3. AU College of Pharmaceutical Sciences, Andhra University, Visakhapatnam, A.P 4. S.V Government Polytechnic, Tirupati, A.P Author for Correspondance:[email protected] 1. INTRODUCTION There are several forms used interchanged viz controlled release, programmed release, sustained release, prolonged release, timed release, slow release, extended release and other such dosages forms. The goal of any drug delivery system is to provide a therapeutic amount of drug to the proper site in the body to achieve promptly and then maintain the desired drug core. It is for this reason that the science and technology responsible for development of sustained release pharmaceuticals has been, and continues to be, the focus of a great deal of attention in both industrial and academic laboratories. 1 The history of Sustain Release technology can be divided roughly into 3 time periods. From 1950 to 1970 in the period of sustained drug release a number of systems containing hydrophobic polymers and very wire fabricated with drugs into dosage forms with the aim of sustaining drug levels and hence drug action for an extended period of time. The period of 1990 to 1990 was involved in the determination of the needs in controlled drug delivery and to understand the barriers of various routes of administrations. Post 1999 in the modern era of sustained release dosages forms (Sustained Release drug delivery technology). Now currently there are numerous products as market formulated for both oral and parentral routes of administration. DEFINITION Sustain Release systems include any drug delivery system the achieve slow release of drug over an extended period of time. Sustained drug action of a predetermines rate by maintaining a relatively constant, effective drug level in the body with concomitant minimization of undesirable effects. ADVANTAGES 1. Improved patient convenience 2. Improved patient compliance 3. Less frequency of drug administration 4. Reduce in fluctuation in steady state level 5. Better control disease condition 6. Reduced intensity of local or systemic side effects. 7. Increased equal safety margin 2 8. Maximum utilization of drugs 9. Reduction in health care costs through improve therapy 10. Shorter treatment period DISADVANTAGES 1. Decreased systemic availability 2. Poor in vitro-in vivo correlation 3. Possibility of doses dumping 4. Retrieval of drug in difficult in case of toxicity poisoning on hypersensitivity reactions 5. Higher cost of formulation. RESULTS Reduced side effects TYPES 1. Oral 2. Parental I. ORAL SUSTAINED RELEASE SYSTEM 1. Continuous release systems 1. Dissolution SR system 2. Diffusion SR system 3. Dissolution and diffusion SR system 4. Ion exchange resin drug complexes 5. Slow dissolving salts and complexes 3 6. Patient dependent formulations 7. Osmotic pressure controlled system 8. Hydrodynamic pressure controlled system 2. Delayed transit and continuous release systems 1. Altered density system 2. Mucoadhesive system 3. Size based systems 3. Delayed release system 1. Intestinal release system 2. Colonic release system II. PARENTRAL SUSTAINED RELEASE SYSTEMS 1. Injectables 1. Solutions 2. Dispersions 3. Microspheres and Microcapsules 4. Nanoparticles and Niosomes 5. Liposomes 6. Released erythrocytes 2. Implants 3. Infusion devices 1. Osmotic pumps 2. Vapour pressure powered pumps 4 3. Battery powered pumps. GUIDELINE FOR DESIGN AND DRUG RELEASE PATTERN OF SUSTAINED RELEASE DRUGS/ SR DOSAGE FORMS Formulation Factors Formulation factors includes - Chemical nature of drug (ester, salts, complex, etc) - Drug solubility in water and organ solvents - Particle size and surface area - Type of dosage forms (solution, suspension, capsule, tablets) - Excipients and process used in the manufacturing of the drug delivery systems Bioavailability is a form which is used to indicate the rate and extent of the administered drug which reacts the systemic circulation intact. If the drug does not flow in the general circulation it cannot be expected to reach the receptor. Hence the absorption into the circulation is an important part of delivery. Hansch made an effect to address this consideration by altering the relatively lipophilicity or hydrophilicity properties of a drug by altering its strucutre some of the delivery properties can also be addressed by the nature of the matrix in which the drug is administered. Excipients any other compound present in the formulation with the drug can also make a difference in drug absorption. The effects of dosage forms an bioavailability depends on the rapidity with which the particular form release the drug into the biological fluids as how rapidly the drug may permeate a membrane 5 (cell membrane). Absorption is most