* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download the portal vein
Survey
Document related concepts
Transcript
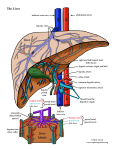
ANATOMY OF HEPATOBILIARY HEPAR • • • • • • • • The largest gland of the body location function lobation segmen attachment counter current flow vessel: porta-systemic anastomosis Introduction The liver • The liver is a pinkish-brown (In life it is reddish brown in) colour • an overall wedge shape "boomerang shaped" organ in the human body • is the largest solid organ (the largest of all is the skin) • Is the largest gland in the human body • In an adult it weighs typically about 2% of body mass (70kg). 1.6 kilograms (3½ pounds) • is about 18 cm (7 inches) across and 15 cm (6 inches) deep at its deepest part -- range : 6-12 cm in percussion at right mic line • medical terms to do with the liver often start in hepato- or hepatic from the Greek hepar for liver. • Several functions • • • • • Formation of bile When the red cells of the blood become worn out they are destroyed by the cells of the reticuloendothelial system In this process bilirubin is formed, and this is carried by the blood to the liver. Together with several other substances it is secreted by the liver as bile. The circulation of blood in the liver is so arranged that very large volumes of blood come into close contact with the cells of the lobules. The cells are thus in a favorable position both to absorb materials from the blood and also secret materials into it. This they do all the time, for the real task of the liver is to maintain in the blood the correct concentrations of many of its constituents. Hepatocytes carry out most of the tasks attributed to the liver, but the phagocytic Kupffer cells that line the sinusoids are responsible for cleansing the blood Gall bladder Vesica fellea • A pear-shaped organ, 7 to 10 cm long, capacity 3050 ml • lies just below the right lobe of the liver in a hollow under the liver • is attached to the visceral surface of the liver by the cystic duct. • The main function of the gall bladder is to store the bile that is secreted by the liver,and is concentrated by the reabsorption of water from it. • the bile travels to the gall bladder along the common hepatic duct • When fatty food is digested, the gall bladder contracts, under the action of the hormone cholecystokinin, thus delivering bile through the common bile ducts (choledochus) to the small intestine where it is able to help dissolve fats • The bile duct and the pancreatic duct enter it together on its posteromedial surface a little below middle of part 2 of duodenum (descendens part) at papilla duodeni major (ampula hepatopancreatica Vatteri. The most common disorder of the gall bladder is gallstones (cholelithiasis), which are composed of cholesterol crystals or pigment material topography • The liver lies in the upper right part of the abdominal cavity. • It occupies most of the right hypochondrium and epigastrium, although it frequently extends into the left hypochondrium as far as the left lateral line. • The narrow end of the wedge lies towards the left hypochondrium, with the anterior edge pointing anteriorly and inferiorly. • The superior and right lateral aspects are shaped by the anterolateral abdominal and chest wall as well as the diaphragm. • The inferior aspect is shaped by the adjacent viscera. • and although firm and pliant its weight and texture depend in part on the volume of venous blood it contains. Anatomy of the Liver • The liver is situated mostly in the top right portion of the abdominal cavity just under the diaphragm. • It can be felt as a hardish mass just below the bottom right rib. liver projection to the anterior Abdomen wall Liver ligaments • It is connected to the diaphragm and abdominal walls by five ligaments: the membranous falciform (which also separates the right and left lobes), coronary, right and left triangular ligaments, and the fibrous round (teres) ligament (which is derived from the embryonic umbilical vein). HEPATIC LOBATION Anatomis (4lobus) Right lobe (terbesar) Left lobe Quadrate lobe (lig. Teres hepatis dan veseca fellea) Caudate lobe (Vena cava inferior, lig. Venosum, dan porta hepatis) • • • • • • • • • • The liver is divided by the 'principal plane' into two halves of approximately equal size. The principal plane is defined by an imaginary parasagittal line from the gallbladder anteriorly to the inferior vena