* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Surrey Supervised Consumption Scheme Operational Policy March
Survey
Document related concepts
Transcript
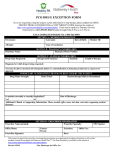
Surrey Supervised Consumption Scheme Operational Policy March 2010 1 CONTENTS Page 3 Contacts Page 4 Introduction Page 7 Guidelines for participating in the scheme Page 8 Shared Care Partners Page 9 Roles and Responsibilities Page 10 Guidelines to the Shared Care Contract Page 11 Sample Shared Care Contract Page 12 Supervised Consumption Procedure – Prescriber Role Page 13 Sample Prescription Page 14 Supervised Consumption Procedure – Pharmacist Role Page 18 Monitoring, Evaluation and Audit Page 18 Other Pharmaceutical Issues Page 21 Health & Safety Page 22 Termination of contract between pharmacist and patient Page 23 Appendix 1 – Remuneration for Pharmacists Page 24 Appendix 2 – Community Pharmacy Contract Page 25 Appendix 3 – Record Form Page 26 Appendix 4 – List of medication for supervision Page 27 Appendix 5 – Harm Reduction and Drug Treatment Page 29 Appendix 6 – Monitoring, Evaluation and Audit Page 30 Appendix 7 – Advice for Locum Pharmacists 2 Contacts Surrey PCT Susie Dadlani Substance Misuse Manager Surrey PCT Ana Rodriguez Substance Misuse Administrator Surrey Harm Reduction Outreach Team Parkview Centre for the Community Blackmore Crescent, Sheerwater, Woking, Surrey, GU21 5NZ Tel: 01932 355533 Fax: 01932 350963 Contract and Paperwork All contracts and paperwork should be returned to: Surrey Supervised Consumption Scheme Manager The Outreach Team Parkview Centre for the Community Blackmore Crescent Sheerwater Woking Surrey, GU21 5NZ 3 INTRODUCTION The Supervised Consumption Scheme In April 1999, the Department of Health published ‘Drug Misuse and Dependence – Guidelines on Clinical Management’ which was circulated to all UK GPs. This followed government white papers and health service guidance emphasising the importance of primary care professionals in the care of drug users. Included in the guidelines is the recommendation that patients should initially be supervised consuming their daily methadone at the point of dispensing, which has meant a greater involvement for pharmacists. ‘the traditional boundaries that enclosed health care professionals have been broken down. The future is clearly about co-operation between health professionals to ensure that the public receives the highest standards of care’. (Royal Pharmaceutical Society of Great Britain – Annual Report 1999) Currently these guidelines are for those pharmacists who are willing to supervise the consumption of methadone, buprenorphine or buprenorphine/naloxone whilst working in conjunction with the patient, the prescriber and the key worker. The Scheme may expand to include other medication at a later date to separate specific contracts. (See Appendix 4) THIS POLICY WILL BE REVIEWED ANNUALLY The Scheme is intended as a more closely monitored course of treatment aimed at immediate harm reduction with the ultimate goal of abstinence wherever possible. The improvement in communication and working relations between professionals will provide further support for the treatment programme within shared care arrangements. Every effort is being made to make process as ‘trouble-free’ as possible for the prescriber/key worker and the pharmacy team. The PCT will contract with the pharmacy contractor to provide supervised consumption for a period of 12 months (or part thereof) from the start of each financial year. The pharmacist will receive payment for each supervised dispensing at the flat rate set by the PCT (see Appendix 1 for further details). Remuneration will be for recognition of the involvement of the professional parties in the project. Pharmacists will undertake to provide 13 weeks supervised self-administration for each patient. Supervision can be longer if all parties continue to be assured that treatment is progressing. Supervised consumption of methadone, buprenorphine or buprenorphine/naloxone is only one aspect of harm minimisation strategy. Patients will be calling into the pharmacy every working day – this service should therefore be as discreet as possible and the patient be treated with respect and courtesy. This will also help to increase a patients ‘sense of worth’ and improves the chance of a successful outcome. Patients given methadone, buprenorphine or buprenorphine/naloxone to take away cannot always be relied upon to consume it. Doses can end up being shared or sold on the black market. Supervised consumption is seen as one way round this problem. It is important that once a patient is stabilised, they are trusted to accept a degree of 4 responsibility by extending treatment to the introduction of ‘take home’ doses, for example, from daily to twice weekly. The pharmacist should accept that supervision might need to be re-instated in times of crisis or relapse and should not consider this as failure of the programme. An optimised Methadone Service The National Treatment Agency for Substance Misuse has highlighted four crucial elements for an optimum methadone service from an evidence base: Adequate doses following proper individualised assessment are important. Daily doses of 60mg to 120mg have been shown to be effective Services with adequate supervision and monitoring of patients including care planning and supervised consumption (during initial stages or periods of instability) are more effective in reducing harm and improving outcome Services that strongly encourage involvement on psycho-social services have better outcomes Services with competent staff who can develop positive relationships with patients have better outcomes. NTASM: Injectable heroin (and injectable methadone). treatment. Executive Summary May 2003. Potential role in drug Government recommendations acknowledge that patient compliance with the programme is an important issue in substance misuse treatment. Non-compliance with treatment may lead to: Increased heroin use with associated risks for the patient, particularly overdose Leakage of methadone, buprenorphine or buprenorphine/naloxone into the illicit market. The issue of leakage of methadone, buprenorphine or buprenorphine/naloxone into the illicit market is one of serious concern. Methadone is dangerous in overdose and it has been suggested that opiate overdoses are not always from people in treatment. It is in the nature of drug dependence that many drug users find control of their drug use difficult. For these people, daily supervision goes some way towards resolving this problem and restricts supply of illicitly bought drugs. It has shown that systematically linking incentives (in the form of relaxations in instalment dispensing) to objective signs of progress may lead to increased stability and reduced illicit drug use. In implementing this service, it must be recognised that this is a measure not considered appropriate for the treatment of other conditions and must be implemented on a clinical rather than moral basis. These guidelines form the basis of a Scheme to pay community pharmacists for supervising the daily consumption of methadone, buprenorphine or buprenorphine/naloxone in Surrey. Pharmacists applying for payment under the Scheme are required to comply with these procedures. Please note that nothing in these guidelines changes the legal position of pharmacists to, at all times, work within the requirements of the Misuse of Drugs Act (1971) and any subsequent legislation. 