rapid from solutions a decreased in the orders. Most of drugs are taken orally hence stability at stomach patients and taste is important consideration in making the drug acceptable to the patients. Suspensions are rapidly absorbed also, mainly because of the large surface area of the very small particles in the suspension. The smaller the particles size, the better crystal form, Viscosity of the preparation is also important. The rate of absorption of a drug from a capsule can be altered considerably by the interaction of the drug with other medicinal components or diluents (excipients) present in the capsule. The compressed tablets are the most widely used dosage form because of its convenience and because of economic factors in the manufacturing process. Disintegrants have been developed to the point that disintegration is not usually the rate limiting step. The US Pharmacopeia set a time limit of disintegration. The variables which affect the disintegration rate include: Compression force with which the tablet was formed. Particle size Crystalline form Type and concentration of disintegrant Type and concentration of lubricant Methods of incorporating additives Processing of the final formulation Coating tables and several types of coating used 6 - Thin film - Sugar coating - Enteric coating The most unpredictable because such coated tablets may pass through the stomach intact and be released into the intestine at unpredictable intervals all of one time rather than slowly over period of time. Binding agents - Which have adhesive properties are important excipients, especially for lozenges and tablets. The choice of the particular binder or thickening agents is dependent upon the derived properties of adhesive strength and thickness. Surface active agents – (usually termed surfactants) A surfactant in dilute solution moves to the interface of a two phase system and reduces the surface free energy. This permits the two phases to mix more completely. Protection of formulation: Especially eg. Solution against microbial growth and requires use of either antibacterial an antifungal preservatives. Sustained release formulations: are designed to release a drug slowly and the release itself is generally the rate determining step. A drug should be efficiently absorbed over a major portion of the GIT. It should also have a relatively sharp biological half life. Since otherwise it will remain in the biological systemic over long periods of time because of the biological half life itself. Finally it should not have a narrow therapeutic index. 7 FACTORS TO BE STUDIED IN DOSAGE FORM DESIGN The properties of the active ingredients 1. Elimination half life Drugs with long elimination half lives are generally undesirable for prolonged release dosages forms unless designed to prevent toxic effects due to a peaking offered or to reduce the dose. 8 2. The first pass effect Bioavailability may be significantly improved of the release rate is referred for drugs that suffer from an extensive first pass effect. 3. The absorption site If the absorption site is limited absorption is likely to decrease of variable bioavailability with occur for typical prolonged release dosage forms. 4. Adverse reactions Undesirable adverse reaction and may develop by using prolonging drug release. It is desirable to clarify following factors i. Correlation of clinical response with blood drug concentration an tissues concentration at the site of action ii. Induction or inhibition of drug metabolizing enzymes by the prolonged blood concentration casual a large of pharmacological responses and the possibility of tolerance or addiction of the drug. iii. Interactions with other drugs due to protein binding. Pharmacodynamics The major purpose for developing prolonged release formulations of the drug is generally to maintain the blood concentration of the active ingredient of therapeutically effective levels. Therefore it is desirable that average minimum affective concentration and optimal therapeutic concentration be classified for 9 each drug by valuating blood concentration of the active ingredients or therapeutic moietys including active metabolites in relation to drug efficacy. Biopharmaceutics Information on the biopharmaceutical properties of the ingredient for a prolonged release dosage is essential in rational formulation design. Particular attention should be given to the following 6 factors: 1. Location of major absorption sites or specificity in the site of absorption 2. Absorption rate 3. The elimination half life of the drug 4. Whether absorption in non linear due to the saturates drug absorption, first pass effects on other reasons. 5. Whether the elimination is nonlinear due to drug metabolism saturation or other factors. 