cava posteriorly. The usual functional division of the liver into right and left lobes lies along this plane. The liver is further subdivided into segments, each supplied by a principal branch of the hepatic artery, portal vein and bile duct. Segments I, II, III and IV make up the functional left lobe, and segments V, VI, VII and VIII make up the functional right lobe. The right lobe can be further divided into a posterior and anterior section or sector. The right posterior section is made up of segments VI and VII, and the right anterior section is made up of segments V and VIII. The left lobe can also be divided into sections: segment IV is referred to as the left medial section, and segments II and III as the left lateral section. The hepatic veins lie in liver parenchyma between the sections. Segment I corresponds to the gross anatomical caudate lobe and segment IV to the quadrate lobe. surgical 8 segments (cabang, v hepatica, vena porta (Couinad)a. Hepatica,drainase biliaris (Healey and Schroy) SEGMENTS IN LIVER • • • • • • • • • I II III IVa IVb V VI VII VIII caudate / spigel lobe left posterolateral segment left anterolateral segment left superomedial segment left inferomedial segment right anteroinferior segment right posteroinferior segment right posterosuperior segment Right anterosuperior segment • • • • • • • • • • • Segmentation of the liver - Couinaud. The segments are sometimes referred to by name – I, caudate (sometimes subdivided into left and right parts); II, lateral superior; III, lateral inferior; IV, medial (sometimes subdivided into superior and inferior parts); V, anterior inferior; VI, posterior inferior; VII, posterior superior; VIII, anterior superior. Although a variety of definitions have been used to describe the anatomy of the liver segments, the most widely accepted clinical nomenclature is that described by Couinaud (1957), and Healey and Schroy (1953). The internal architecture of the liver is divided into segments, commonly referred to as Couinaud's segments. Couinaud based his work on the distribution of the portal and hepatic veins whilst Healey and Schroy studied the arterial and biliary anatomy. HEPATIC VESSELS • The vessels connected with the liver are: – The portal vein – The hepatic artery proper – The hepatic veins vascularisation 25 Liver Blood flow • The liver receives blood from two sources. • Oxygenated blood is supplied in the hepatic artery, a branch of the celiac trunk from the abdominal aorta. • Venous blood from the entire gastrointestinal tract (containing nutrients from the intestines) is brought to the liver by the hepatic portal vein. On reaching the liver the portal vein divides into thousands of which pass in between the lobules and terminate in the sinusoids. The blood leaves the liver via a central vein in each lobule, which drains in the hepatic vein. The central canal is a blood vessel in the middle of each lobule which receives blood from the hepatic portal vein and hepatic artery via the sinusoids and drains the blood into the hepatic vein Truncus celiacus Truncus coeliacus HEPATIC ARTERY & ITS BRANCHES • Divide and subdivide in the liver • Smaller rami being associated with those of the portal vein with which they are distributed • There are NO ANASTOMOSIS between their territories; each is END-ARTERIES HEPATIC ARTERY & ITS BRANCHES • A blood vessel which supplies the liver with oxygenated blood • Supplies 20% of the liver’s blood Truncus celiacus dipercacabangkan aorta abdominalis (V.TH 12), mempercabangkan a. gastrica sinistra, a. hepatica communis dan a.lienalis. a.hepatica communis datang di cranial pars superior duodeni, bercabang a. gastrica dextra (ke curvature minor), a. hepatica propria (ke porta hepatica, rr. Dexter, rr sinister dan a. cystica) dan a. pancreaticuduodenalis (yang bercabang menjadi a. pancreaticoduodenalis superior dan a. gastroepiploica dextra, ke curvatura major, oral, beranastomosis dengan a. gastroepiploica sinistra HEPATIC VEINS • Convey the blood from the liver to inferior vena cava • Have a thin tunica adventitia; binding them to the wall of their canals within the liver 36 THE PORTAL VEIN • Supplying most of the blood to the liver (supplies 80% of the liver’s blood) • Formed posterior to the neck of pancreas by the union of – The superior mesenteric vein – The splenic vein THE PORTAL VEIN • The main channel of the portal system of veins • Collects blood from the abdominal part of the