* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download dr.mohamed farouk Cervical cancer
Survey
Document related concepts
Transcript
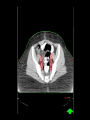
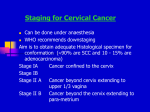
CERVICAL CANCER: RADIATION ONCOLOGIST PERESPECTIVE Mohamed farouk akl PhD clinical oncology Anatomical considerations: The cervix is conical in shape and typically measures 3 × 3 cm portion of the cervix that protrudes into the upper vagina is referred to as the ectocervix The ectocervix has a central opening referred to as the external cervical os that extends superiorly to become the endocervical canal and terminate at the internal cervical os to become the endometrial canal The endocervix is lined by columnar epithelium, while the ectocervix is covered by squamous epithelium The region where these two epithelial layers meet is referred to as the squamocolumnar junction Anatomical considerations (cont'd) : The cervix is attached to the lateral pelvic wall by a pair of ligaments at the base of the broad ligament referred to as the cardinal ligaments This ligament contains the uterine arteries and veins. The uterine arteries pass over the ureters on each side in close proximity to the cervix Most cervical malignancies arise in the mucosa of the SCJ and invade into the underlying cervical stroma Lesions can be exophytic or endophytic and spread by direct extension to the uterine fundus, surrounding vaginal fornices,parametrial tissues, pelvic sidewalls, rectum and vagina illustration of the anatomical components around the cervix with reference to the parametrium. LYMPHATIC DRAINAGE: The cervix drains into the paracervical lymph nodes which then drain into the obturator, internal iliac, and external iliac lymph nodes followed by the common iliac and para-aortic lymph node follows a stepwise pattern by spreading to the pelvic lymph nodes before the para-aortic lymph nodes. CT SCAN FINDINGS IN CA CERVIX: The normal cervix has a variable enhancement pattern The primary tumor is heterogeneous or hypodense relative to normal stroma on contrast enhanced scans Obliteration of the periureteral fat plane and a soft-tissue mass are the most reliable signs of parametrial extension Less than 3 mm separation of the tumor from the pelvic muscles and vascular encasement are signs of pelvic side wall invasion Obstruction of the endocervical canal leads to distention of the endometrial cavity with blood, serous fluid, or pus The limitations of CT have been lack of consistent visualization of the primary tumor and inaccurate detection of parametrial invasion cervical cancer as a hypoattenuating mass (solid arrow) with diminished enhancement when compared with the normal stroma (open arrow) of the cervix A low-attenuation mass (arrow) is present in the cervix, and the attenuation of the parametrium is increased bilaterally The fat plane around both ureters has been obliterated (arrows) A low-attenuation cervical mass is present with irregular margins and thick parametrial soft tissue Strands. The vagina (open arrow) is expanded by the tumor growing into it from the cervix. The tumor involves the lower one-third of the vagina, a finding consistent with stage III disease The mass extends to the rectum (open arrow) and also involves the bladder at the right ureterovesical junction enlarged node in the lateral external iliac chain (solid arrow) as well as the enlarged node in the medial chain (open arrow). MRI findings in normal cervix: MRI anatomy of the cervix is best delineated on T2W image as four major zones of cervix From center to periphery, these are high signal intensity endocervical canal, intermediate signal intensity plicae palmatae, low signal intensity fibrous stroma, and intermediate signal intensity outer smooth muscle MRI findings in normal cervix (cont'd) : MRI findings in ca cervix: The basis of the radiologic evaluation of cervical cancer is T2-weighted MRI sequence Cervical ca is characterized by high signal intensity against low signal of cervical stroma Sagittal and transverse T2-weighted sequences serve to determine the localization and size of the tumor as well as the depth of cervical stromal invasion These sequences are also crucial for excluding extracervical extension and infiltration of the parametria, vagina, bladder, and rectum The two critical issues – depth of infiltration and parametrial involvement can be assessed most reliably on axial images MRI findings in ca cervix (cont'd) : On T1-weighted MR images, cervical cancer is similar in SI to cervical stroma. Demarcation from the corpus uteri, vagina, and parametria is difficult In the routine clinical setting, T1-weighted sequences are primarily used for lymph node staging T2WI :The cervical cancer is seen as a hyperintense mass in the surrounding lowsignal-intensity cervical stroma The cervical cancer (asterisk) is seen as a large mass of intermediate to high signal intensity that is delineated against a very thin margin of lowsignal-intensity cervical stroma and against the more hypointense myometrium of the uterine corpus Stage IB cervical cancer The tumor is surrounded by low-signalintensity cervical stroma stage IIB cancer of the posterior cervix with disruption of cervical stroma Stage IIA disease: High signalintensity cervical cancer with infiltration of the posterior vaginal fornix Stage IIB disease: Posterior disruption of the cervical stroma and a solid tumor extending in a posterior direction are signs of parametrium infiltration Stage IIB disease: Large solid tumor extends into the parametria posteriorly but do not infiltrate the rectum. Also see the nodal metastases of the internal obturator group, along the internal iliac artery, and of pararectal nodes on the left Stage IIIB disease: T2w image Cervical cancer with right lateral parametrial infiltration and infiltration of the right pelvic wall Stage IIIB disease: Cervical cancer with right lateral parametrial infiltration and infiltration of the right ureter, which is distended as a consequence Stage IVA disease: Cervical cancer with infiltration of the posterior parametria and invading the rectum enlarged lymph nodes of the common iliac artery group on both sides SIMULATION AND DAILY LOCALIZATION: Patients may be set up in either a supine position or prone position use of a belly board to allow setup reproducibility in prone CT simulation should be done with ≤3 mm slice thickness -/+ Intravenous contrast In cases of vaginal involvement, a radiopaque marker should be placed at the caudal extent of the tumor bladder and rectal fullness should be maintained Nodal CTV components: nodal CTV was subdivided into five regions, i.e. common iliac, external iliac, internal iliac, obturator and presacral. CTV components: CTV components: CTV components: The CTV should be divided into three subregions: CTV1 should include the gross tumor volume (GTV), cervix, and entire uterus for intact patients or 3-4 cm of the proximal vaginal cuff for postoperative patients. CTV2 should extend 2 cm below the most inferior extent of vaginal disease and parametrium. CTV3 will include lymph nodes. CTV components: GTV (red), cervix (pink), uterus (blue), vagina (yellow), parametrium (green), bladder (purple), rectum (light blue), and sigmoid (orange). Arrow heads refer to uterosacral ligaments and mesorectal fascia. Arrows refer to the broad ligament and top of the fallopian tube Parametrium borders: Parametrium borders: Parametrium borders: Parametrium borders: Stage-specific delineation schemes for the posterior border of the parametrium (solid red line): (a) Non-bulky early-stage (IB1 or IIA) disease. (b) Bulky early-stage (IB2 or IIA) (c) Stage IIB (slight parametrial involvement). (d) Stage IIIB disease (massive parametrial involvement). Japanese clinical oncology group guidlines Suggested CTV-PTV margin: Postoperative ca cx: marked difference between uterus and cervix positions, with altered bladder filling