6. Inactivation or metabolism of the drug in the body, including the GIT. Chemistry and physiochemistry Chemical and physiochemical properties of drugs, especially patient solubility characterized should be clarified. Factors due to physiological condition The release of an active ingredient from prolonged release dosage forms and its absorption are inevitably affected by physiological factors in the HIT. 10 Prolonged release dosage forms are more susceptible to these factors than immediate release dosage forms. Transit characteristics of the dosage form through the GIT The transit rate of a large form through GIT is known to depend on the formulation properties such as size, form, specific gravity and adhesiveness of the properties physiological properties such as the length, size and motility of the GIT: and on the composition and volume of the gastrointestinal content. It is also affected by food, disease, posture and stress. The bioavailability of drugs often depends on gastrointestinal period rate of the dosage forms. Physiology of the GIT The physiological characteristic of the gastrointestinal tract (the volume composition, pH, surface tension, and viscosity of the gastrointestinal content, gastrointestinal motility) vary greatly from site to site. Prolonged release dosage forms remain in the gastrointestinal tract layer the conventional preparations. Prototype dosage forms and selection of the final dosage form i) Duration of appropriate blend drug concentration for a sufficient time with minimal influence of food and physiological conditions of the gastrointestinal tract. ii) Minimal contribution to intra & inter subject variable. To select the best possible dosage forms all candidate forms should be fully tested for release characteristics. 11 DRUG RELEASE PATTERN i) Drug disposition follow first order kinetics ii) The rate limiting step in the absorption is the rate of drug release from the controlled release formulation (ie. Kr < Ka) iii) The release of drug is rapidly and completely based on absorbed Then the four models for drug input based on the drug release pattern can be defined i) Slow zero order release ii) Slow first order release iii) Initial rapid release of loading dose followed by slow zero order release iv) Initial rapid release of loading dose followed by slow first order release EVALUATION OF THE SUSTAINED RELEASE DOSAGE FORM Release characteristics A. Evaluation of the release characteristics The release of the active ingredient from the properties in the GIT is affected by many physiological forces including the mechanical forces extended by the digestive tract in relation to its movement, the volume; composition; pH; surface tension; a viscosity of the GIT. Therefore, in vivo release behaviour should be investigated under as many conditions as possible to understood possible affects of gastrointestinal variables on in vivo release. To achieve stable blood concentration; it is generally desirable to prepare prolonged release 12 dosages forms whose release refers are minimally pH dependent. Therefore, release of the achieve ingredient should be evaluated at multiple levels of patient such as 1:2, 4:0 and 6:8 representing typically gastrointestinal per variations. Considering the variation in gastrointestinal moiety; agitation rate should also vary more than 12 levels among 50, 100 and 250 rpm at an appropriate point. B. Specification for dissolution testing The specification of drug release should be established for quality control of prolonged release dosages forms. The tolerable drug release range change depending on the affect of the release rate an absorption or a release pharmacodynamically properties (therapeutic wireless, toxicity or adverse reactions). Therefore based on the relation between release rate and blood concentration or pharmacological affects, the tolerable range should be set within limits which do not allow great changes in blood concentration are in clinical efficacy. If the relation between the release rate and blood concentration is not clear; or if sufficient data are not available to prove the correlation it is difficult to set rational specification. In such a case this desirable to set specifications using the second method (paddle method) in the Japanese pharmacopoeia at sampling time pints of 2040%, 40-60% more than 70% of the labeled amount of the active ingredient is released. If 100 rpms and 900 ml of test fluid was used for the paddle method the tolerance range at 1st and 2nd and 3rd points should be set within 15%, 15%, 10% of the average release respectively. At the 3rd sample point, only lower limits is acceptable instead of the tolerance range The acceptance