5 The Provision of supervised Consumption The Surrey Drug Action Team (DAT) fully supports the supervised self-administration of methadone, buprenorphine or buprenorphine/naloxone within community pharmacy premises. Pharmacists can choose whether to participate in the Scheme, as it is optional, and should discuss the Scheme and this document with staff and locums, before entering the programme. It is essential that the programme remains consistent and that all those involved are committed to its goals. Through regular contact, pharmacists can build relationships with patients, encourage stable use of methadone, buprenorphine or buprenorphine/naloxone and give verbal affirmation and feedback appropriate information to partners on the programme. Confidentiality Confidentiality and discretion are crucial factors in the programme. The RPSGB Medicine, Ethics and Practice guidance states; ‘Consideration must be given to providing adequate privacy in the pharmacy for patients self-administering medicines.’ If there is no ‘quiet’ area, this must be explained to the patient, who can then decide whether to nominate an alternative pharmacy. Only in extreme circumstances, as a temporary measure, should supervision take place in the dispensary. Should a patient within the Scheme request other services, particularly needles/syringes, the right of patient confidentiality must be respected. Remember, this programme is based on harm reduction. Such a request provides an ideal opportunity to raise the risk of overdose – made more likely due to the patient’s use of mixed substances. Patients should not be made to feel judged by any member of staff as this could impede the effectiveness of the programme (see also page 7). Should a patient ask to see your confidentiality policy, you will need to be aware of where to locate relevant paperwork. All staff should be aware of the sensitive nature of this treatment and the need to make the patient feel safe about privacy. Information is passed on purely on a ‘need to know’ basis to others involved in the programme (see Caldicott Report, 1997). 6 GUIDELINES FOR PARTICIPATING IN THE SCHEME Pharmacists who agree to take part in this extra service will be required to sign an annual contract with the PCT, committing them to run the project in accordance with this policy. The agreement will run from April – March and will be for 12 months (or part thereof if joined after beginning of the year). Whilst this document covers all the procedures for taking part in the Scheme, each pharmacy should have its own specific standard operating procedure for the Scheme, an example of which is in the information file. Aims To improve consistency and quality of care to the patient To achieve stability and harm reduction To reduce the risk of ‘leakage and spillage’ of drugs liable to misuse into the community To ensure, as far as possible, only the patient consumes the product doses To promote positive contacts with treatment services To improve communication between prescriber, key worker and the pharmacist To reduce the risk of drug related death. Pharmacists signing the PCT agreement will be required to take part in training offered by the PCT and to have completed or be undergoing the named CPPE distance learning pack (ref: Training section). 7 SHARED CARE PARTNERS ‘Shared Care’ refers to the process of treatment of a patient, which includes a number of professionals responsible for the medication and care package. Government guidelines (1999) suggest ‘Shared Care’ is characterised ‘…by an enhanced information exchange beyond routine discharge and referral letters’. All people involved in ‘Shared Care’ are referred to as ‘partners’ and can consist of: The patient The pharmacist The prescriber The key worker Other relevant professionals. Permission should always be obtained from the patient prior to any partners entering into discussion with another partner. This should be in the form of a signed confidentiality waiver (ref: contract). Patients come into daily contact with the pharmacist, which allows for health promotion advice to be given and the monitoring of patient compliance/stability. The agreement about supervised consumption of methadone, buprenorphine or buprenorphine/naloxone seeks to develop for pharmacists a more formal role in monitoring and review of methadone patients. It is difficult to give hard and fast rules about what should be discussed with the prescriber/key worker. The decision is a professional one, which should be made after considering the risk to the patient of non-disclosure and the damage that may be done to the supportive relationship between the pharmacists and the patient. Examples of feedback are: Patient attends irregularly Patient’s general well-being appears to have improved/deteriorated Patient does/does not consume the whole dose under supervision Patient appears intoxicated (patients stabilised on methadone should be alert and coherent) Patient on a titrating dose at the start of a supervised script fails to collect one dose. (The increased dose designated for the next day may be enough to risk accidental overdose) Patient on a stable dose fails to collect up to three consecutive doses of methadone/buprenorphine or on several occasions over a period of weeks (missing doses may result in a drop in opiate tolerance with an increased risk of accidental overdose) There are problems concerning the prescription, e.g. ambiguity of dates for dispensing 8 ROLES AND RESPONSIBILITIES The patient, prescriber, key worker and pharmacists agree to the following: To treat people as individuals and accord them respect To empower to make informed choices To only discuss items relevant to them. They are bound by their own professional codes of ethics to maintain this confidentiality To ensure any written records are securely stored and that the Data Protection Act covering computerised records