GI tract The gallbladder The pancreas The spleen Vena porta hepatis THE PORTAL VEIN • At the right end of the porta hepatis, the portal vein terminates by dividing into right and left branches, each of which supplies about half of the liver Portocava anastomosis ZONES • ZONE 1 – Immediately surrounding the portal triad – The first to get exposed to toxins from portal blood • ZONE 2 • ZONE 3 – Closest to terminal hepatic venule – Gets the least oxygenated blood 47 CELLS OF THE LIVER • • • • • • Hepatocyte Perisinusoidal (Ito) cells Endotheliocytes Macrophages (Kupffer cells) Lymphocytes (pit cells) The cells of biliary tree (cuboideal to columnar epitheliocytes • Connective tissue cells of capsule and portal tracts PORTAL TRIAD • CONSIST OF : – BILE DUCT – HEPATIC ARTERIOLE – PORTAL VENULE, the largest structure (histologically) in the triad COUNTERCURRENT FLOW • BLOOD-FLOW • BILE-FLOW BLOOD-FLOW • Portal vein portal triad portal venule terminal hepatic venule central venule central vein hepatic vein • Zona 1 zona 3 BLOOD-FLOW • Hepatocytes closest to portal triad – receive the most oxygenated blood – Specialized for drug detoxification – most susceptible to damage from drug toxicity BLOOD-FLOW • Hepatocyte closest to the terminal hepatic venule – Receive the least oxygenated blood – Specialized for bile production – Most susceptible to damage in the event of hypoxia BILE - FLOW • Central venule bile duct hepatic duct bile canaliculus portal triad common bile duct • Zona 3 zona 1 PORTAL - SYSTEMIC ANASTOMOSIS • The portal venous system communicates with the systemic venous system • Important clinically • Portal circulation obstructed, blood from GI tract can still reach the right side of the heart through IVC via collateral routes Vena porta hepatis PORTAL SYSTEMIC ANASTOMOSIS • The portal veins and its tributaries have no valves • In portal hypertension – Venous pressure in portal venous system increased – Blood in portal venous may reverse its direction – Blood pass through portal-systemic anastomosis into the systemic venous system – Causes the vein in portal-systemic anastomosis areas to dilate and tortuous and called varicose vein PORTAL - SYSTEMIC ANASTOMOSIS AREA • • • • In the gastroesophageal region In the anorectal region In the paraumbilical region In the retroperitoneal region PORTAL - SYSTEMIC ANASTOMOSIS AREA • Esophageal tributaries of the left gastric vein anastomose with the esophageal veins, which empty into the azygos vein • The superior rectal veins anastomoses with the middle and inferior rectal veins, which are tributaries of the internal iliac and internal pudendal veins, respectively PORTAL - SYSTEMIC ANASTOMOSIS AREA • The paraumbilical veins in the falciform ligament anastomose with subcutaneous veins in the anterior abdominal wall • Tributaries of the splenic and pancreatic veins anastomose with the left renal vein VARICOSE VEIN • Anal region are called hemorrhoids • Gastroesophageal esophageal varices • Paraumbilical caput medusae – Like small snake under the skin – Its resemblance to the serpents on the head of Medusa, a character in Greek mythology Common way to reducing portal pressure • Portocaval anastomosis – Creating a communications between the portal vein and the inferior vena cava • Splenorenal anastomosis – Join the splenic vein to the left renal vein, following removal of the spleen (splenectomy) PORTAL HYPERTENSION • In the normal system, blood is delivered to the liver via : – The hepatic artery (400 ml/minute) – The portal vein (1000 ml/minute) • Normally, blood from all of the gastrointestinal organs come through the liver to be processed PORTAL HYPERTENSION • In the portal hypertension, there is a medical blockage in the liver, due to : – Cirrhosis – Scarring – Hepatitis – Sarcoidosis PORTAL HYPERTENSION • This blockage causes : – the incoming low pressure blood to ‘back up’ • because the blood does not have the pressure to overcome the elevated pressure in the portal vein PORTAL HYPERTENSION • The result is distended veins throughout the GI system : – Hemorrhoid – Varices – Caput medusae – Leakage of fluid into the peritoneum • Ascites • Edema 73 74 Ascites • from Greek askites, "baglike“) • is a gastroenterological term for an accumulation of fluid in the peritoneal cavity. • The medical condition is also known as peritoneal cavity fluid, peritoneal fluid excess, hydroperitoneum or more archaically as abdominal dropsy 75 lobulus 77