criteria of the 13 drug release follow the criteria of dissolution of an release tests of IP XI or USP XXI. C. Stability test Specimens for long form stability tests should be subject to dissolution testing and comply with the standards of the specifications. Pharmacokinetics: A. Comparison of the prolonged release dosage form with an immediate release dosage form As far as possible, the pharmacokinetics of the prolonged release dosage form should be compared with the immediate release products in healthy volunteers. Pharmacokinetic evaluation should be made based on blood concentration data. Data on drug concentration in the urine saliva or other body fluids will be accepted only when the use of the active ingredient in the blood as at the site of active are correlates with that in those fluids. Unless the drug shows linear pharmacokinetics within the clinical dose range, the investigation should be made at two levels, high and low. i. Single dose study The usefulness of the prolonged release dosage form given according to the dosage regimen should be evaluated by comparing the blood concentration with that of the immediate release dosage form an alternative forms such as solution on a powder; or with a prolonged release product which has already been approved when better prolonged release characteristics are claimed. The 14 parameter to be compared are AUC (zero to the final sampling time), AUC (0-), Cmax, the duration of the MEC, or optimal effective use of the active ingredient if these concentration are known as can be estimated. It is desirable to determine the time to reach the MEC or the optimal effective concentration time, absorption rate consistent, elimination rate constant, clearance, extent absorption and MRT and VRT by the moment analysis method. ii. Multiple dose study Prior to a multiple dose study, a blood concentration profile at steady state for multiple doing of both standard and test dosage forms should be stimulated form the single dose pharmaceutical trials. In the multiple dose studies it should be ascertained that Cmax and Cmin at steady these are within the estimated ranges and the usefulness of the prolonged release dosage form the estimated ranges and usefulness of the prolonged release dosage form the estimated ranges and usefulness of the prolonged release dosage form should be evaluated by comparing it with reference product in 1. Cmax 2. Cmin 3. The difference between Cmax and Cmin as the ratio (dosage form index , Cmax/Cmin) and the duration of the MEC or that of optimal effective concentration. B. Effect of dosing conditions and physiological forces Factors which might affect the pharmacokinetics of a prolonged release dosage form should be studied in which food is particularly on my factor because it is know to affect furnish of dosage forms in GIT, disintegration and release of 15 the drug. If significance affects of food was observed a special caution should be included in the dosage regimen and it should be clarified whether the food related product, although the studies are not needed when there is published evidence. It is also desirable to investigate diurnal variation of pharmacokinetic parameters. Clinical efficacy The clinical usefulness of the prolonged release dosage from should be shown comparing it with its already approved immediate release product or is already approved prolonged release product. 3. METHOD AND RESUTLS Establishment of dosing regimen The appropriate dosing regimen should be established during phase I and II clinical studies in which it is recommended that the blood concentration are reinforced during phase II clinical tubes to establish a better dosing regimen. Factors of particular importance in establishing dosing regimen i) Overdose or dose dumping: SR dosage forms might be more likely to produce significant adverse and toxic effects than immediate release dosage forms in case of over dose or dose dumping because of the higher doses of active ingredients which are absorbed over a prolonged time. Dose dumping, e.g. resulting from crushing by the teeth, may be another problem with prolonged release dosage forms. ii) Disease state: The physiological changes in GIT, liver, kidney or heart due to disease often affect absorption, distribution and elimination of drugs and there is 16 a possibility that prolong release doses forms are particularly susceptible to the change. In such cases, the dosing regimen should be studied and established as to reflect the pathological changes. iii) Condition therapy If any other drug is used concurring it may for absorption, distribution and elimination of the drug contained in the prolonged release dosage form. As a result, blood concentration of the drugs which