is adhered to: Data collection will be anonymous (according to the National Drug Treatment Monitoring System) to ensure individual patients cannot be identified To endeavour to ensure that prescriptions and prescribed medications are correct and available at the proper time, providing patients attend appointments at the correct time. Pharmacists To fully respect the patients right to confidentiality To keep any personal details in a secure place To ensure all staff treat the patient with dignity and respect To explain the arrangements for when the pharmacy is closed To explain the ‘house rules’ of the pharmacy e.g. no dogs allowed/collection times To order and prepare (whenever possible) medication in advance To not keep the patient waiting unnecessarily for medication To ensure that medication is only dispensed to the patient To dispense according to the prescription e.g. missed doses cannot be dispensed at a later date To discreetly supervise consumption (e.g. no calling out your name/address) To ensure that the patient is correctly identified To provide drinking water before and after medication has been consumed To prepare all doses in suitable containers and ensure the lids are sealed To feedback to the key worker/prescriber on attendance and well-being To advise, if asked, of feedback given to your key worker/prescriber To provide details of needle exchange outlets in confidence To explain the complaints procedure To maintain full PMR records for each patient To explain that if three consecutive doses are missed, the prescriber/key worker will be contacted to determine whether or not to continue to supply To ensure all paperwork is returned to the Scheme Co-ordinator (Susie Dadlani). The Prescriber/Key Worker To complete the initial assessment and initiate a programme treatment To ensure that the patient has nominated a pharmacy that is willing to participate in the Scheme To complete the relevant paperwork, which form the Scheme To liaise with the pharmacist on the patients behalf To confirm the patient is registered with a GP. 9 GUIDELINES TO THE SHARED CARE CONTRACT There will be four copies of the contract for each patient. The prescriber/key worker will complete the patient’s name and the name of the pharmacy from which the patient will collect his/her methadone, buprenorphine or buprenorphine/naloxone The prescriber/key worker will discuss the contents of the contract with the patient at the first consultation The patient and the prescriber will then sign the contract. The prescriber/key worker will then remove the top copy to keep on file The remaining three copies of the contract will be sent by post to the pharmacy. If there are time constraints, the patient may deliver the contract. The pharmacist will discuss relevant details with the patient and sign the contract The pharmacist will keep one copy on file and give one copy back to the patient The pharmacy copy of the contract should be kept in this procedure manual, for easy reference, stored in alphabetical order. Ensure the name is clear and, when appropriate, include on the contract, the date the supervision has started and stopped. The contract should be stored in a secure place The pharmacist will send one copy of contract to the supervised consumption coordinator (Susie Dadlani), in order for payment to be arranged. (Please ensure all details are clearly readable on this copy) For a patient who has preciously received a contract and is presenting a new prescription, it may be worth reminding the patient of the agreement and asking if they would like anything explaining again. Another copy of the patient information leaflet can be given if appropriate. 10 SHARED CARE CONTRACT I, the patient named below, understand and agree to the following conditions of treatment: 1. I will be prescribed methadone mixture, buprenorphine (Subutex) or buprenorphine / naloxone (Suboxone) (delete as appropriate) for daily supervised consumption at an initial dose of …………………………………………………….. Special Instructions: ……………………………………………………………………… 2. I will collect my prescription in person from the pharmacy named below, at the time arranged between the pharmacist and myself 3. I will see my key worker/prescriber on a regular basis and keep all my appointments unless previously agreed. 4. The following have the right to discuss my case and may wish to see me together if this is felt appropriate: …………………………………………………………………… 5. If I am intoxicated, my pharmacist has the right to refuse to dispense my medication. 6. I will not be a nuisance, abusive, violent, aggressive or rude to the prescriber, key worker, pharmacist, pharmacy staff or customers. 7. I will provide a urine sample for analysis when requested. 8. I am responsible for any medication which I am prescribed and if I should lose them or take them other than as directed, they will not be replaced. 9. I understand that I can only obtain prescriptions from my named prescriber unless alternative arrangements are made. 10. I understand that I have chosen the pharmacy named in this contract from which to collect my prescriptions. This means that I cannot have my prescription dispensed by any other pharmacy without renegotiating my contract with the prescriber and another pharmacy. 11. I understand that I must collect my prescription on the specified day. If I fail to collect a dose on the specified day, I will not be able to collect that dose on a later day. 12. I understand that if I fail to collect my dose for three days or more, my treatment will be reassessed. TERMINATION OF CONTRACT The prescriber has the discretion whether or not to continue to prescribe to a patient and any abuses or non-compliance with this contract will result in a review of the situation. The pharmacist has the discretion to review whether or not to continue to dispense and supervise consumption if any abuse of the contract, staff or premises occurs. Patients have the right to terminate the contract if they feel the other parties have failed to fulfil the term of the contract. Name Prescriber Team (tick) □ Access □ GP DOB Signature Contact No. Date Copy Type □ Windmill □ Acorn □ Respond □ Other specialist DA service (please specify) Pharmacist Yellow Patient Pink Full Pharmacy Address The prescriber and patient will sign the contract; the top copy (white) should be kept in the patient’s medical records. The other three copies will be delivered to the pharmacist who will sign the contract, retain the yellow copy, return the pink copy to the patient and send the green copy to the Supervised Consumption Scheme Manager: Surrey Harm Reduction Outreach Team Parkview Centre for the Community, Blackmore Crescent, Sheerwater, Woking, Surrey, GU21 