might be used together in practice should be studied, and suitable indications and special warnings for the concurrent case of other drugs should be established. Dosing guidelines Recommendations for dosing conditions, frequency of dosing per day and dose levels (initial dose, maintenance dose, dose adjustment for insufficient response and the maximum tolerance dose) should be established based on the available pharmacokinetics data during phase II clinical studies. The action to be taken if toxic agents / signs or adverse effects develop should also be specified in these guidelines. Detailed drug guidelines including information about dose adjustment based on blood concentration monitoring or changed in renal clearance of each patient may be useful to maximize the therapeutic efficacy by making the utmost use of the advantages of the prolonged release dosage form. It is desired to set up corresponding detailed guidelines particularly for prolonged release products containing 17 A. Drugs, blood concentration of which may along strikingly by minimal changes in dose B. Drugs, the clearance and blood concentration of which are susceptible to physiological conditions age C. Drug, with a narrow therapeutic window and D. Drugs with might cause tolerance and or severe adverse effects. 4. DISCUSSION ANTIHYPERTENSIVE DRUG (Metoprolol) Antihypertensive drug therapy has been remarkably improved in the last 50 years. Different classes of drug have received prominence with passage of time in this period. Before 1950 hardly any effective and tolerated antihypertensive was available. Veratrum and sodium thiocyanate could lower BP but were toxic and difficult to use. The ganglion blokcer developed in the 1950’s were effective but inconvenient. Reserpive was a break through but produces mental depression. The antihypertensive of the 1960-70s were methyldopa, -Blockers, thiazide and high ceiling diuretics and clonidine. The studies of B-Blockers and blocker prazosin broke new grounds. The antihypertensive of 1980-1990s are Angiotensin II converting enzyme (ACE) inhibitors and calcium channel blockers. Angiotensin II antagonists (Losartan) are the latest antihypertensive. General guideline of antihypertension: These are drugs used to lower BP in hypertension systemic arterial B.P. is determined by cardiac output (c.o) and total peripheral resistance (t.p.r). In most 18 of cases, rise in BP is due to increase in t.p.r. while c.o and heart rate (HR) are not high. Hypertension could be is due to increase in t.p.r while long term cardiovascular mortality. The INC VI (1997) and WHO ISH guideline (1999) have define is to be 140 mm Hg systolic and 90 mm Hg diastolic through risk appears to increase even above 120/180 mm Hg. Sustained hypertension 1. Damagers blood vessels in the brain, heart and the kidney 2. Leads to increased incidence of coronary disease renal failure and stroke The urgency of insinuating treatment and risk of end organ damage increases proportionate to the magnitude of blood pressure elevation. Diagnosis It is generally based on repeated, reproducible measurements of elevated B.P. and not on patient symptoms. Patient compliance is a major obstacle to therapy. Classification of high B.P. for adults aged 18 years and older Category Systolic Diastolic Normal < 130 < 85 High normal 130-137 85-89 Hypertension – stage I 140-159 90-99 Stage II 160-179 100-109 Stage III > 180 > 110 19 Diagnosis is based on measurements of elevated B.P. and not on patient symptoms initial screening B.P. (mm Hg) Follow up recommendation Systolic Diastolic < 130 < 85 Recheck in 2 years 130-139 85-89 Recheck in 1 year, provide advice about life style modification 140-159 90-99 Confirm with in 2 months; provide advice about life style modifications 160-179 100-109 Evaluate or refer to source of care within 1 month > 180 > 110 Evaluate as refer to source of case immediately or within one week depending on clinical situations. Treatment 1. The decision to initiate treatment requires consideration of several factors including severity of B.P. elevation and presence of other risk factors. The risks of toxicity form drug treatment must be weighed against the risks of not treating. No single made of treatment is suitable for all patients. 2. Life style modification - If over weight, loss weight - Limit alcohol intake - Reduce sodium, to no more than 2.4 g of sodium / day - Exercise - Stop smoking 20 - Reduce intaking of dietary fat and cholesterol - Dietary approach to step hypertension (DASH) diet. 3. Drugs with different sites of action can be used together most effectively. Drugs with the same mechanisms of action should rarely be combined. Comparative cost for 30 days treatment with commonly Antihypertensives Hydrochlorothiazide 12.5 – 25 mg per daily $ 8.00 Atenolol 50mg per daily $ 18.00 Metoprolol SR 100mg per daily $ 16.00 Acebutolol 200mg per bid $ 25.00 Lisinopril 10mg per daily $ 36.00 Enalapril 10mg per daily $ 42.00 Enalapril 5mg per bid $ 64.00 Felodipine ER 10mg per daily $ 43.00 Diltiazem CD 180mg per daily $ 48.00 21 used CLASSIFICATION 1. ACE inhibitor: Captopril, Enalapril, Lisinopril, Ramipril 2. Angiotensin (AT1) Antagonists: Losartan, Landesartan, Irbesartan 3. Ca+ channel blockers: Verapamil, Nifedipine, Felodipine, Amlodipine 4. Diuretics: i. Thiazide Hydrochlorothiazide, Indapamide ii. High ceiling Furosemide iii. K+ sparing Spironolactone, Amiloride 5. Adrenergic blockers: Propranolol, Metoprolol, Atenolol 6. + adrenergic blockers: Labetolol, Carvediol 7. Adregenic blockers: Prazosin, Terazosin, Doxazosin, Phentolamine, Phenoxybenzamine 8. Central sympatholytics: Clonidine, Methyldopa 9. Vasodilators: i. Arteriolar - ii. Arteriolar + venous - Hydralazine, Diazoxide Sodium nitropruside 22 DRUG METOPROLOL (Lopressor) Metoprolol is used alone are in combination with the medications to treat high B.P. It is also is used to prevent angina (chest pain) and to treat heart attacks. Extended release (long action) Metoprolol also is used in combination with other medication to treat heat failure. Metoprolol is in a class of medications called beta blockers. It works by slowing heart rate and releasing the blood vessels so the heart does not have to pump as hard. Structure CH3 – O – CH2 – CH2 – OH CH3 | | – O – CH2 – CH –CH2–NH–CH–CH3 Metoprolol comes as a tablet and an extended release tablet to take by mouth. The regular tablet is usually taken once or twice a day with meals or immediately after meals. The extended release tablet is usually taken once a day. To help you remember to take Metoprolol, take it around the same time every day. Metoprolol controls high B.P. and angina but does not cure them. Extended release Metoprolol control heart failure but does not cure it. It may take a few weeks before you feel the full benefit of Metoprolol. Continue to take Metoprolol even if you feel well. Metoprolol is also used sometime to prevent migraine headaches and to treat heart beat and movement disorder caused by medications for mental illness. Take the missed dose as soon as you remember it. However if it is almost time for the next dose; skip the missed dose and continue 23 your regular dosing schedule. Do not take a double dose to make up for a missed one. SIDE EFFECTS i) Dizziness or lightheadedness ii) Tiredness iii) Depression iv) Upset stomach v) Dry mouth vi) Stomach pain vii) Gas or bloating viii) Heart burn ix) Constipation x) Rash or itching xi) Cool hands and feets SYMPTOMS 1. Shortness of breath 2. Wheezing 3. Swelling of the hands, feets, ankles and lower legs 4. Unusual weight gain 5. Fainting 6. Rapid irregular heart beat 24 STORAGE CONDITIONS: Keep this medication in the container it came, in tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture. Thrown away any mediation that is out dated or no longer needed. PHARMACOLOGICAL ACTIONS It decreases heart rate, force of contraction and cardiac output. It prolongs systole by regarding conduction so that synergy of contraction of ventricular fibers is disturbed. The effect on a normal resting subjects are not appreciable but become prominent under sympathetic over activity. Cardiac work and oxygen consumption are reduced as the product of Heart rate and aortic pressure decreases. Total coronary flow is reduced, but this is largely restricted to the subepicardial region, while the subendocardial area is not affected. Overall effect in angina patients is improvement of oxygen supply or demand status and exercise tolerance is increased. It block vasodilatation and fall in BP evoked by Isopropanol and enhances the rise in BP caused by Adrenaline there is re-reversal of vasomotor reversal that is seen after - Blockers. It has no direct effect on BV and there is little active change in BP. Some Silent features 1. Low prosperity to cause bronchoconstriction, but even these drugs should be avoided, if possible in asthmatics. 25 2. Lower incidence of cold hands and feets, less chances of precipitating Reynaud’s phenomenon. 3. No / less deleterious affect on blood lipid profile. 