5NZ (Please ensure all details have transferred to the green copy) 11 SUPERVISED CONSUMPTION PROCEDURE Prescriber Role Choosing a Pharmacy: The prescriber will discuss with the patient, the most suitable/convenient pharmacy, where the pharmacist will supervise consumption. The prescriber must also explain to the patient that the pharmacist will be required to inform partners as to the progress of treatment and will include for instance, frequency of consumption and in general how stable the patient becomes on their medication. As part of the prescriber/key worker contract, informed written consent to such discussions taking place should be obtained. This is the nature of the ‘shared care’ contract. Contacting the Pharmacy: The prescriber/key worker should contact the chosen pharmacy in advance in order to seek permission by the pharmacist to accept a patient of supervised consumption. This can be done over the phone. Dispensing Arrangements: The pharmacist needs to be informed of the dispensing arrangements prior to the patient attending the pharmacy. This makes the process less distressing for the patient who otherwise might be viewed with suspicion. The prescriber/key worker should verbally inform the pharmacist of the dispensing arrangements with special conditions specified (e.g. confirm the medication is in stock as sugar-free methadone may take longer to order). It is good practice to send the pharmacist an introductory letter stating the name and address of the patient, the dispensing dose, start and expiry date of the prescription, and the names and contact details of ‘shared care’ partners. To save time, this letter can be faxed to the pharmacy. It should be made clear to the patient starting a new prescription that it is best to attend the pharmacy during clinic hours in order that any queries with the prescription can be addressed. Prescription Details: Only prescriptions, which are legally written, can be legally dispensed and care should be taken over getting them right. Prescribers must issue instalment dispensing on blue FP10 (MDA) forms. FP10 (MDA) forms must only be used for Schedule 2 drugs, buprenorphine and buprenorphine/naloxone. Any changes to the prescription requirements will be highlighted to all partners by the pharmaceutical advisor. Writing the Prescription: State the pharmacy name in the top left hand corner, which ensures only the nominated pharmacy, can legally dispense. Supervised consumption takes place every day the pharmacy is open with take-home doses for Sundays and back holidays if the pharmacy is closed on those days. Instructions can include: ‘All doses to be consumed on the premises whenever possible and washed down with a glass of water’, which clarifies the situation for the patient. Strike through any unused part of the prescription. Hand writing exemptions can be issued by the Home Office if more than 10 controlled drugs prescriptions a week are written, but still, they must be signed and dated by the prescriber. The prescription should state the total quantity being prescribed, the amount of each instalment and the intervals between dispensing. See example overleaf: 12 Example of Instalment Dispensing 13 SUPERVISED CONSUMPTION PROCEDURE Pharmacist’s Role Communication: Pharmacists and prescriber/key worker agree which information is to be communicated Pharmacists to agree on a suitable time to discuss any issues that arise from treating patients on the scheme Introductions: Prior to arrival of the patient, the pharmacist should check the details of the contract. Supervision Area: Clarify for the patient where the supervision will take place. Ideally, supervision should never take place in the dispensary. Where possible, a designated area offering suitable privacy should be selected in each pharmacy and used for this purpose as well as discussing other sensitive issues with customers. No other person in the pharmacy should be aware of what the patient is doing. Care is needed in making the patient comfortable and not stigmatised. If the patient is not satisfied that it is suitably private or discreet, they can elect to attend an alternative pharmacy. Patient Contract: Assuming the patient accepts the area of supervision as suitable; the pharmacist should then verbally go through the contract with the patient and complete the pharmacy leaflet. When agreed, the pharmacist will sign and return the patient copy to the patient. The main issues to be covered are: What to do when the pharmacy is closed, e.g. Sundays and/or bank holidays Missed doses cannot be dispensed at a later date The pharmacist will be feeding back to the prescriber/key worker, the observed effect of treatment on the patient That said, the patient’s right to confidentiality remains and information given to the prescriber is strictly on a ‘need to know’ basis The patient can discuss with the pharmacist any issues arising on a daily basis without fear of the prescriber being informed. There are exceptions to this such as child welfare and serious health issues Requests for injecting equipment are not reason enough to inform the prescriber/key worker (Ref: Pg 6) The prescriber/key worker will be contacted and methadone, buprenorphine or buprenorphine/naloxone may not be dispensed if the patient has missed up to three consecutive days’ doses Methadone, buprenorphine or buprenorphine.naloxone might not be dispensed if the pharmacist suspects there is evidence of drug and/or alcohol intoxication due to the risk of overdose and the prescriber/key worker may be contacted as a result. 14 Staff If appropriate, the pharmacist should introduce the patient to key members of staff. The Prescription: When a prescription is presented, it should be checked to see if it is legal and if the quantities and patient details are correct. If the pharmacy has been indicated in the top left hand corner, then check it is correct. The prescription should stipulate ‘supervised consumption’. Preparation of methadone: Doses of methadone should be made up in advance each day (assuming the pharmacist is in the possession of a current prescription). Methadone should be dispensed into an appropriate child restraint container labelled in accordance with the requirements of the Medicines Act. The correct date of dispensing e.g. the date of supply to the patient should be shown on the label. Storage: The methadone, buprenorphine or buprenorphine/naloxone should be stored in the controlled drugs (CD) cupboard until the patient attends. Patients should not witness the removal or replacement of the container in the cupboard. Dispensing: When the patient arrives, the pharmacist must ensure that the patient is correctly identified and receives his/her dose of medication. Supervised patients are highly sensitive to their situation and care should be taken not to disclose to other customers their medication details. Wherever possible, supervision should be conducted out of the public view, in a place that is commonly used for private consultations generally. The methadone should be consumed directly from the bottle or may be poured into a cup provided by the pharmacist. The use of straws should be recommended as a means to promote hygiene. Consumption: The pharmacist must observe the consumption of the medicine by the patient. To ensure the product is consumed, the pharmacist should provide some water for the patient to drink. It is not suitable for the patient to drink something they have brought into the pharmacy. Alternatively, engaging in conversation with the patient also proves the methadone has been swallowed or the buprenorphine, buprenorphine/naloxone has been sublingually dissolved and allows for enhanced pharmaceutical care to take place. Ask if the patient is well or if they are experiencing any problems etc. When all the medication has been consumed, the patient should return the bottle to the pharmacist. For specific guidance on buprenorphine, buprenorphine/naloxone dispensing, please refer to Ref: Pg 16. Documentation: After each dispensing/supervision, the pharmacist should then make the appropriate entries in the CD Register, on the prescription and the record form. Processing for Payment of Prescription: The prescription should not be processed for payment until after the last valid dispensing date/or once expiry date has been passed. Missed Doses: If a patient fails to collect three consecutive doses, no further methadone, buprenorphine or buprenorphine/naloxone should be dispensed without the agreement of the prescriber/key 15 worker. This is due to the risk of overdose once a patient’s tolerance to methadone has been reduced. If three consecutive doses have been missed, the pharmacist should try to contact the prescriber/key worker prior to the patient next attending the pharmacy. This means that when the patient does attend, they can be advised immediately about their prescription and will not have to wait around the pharmacy unnecessarily (regardless of the decision to continue dispensing or not). Individual missed doses (one or two days) should be documented on the record form. It is not necessary to alert the prescriber on that very day. Use professional judgement and if you are concerned about the patient, the prescriber will be pleased to hear from you. However, it may upset the patient’s overall progress on the programme if they think you have been ‘telling tales’ behind their back. Additional Guidance for Dispensing BUPRENORPHINE (Subutex) and BUPRENORPHINE / NALOXONE (Suboxone) Unit dose packaging allows safer and more convenient handling, but risks confusion of strengths and difficulties in popping the tablet out of the blister if individual doses are ‘snipped’ dispensed and labelled. For this reason, some pharmacist’s currently dispensing buprenorphine (Subutex) or buprenorphine/naloxone (Suboxone) have been dispensing the total amount on the prescription all at once. Daily dosed for supervision are taken from these packs without individual patient medication records (PMR) being made on the computerised records. However, the RPSGB legal department have stated that pharmacists must fully dispense and label individual instalments-ensuring daily recording on the PMR. Buprenorphine (Subutex) and buprenorphine/naloxone (Suboxone) are Schedule 3 controlled drug and does not require entry into the CD Register. They are subject to prescription writing and safe custody requirements for controlled drugs. Buprenorphine (Subutex) and buprenorphine/naloxone (Suboxone) should be prescribed in daily instalments (occasionally thrice weekly) for supervised consumption on the correct form The prescription should be marked with “Supervised Consumption” The daily dose should be dispensed and labelled appropriately before the patient arrives (when a prescription is current). Sometimes this may involve a mixture of strengths, which must be separately labelled in accordance with standard ‘best practice’ procedures The original prescription should not be processed for payment until it expires/is completed The patient must have a drink of water before consumption to moisten the mouth. Provision must be made for safe disposal of drinking cups to ensure cross infection does not occur The pharmacist should pop the tablet out of the blister pack, either into the patient’s hand or into a small disposable pot The tablet needs to be taken as a single dose (where possible) 16 The tablet(s) should be placed under the tongue and left to dissolve. The active ingredient passes through the buccal mucosa and produces its effect The tablet should not be swallowed, as it is ineffective if taken in this way The summary of product characteristics states that the buprenorphine (Subutex) tablet will dissolve in five to ten minutes. The buprenorphine/naloxone (Suboxone) tablet will dissolve in two to ten minutes The patient should not leave until the staff are sure that the tablet is dissolved. Once dissolved, what remains is a chalky residue that can be swallowed It is not necessary for the pharmacist to watch the patient continuously – the pharmacist is only responsible for ensuring the tablet goes into the mouth, under the tongue and then confirming with the patient that the dose has been absorbed The pharmacist must be satisfied (either by conversing with the patient, water being swallowed or other means) that the medication has not been concealed in the mouth. Specific guidance for the use of buprenorphine for the treatment of opioid dependency in Primary Care, produced by the Royal College of General Practitioners, will be provided by the PCT. 17 MONITORING, EVALUATION AND AUDIT As part of the RPSGB Standard 14 of Good professional Practice, it states that documentation must be maintained to enable the regular monitoring of the service. One of the roles of the co-ordinator will be to ensure the scheme is successful in achieving the anticipated benefits. In January 2009 the Scheme, including the operational policy, will be evaluated. Pharmacists are asked, therefore, to keep ongoing records of ideas, problems, incidents with individual patients/the prescriber/key worker/co-ordinator, etc. (Ref: Record Form). The views of the patient will also be formally gathered to ensure the service meets the needs of all partners. Further reference, please see Appendix 6 OTHER PHARMACEUTICAL ISSUES The treatment of the majority of minor ailments is no different for patients