4. In effective in suppressing essential tremor 5. Less liable to in favor exercise capacity Mechanism of action It include i) Decrease myocardial contractility and cardiac output ii) Decrease rennin secretion and hence decreases levels of Anginotension II. Preparation and characterization of Metoprolol sustained release solid dispersions. In recent years, great attention has been paid to using solid dispersions to make sustained-release drugs. The objective of this study is to produce sustained-release systems of Metoprolol tartrate using solid dispersion techniques and to evaluate their physicochemical characteristics. The solid dispersions were produced by melting and solvent methods, containing 7%, 15%, or 25% of the drug and different ratios of Eudragit RLPO and RSPO in ratios of 0:10, 3:7, 5:5, 7:3, and 10:0. Drug release profiles were determined by USP XXIII rotating paddle method in phosphate buffer solution (pH 6.8). XRD, DSC, IR, and microscopic observations were performed to evaluate the physical characteristics of solid dispersions. Results showed that the drug release from dispersions was at a slower rate than pure drug and physical mixtures. Moreover, 26 the formulations containing greater ratios of Eudragit RSPO showed slower release rates and smaller DE8% but larger mean dissolution time than those containing greater ratios of Eudragit RLPO. Dispersions with particle size of less than 100 micro containing 7% of Metoprolol and Eudragit RL:RS 5:5 (solvent method) and those with the ratio of 3:7 (melting method) had similar release pattern to Lopressor sustained-release tablets by zero-order and Higuchi kinetics, respectively. Analytical method for the determination of Metoprolol tartarate A kinetic spectrophotometric method has been described for the determination of Metoprolol tartrate in pharmaceutical formulations. The method is based on reaction of the drug with alkaline potassium permanganate at 25+/-1 degrees C. The reaction is followed spectrophotometrically by measuring the change in absorbance at 610 nm as a function of time. The initial rate and fixed time (at 15.0 min) methods are utilized for constructing the calibration graphs to determine the concentration of the drug. Both the calibration graphs are linear in the concentration range of 1.46 x 10(-6)-8.76 x 10(-6) M (10.0-60.0 microg per 10 ml). The calibration data resulted in the linear regression equations of log (rate) = 3.634+0.999 log C and A=6.300 x 10(-4)+6.491 x 10(-2) C for initial-rate and fixed time methods, respectively. The limits of quantization for initial rate and fixed time methods are 0.04 and 0.10 microg ml(-1), respectively. The activation parameters such as E(a), DeltaH(double dagger), DeltaS(double dagger) and DeltaG (double dagger) are also evaluated for the reaction and found to be 90.73 kJ mol(-l), 88.20 kJ mol(-l), 84.54 J K(-1) mol(-l) and 63.01 kJ mol(-l), respectively. The results are validated statistically and through recovery studies. The method has been 27 successfully applied to the determination of Metoprolol tartrate in pharmaceutical formulations. Statistical comparison of the results with the reference method shows excellent agreement and indicates no significant difference in accuracy and precision. Evaluation of the vitro release rate and the vivo absorption characteristics of four Metoprolol tartarate SR tablet formulations The purpose of this investigation was to examine the impact of formulation and process changes on dissolution and bioavailability/bioequivalence of Metoprolol tartarate tablets manufactured using a high-shear granulation process. A half-factorial (2(4-1), Res IV) design was undertaken to study the selected formulation and processing variables during scale-up. Levels and ranges for excipients and processing changes studied represented level 2 or greater changes as indicated by the SUPAC-IR Guidance. Blend and tableting properties were evaluated. Changes in sodium starch glycolate and magnesium stearate levels, and the order of addition microcrystalline cellulose (intra- vs. extra granular) were significant only in affecting percent drug released (Q) in 5, 10, and 15 min. Statistical analysis of data showed no significant curvature. No interaction effects were found to be statistically significant. To examine the impact of formulation and processing variables on in vivo absorption, three batches were selected for a bioavailability study based on their dissolution profiles. Subjects received four Metoprolol treatments (Lopressor, slow-, medium-, and fast-dissolving formulations) separated by 1 week according to a randomized crossover design. After an overnight fast, subjects were administered one tablet (100 mg), blood samples 28 were collected over 24 hr and plasma samples were analyzed. The formulations were found to be bioequivalent with respect to the log C max and log AUCOinfinity. The results of this study suggest that: (i) bioavailability/ bioequivalence studies may not be necessary for Metoprolol tartrate and perhaps other class 1 drugs after level 2 type changes and (ii) in vitro dissolution tests may be used to show