receiving methadone, buprenorphine or buprenorphine/naloxone than it is for any other patient in the pharmacy. However, there are certain requests which may be common in supervised consumption patients and there are certain OTC drugs, which may cause problems. SEE INFORMATION section Health Promotion Pharmacists should ensure patients have received a copy of the Methadone Handbook 2002 and the patient leaflet. When appropriate, the pharmacist should refer to the various aspects covered by the handbook/leaflet Security of Staff, Premises and Stock Consideration must be given to provide adequate insurance (e.g. check with the NPA). The procedure of supervised consumption should not put staff or patients at risk of suspicion. Avoid allowing patients access to dispensary stock Balance the need of privacy against risk of becoming isolated with a patient Ensure compliance with all legal and professional requirements; in particular with regard to storage of controlled drugs Local Pharmacists A pharmacist must be able to reserve the right not to participate in supervised consumption schemes. It is therefore important to ensure locum pharmacists are told before they agree to work that they will be expected to supervise the consumption of methadone, buprenorphine or buprenorphine/naloxone. The contractor should ensure sufficient staff training to support a locum pharmacist in this. Locum pharmacists should also be aware of what to do if contacted by the prescriber or key worker about new or current patients and have access to, and be familiar with this operational policy (Please see Appendix 7 advice for Locum Pharmacists). 18 Dealing with Problems There are many problems and situations, which the pharmacist is able to deal with efficiently and professionally. It should not be necessary for the pharmacist to continually contact the prescriber about the patient’s behaviour or appearance. By developing links with the prescriber, it is hoped that pharmacists will come to understand what is appropriate for each individual patient. This area will be covered fully in the training workshops for the Scheme. Pharmacists will be expected to use their professional judgement and experience as well as knowledge of the patient to decide what would be an appropriate reason for contact. The operational policy makes some suggestions. As there may be occasions, which would not warrant a specific call, pharmacists should keep an ongoing record (in this manual), which will assist, at the patient’s regular reviews and for audit of the service. Confidentiality Patient confidentiality must be maintained and it is vital that the pharmacist does not inadvertently discuss the patient with an unauthorised person. This Scheme helps pharmacists with this as patients have given their consent for pharmacists to discuss their treatment with their key worker/prescriber. Discussions with the prescriber and the key worker must be directly relevant to prescribed medication. Pharmacists are referred to the obligations of part 2 of the Code of Ethics. Pharmacy staff must also be made aware that they are also bound by the principle and the additional guidance of the code. Request for injecting equipment and needle exchange Patients participating in substitute prescribing programmes may also request injecting equipment. In such cases, where the pharmacist participates in the local needle exchange scheme, the required needle exchange packs should be supplied in the usual way. Even in the most effective methadone programmes about 25% of patients will continue to inject; many more may inject as a “treat” from time to time. Preventing access to sterile equipment will not stop them injecting but may well force them to share equipment, which is a serious public health risk. The key worker/prescriber will carry out regular urine testing and any additional drug use by the patient will soon become apparent. Pharmacists may take the opportunity to talk about the risk of overdose; patients who feel confident in the pharmacist’s discretion and confidentiality may be more willing to discuss this and other aspects of their treatment. Patients must not be made to feel judged by any member of staff as this could impede the effectiveness of the substitute-prescribing programme and may also lead to risky injecting behaviour. A list of pharmacists who participate in the local needle exchange scheme is contained in the leaflet available with this operational policy. This is a free and confidential service where patients can obtain sterile needles and syringes and return used injecting equipment for safe disposal. 19 Training Pharmacists who take part in this Scheme must be committed to continuing professional development. The following must be completed: Induction (workshop or one-to-one) Attendance at the annual PCT harm reduction workshop CPPE Distance Learning Course: Substance Use and Misuse (Ideally, to be completed within six months of the commencement pf provision of the service) Material, which may be of use: “The Methadone Briefing” by Andrew Preston, 2002 available from Drugscope. “Drugs of Abuse” by Simon Wills, published by the Pharmaceutical Press, 1997 Drug Misuse and Community Pharmacy: Jane Sheridan and John Strang, 2003 20 HEALTH AND SAFETY Helpline for pharmacists under Threat As with all public situations, there may be times when you feel threatened. If appropriate, the pharmacist must contact the police. The co-ordinator and the Pharmaceutical Advisers are also available to offer help and advice. There have been instances where a pharmacist has felt unable to contact anyone about a particular problem, in particular related to drug mis-users. In the event of such a situation, the RPSGB Benevolent Fund “Listening Friends” Scheme can be contacted for free, confidential support. The Listening Friends Scheme: Telephone: 020 75 72 24 42 Needle Stick Injury Any accident with needles or syringes must be reported to the pharmacists. In the event of a needle stick injury: Encourage wound to bleed freely and wash thoroughly with soap and cold water, splashes of blood in the eye or mouth should be irrigated copiously with water Affected person should report immediately to their nearest Accident and Emergency Department for post exposure prophylaxis – preferably within 60 minutes. (DoH circular PL/CO (97)1) Keep the sharp responsible (in a safe place) and make an entry in the accident book. Hepatitis B Immunisation Following guidance, all health care workers should be vaccinated against Hepatitis B REF: UK Health Departments Guidance for Clinical Health Care Workers: Protection against infection with blood born viruses. DoH J15/002 12784 HP 75K 1P Mar98 BEL Care should