bioequivalence of Metoprolol formulations with processing or formulation changes within the specified level 2 ranges for the equipment examined VARIOUS SALT FORMS OF METOPROLOL 1. Metoprolol tartarate 2. Metoprolol succinate Metoprolol tartarate (Lopressor) Metoprolol tartrate is a selective beta adrenoreceptor blocking agent, available as 50- and 100-mg tablets for oral .administration and in 5-ml ampoules for intravenous administration. Each ample contains a sterile solution of Metoprolol tartrate, 5 mg and sodium chloride, 45 mg. Metoprolol tartrate is (+)-1-(isopropyl amino)-3-(p-(2-(methoxyethyl) phenoxy)-2-propanol (2:1) dextro-tartrate salt. Metoprolol tartrate is a white, practically odorless, crystalline powder with a molecular weight of 684.82. It is very soluble in water; freely soluble in methylene chloride, in chloroform, and in alcohol; slightly soluble in acetone; and insoluble in ether. 29 Lopressor Inactive Ingredients: Tablets contain cellulose compounds, colloidal silicon dioxide, D&C red no. 30 Aluminum Lake (50-mg tablets), FD&C blue no. 2 Aluminum Lake (100-mg tablets), lactose, magnesium stearate, polyethylene glycol, propylene glycol, povidone, sodium starch glycolate, talc, and titanium dioxide. Metoprolol succinate (Toprol-XL) Description Metoprolol succinate is a beta-selective (cardioselective) adrenoceptor blocking agent, for oral administration, available as extended release tablets. Toprol-XL has been formulated to provide a controlled and predictable release of Metoprolol for once daily administration. The tablets comprise a multiple unit system containing Metoprolol succinate in a multitude of controlled release pellets. Each pH acts as a separate drug delivery unit and is designed to deliver Metoprolol continuously over the dosage interval. The tablets contain 47.5 mg, 95 mg and 190 mg of Metoprolol succinate equivalent to 50, 100 and 200 nig of Metoprolol tartrate, USP, respectively. Its chemical name is (±) 1-(isopropyl amino)-3-[p-(2-methoxyethyl) phenoxy]-2-propanol succinate (2:1) (salt). Metoprolol succinate is a white crystalline powder with a molecular weight of 652.8. It is freely soluble in water; soluble in methanol; sparingly soluble in ethanol; slightly soluble in dichloromethane and 2- propanol; practically insoluble in ethyl-acetate, acetone, diethyl ether and heptanes. 30 Inactive ingredients: silicon dioxide, cellulose compounds, sodium stearyl fumarate, polyethylene glycol, titanium dioxide, paraffin. 5. CONCLUSION From the above review of Metoprolol we came to know that Metoprolol is the prototype of cardio selective 1 blockers. Its potency to block cardiac stimulation is similar to Propranolol, but nearly 50 times higher dose is need to block induced vasodilatations. Patients who complain of cold hands and feed while an Propranolol do better Metoprolol. First pass Metoprolol was less marked than others but 90% or more was ultimately metabolized before excretion. There was slow and fast hydroxylators of Metoprolol the former may require a lower dose. Side effects of Metoprolol are mild, but precautions and contra indication remain the same as with the other drugs. Metoprolol use to cure the effect of angina patients and improvement of oxygen supply or demand status and increased the tolerance of exercise. It has no direct effect on blood volume and there was little active change blood pressure. Metoprolol was also too less expensive then the other antihypertensive drugs. 6. REFERENCES 1. Preparation and characterization of Metoprolol sustained release solid dispersion, Department of pharmaceutical science, school of pharmacy and pharmaceutical sciences, 2006 Jul-Aug; 13(4): 295-302. 31 2. Validated kinetic spectrophotometric method for the determination of metoprolol in pharmaceutical formulations, Rahman N, Rahman H, Azmi SN, Department of chemistry, Aligarh Muslim University, Aligarh. 3. Evaluation of in vitro release rate and in vivo absorption characteristics of four Metoprolol sustained-release tablet formulations, Rekhi Gs, Eddington ND, Fossler, MJ, Schwartz P, Lesko LJ, Augsburger LL, Dept. of pharmaceutical sciences, School of pharmacy, University of Maryland at baltimore. 4. Notari, Robert E., Biopharmaceutics and Clinical Pharmacokinetics, An introduction, 4th Edition, Marcel Dekker, Inc, New York, 1987. 5. Foye, William O., Lemke, Thomas L., Williams, David A., Principles of Medicinal Chemistry, 4th Edition, Wililams & Wilkins, Baltimore, 1995. 6. Pharmacokinetics and Biopharmaceuticals A definition of terms, J. Phrmacokinet, Biopharm. 1:3 (1973). 7. A. G. Fishburn, An Introduction of pharmaceutical formulation, pergamon press, New York, 1965. 8. Goodman & Gilman (*9th Ed) 9. Katzung 6th ed. 32