be taken to avoid exposure to blood or other body fluids No vaccination is available against HIV or Hepatitis C. 21 TERMINATION OF SHARED CARE CONTRACT The pharmacist and Doctor have the right to expect the patient to conform with the behaviour requirements of the contract. Failure by the patient to adhere to the contract may result in the review of the situation. The prescriber may choose to refuse to continue to prescribe and the pharmacist may review the continuation of supervision supply. Cancellation of the contract should be the last choice and it would be expected that all other avenues have been explored first. Before any action or decision is taken, please discuss with the PATIENT and at least one of the following: Prescriber (Does not apply if the prescriber is reviewing) Pharmacist (Does not apply if the pharmacist is reviewing) Key worker Scheme Co-ordinator Community Pharmacy Facilitator Outreach Team. If all attempts to sort out the problem fail, the contract may be terminated (as a last resort) by the following means: Inform patient Inform prescriber Inform Scheme Co-ordinator Inform Pharmacist Inform Key Worker. The patient has the right to terminate the contract if they feel that the other parties have not fulfilled the terms of the contract. The patient should be encouraged to contact the aforementioned people to discuss their problems before terminating the contract. 22 Appendix 1 REMUNERATION FOR PHARMACISTS The last government initiated a number of extensions in the provision of treatment for serious drug misusers. The present government has continued this policy. Amongst other things, PCT’s have been asked to: Facilitate greater involvement of primary care professionals, such as general practitioners and community pharmacists, in the care of more stable drug mis-users Support well-managed methadone administration and associated counselling and care programmes for opiate mis-users, aimed at immediate harm minimisation, with the ultimate goal of abstinence wherever possible. Treatment with methadone or similar drugs is believed to be more effective when it is administered through a formalised ‘partnership’ arrangement. This Scheme aims to bring together the patient, community pharmacist and the drug misuse service. Participation in this Scheme will be limited to opiate mi-users who wish to make a commitment to reducing or eliminating their dependency. Each contract will require regular attendance by the patient at the pharmacy and the drug misuse service, as well as regular communication between the three parties, for a period of up to thirteen weeks, for supervised self-administration of Methadone, buprenorphine or buprenorphine/naloxone under the observation of a pharmacist on pharmacy premises. Non-compliance may cause termination of the contract. The PCT invites contractors to participate in a 12-month contract with the PCT. Attendance at an annual workshop and completion of the CPPE training package will be required, upon receipt of the CPPE certificate; an annual retainer fee will be paid. In recognition of the pharmacist’s contribution, the PCT will pay a flat rate fee of £1.93 per supervised dispensing. Payments will only be authorised by the Scheme Co-ordinator on receipt of a copy of the contract and copies of patient record forms. Local set up and induction training costs will be met by the scheme. Participating pharmacists must have facilities and staffing levels appropriate for observed consumption in their premises. This Scheme has a limited number of supervised dispensing available, in the event of an over subscription of pharmacy applications, first consideration will go to pharmacies who are deemed suitable in order to ensure the needs of the service in our area are met. For these patients who require more than thirteen weeks supervised consumption, the PCT will arrange further payments for dispensing as required. 23 Appendix 2 Community Pharmacy Supervised Consumption of Drugs Annual contract with the PCT Pharmacy Address Name of Pharmacy Contractor: ………………………………………………………. Name of Pharmacist: ……………………………………………………….. Contract to run from: ………………………………… To: 31st March 20 …………. I agree to provide supervised consumption of: a) Methadone b) Subutex c) Suboxone as part of the Surrey Scheme I understand that in return this service and complying with the following criteria, the pharmacy contractor will be paid a retainer fee and supervision fees as agreed with the LPC and specified in the policy. I agree to undertake the required training as specified by the PCT I have read and fully understand the operational policy I agree to send a copy of my CPPE certificate, the standard operating procedure specific to my pharmacy and proof of attendance at the workshops/induction I agree to provide sufficient information and staff training to enable any managers/locum pharmacists to provide the service in my absence I am aware that supervision payments will only be made when the Scheme Manager at the Outreach Team receives a signed copy of the shared care contract and the appropriate record forms I agree to provide the service for the term of the contract as stated above. Signed: ………………………………… (Pharmacist) Date: …………………. Signed: ………………………………… (Contractor) Date: …………………. Signed: …………………………………. (PCT) Date: …………………. Surrey PCT Pharmacists may at any time give notice in writing that they are terminating the annual contract between the PCT and pharmacy 24 Appendix 3 Supervised Consumption Record Form For office use only: Patient Ref: For office use only: Payment Ref: Number of Dispensings: Patient Initials: Pharmacy Stamp: Date of Prescription: Gender: Methadone dose: Date of Birth: Subutex dose: Suboxone dose: Date Special Instructions e.g. supervised, daily pick-up, twice weekly pick-up Supervised / Collected Please circle Comments e.g. Sunday dose taken, changes to original script Y or N Y or N Y or N Y or N Y or N Y or N Y or N Y or N Y or N Y or N Y or N Y or N Y or N Please make a note below of any INTERVENTIONS, PROBLEMS OR SITUATIONS that you have come across. This information will be useful when the patient is reviewed and it will help us when we audit the project. Please include any correspondence with prescriber/key worker, Scheme Manager and any adverse events Date Interventions, Problems or Situations Prescriber/Windmill/ acorn/Respond Team Contacted Yes or No Date patient stopped supervision: ……………………………… Reason (e.g. went into daily pick-up): ………………………………………………………………………. Pharmacist Name: ……………………………. Signature: ………………….. Date: ……………. On completion, please post this form IMMEDIATELY to: Community Pharmacy Drug Misuse Manager, Surrey Harm Reduction Outreach Team, Parkview Centre for the Community, Blackmore Crescent, Sheerwater, Woking, Surrey, GU21 5NZ Tel: 01932 355533 Fax: 01932 350963 25 Appendix 4 List of medication for supervised consumption (September 2007) Methadone Mixture 1mg/ml (Sugar free) Methadone Mixture 1mg/ml Methadone Mixture Concentrate 10mg/ml* Buprenorphine (Subutex) 400mcg Tabs Buprenorphine (Subutex) Tabs 2mg Buprenorphine (Subutex) Tabs 8mg Buprenorphine 2mg/naloxone 0.5mg Tabs (Suboxone) Buprenorphine 8mg/naloxone 2mg Tabs (Suboxone) *CARE. This will only be prescribed on relatively rare occasions and the SOP must have safety mechanisms to ensure that this is not dispensed unless specifically asked for. 26 Appendix 5 HARM REDUCTION and DRUG TREATMENT Harm reduction aims to reduce or limit the harm to communities and individuals caused by drug and alcohol use. Key roles for the pharmacist: Dispensing services – including daily/supervised/instalment dispensing of: - Methadone - Buprenorphine – Buprenorphine/naloxone - Diazepam (when appropriate) or other medication as agreed with the PCT, LPC and the prescriber Supply of clean injecting equipment via needle exchange schemes Monitoring of general health Harm minimisation advice - To stop injecting - To stop sharing injecting equipment - Safer injecting practices - Disposal of used paraphernalia - Advice on safe sexual practices and sexual health - Supply f condoms Information re. GP, drug services, needle exchange schemes Health promotion literature Monitoring of prescriptions for potential overuse of medicines or for interactions with non-prescribed drugs or other prescribed drugs (using patient medication records) Evaluation of legal validity of prescriptions and screening for errors Identification of inappropriate prescribing Monitoring the misuse potential of ‘over-the counter’ medicines (OTC) Advice on smoking cessation. A flexible approach is essential when working with drug users. It can take time to adjust to a methadone, buprenorphine or buprenorphine/naloxone prescription, whilst the patient becomes stable on an appropriate dose and distances him or herself from a range of cognitive, emotional and behavioural patterns associated with problematic drug use. With support, supervised consumption can significantly reduce the harm of illicit heroin use, such as the risk of: HIV and hepatitis infection Overdose Chaotic drug use Criminal behaviour. Methadone, buprenorphine and buprenorphine/naloxone prescribing has also been shown to improve: Contact with primary health care services Social stability Diet and general health. 27 In this sense, prescribing methadone, buprenorphine or buprenorphine/naloxone as a substitute opiate can clearly be seen as a harm reduction measure. It will minimise the risks associated with illicit heroin use, namely, health issues, financial concerns, criminal activity, relationship difficulties, housing problems etc. It is not ‘treatment’ in the traditional sense where the aim is to ‘cure’ an affliction. Receiving a regular measured dose of methadone can sometimes be the first step in enabling the opiate-dependent person to gain stability in their lives. Nevertheless, this process can take a number of attempts and patients should not be made to feel they have ever failed a programme as it is always possible to learn from each attempt (fig 1). Figure 1: ‘Cycle of Change’, taken from Prochaska & DiClemente (1992) DETERMINDATION ACTION START: PRECONTEMPLATION CONTEMPLATION MAINTENANCE PERMANENT EXIT RELAPSE When patients start a methadone programme, it is desirable to commence them, whenever possible, on a supervised regimen (bearing in mind working/child care arrangements etc). However, once the patient is stabilised, they can accept more responsibility through the introduction of ‘take home’ doses, for example from daily to six times weekly, to two or three times weekly, to weekly. The pharmacist should recognise the benefit or reimposing supervision in times of crisis or relapse and discuss this with the prescriber/key worker. 28 Appendix 6 Monitoring, Evaluation and Audit Questionnaire to Pharmacist, Prescriber and Key Worker Improvement in Communication Has this occurred? Has it worked? Who has communicated? What has been communicated? Has it been relevant? Financial and Activity Projections Has payment arrived on time? Any problems with payment? Is remuneration appropriate? Has the project been successful? It is vital to the success of the scheme that pharmacists are able to demonstrate their contribution to the ‘shared care’ of the patient. The only way this will be possible is by ensuring the pharmacist documents any intervention fully, either with prescriber/key worker or patient. The co-ordinator will help with this process as much as possible. The pharmacist will be asked to complete a questionnaire asking: What they thought of the scheme What they thought about the guidelines and information provided What they thought about the co-ordinator’s input Was anything missed out? Is there anything useful to be learned? Did the scheme achieve what was expected/hoped for? 29 Appendix 7 ADVICE FOR LOCUM PHARMACISTS The Pharmacy has a contract with the PCT to provide supervised consumption of Methadone / Subutex / Suboxone and / or instalment dispensing of benzodiazepines SUPERVISED CONSUMPTION OF METHADONE / SUBUTEX / SUBOXONE The full Policy explaining this scheme can be found in the: ………………… Surrey Supervised Consumption Scheme Resource File – Section 1 ……. The Paperwork you will need to complete can be found: ……………….. Surrey Supervised Consumption Scheme Resource File – Section 4 ……... The following Information may be found: Prescriptions for this project will be from: - The Windmill Drug & Alcohol Team (Abraham Cowley Unit) - Acorn Drug & Alcohol Team - Respond - The Access Team - Specialist Centre’s & Primary Care GP’s Instalment prescriptions will be written on FP10(HP)(Blue) Instalment prescription from Sunday and Bank Holiday doses should be supplied a day in advance if this is the usual procedure Each patient will have a contract which will be kept in the policy folder. Take a few moments to identify how many patients you can expect Each patient will have a record form located (please complete details): ……………………………………………………………………………………………….. If a patient misses three doses, you must inform the prescriber. However, if this happens at a weekend, please use your professional judgement and contact the prescriber on Monday. INSTALMENT DISPENSING OF BENZODIAZEPINES Policy and paperwork can be found: ………………………………………………………… USEFUL NUMBERS The Windmill Team Acorn Team Respond Access Team Supervised Consumption Manager 01932 872010 01483 450256 01372 379739 01932 875213 01932 355533 30