* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download -click here to download - Full Page
Survey
Document related concepts
Transcript
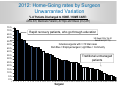
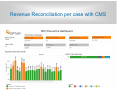
Physicians and Hospitals Odd couple or match made in heaven Mark I Froimson, MD, MBA Former, President, Euclid Hospital Cleveland Clinic Now, Executive Vice President, Chief Clinical Officer Trinity Health Medical Updates March 9, 2015 1 1 COI Disclosure (in last 5 years) Consultant MCS DePuy Synthes CITI Speaker Care Fusion Research Support Stryker Leadership/Board Positions MAOA Board member, AAHKS 3rd VP, AAOS, AF Editorial Boards/Reviewer JOA, AJO, JBJS 2 Cleveland Clinic: A Physician Group Practice Led Academic Medical Center/Health System Largely Integrated Model of Care • 44,000 employee caregivers • 5.1 million total visits • 50 states and 132 countries patient coverage • 160,600 hospital admissions • 3,000+ employed physicians and scientists, plus private practice • 8 community hospitals, 16 family health centers • Florida, Nevada, Toronto, Abu Dhabi 3 3 Trinity Health: A National, Multihospital Catholic Health System with mixed Medical Staffing Model • 89,000 employee colleagues • 86 Hospitals, >100 continuing care orgs • 27 Regional Health Systems • 21 states, • 3,500+ employed physicians • 25,000 affiliated physicians • 30M patients in service areas • 500,00 hospital admissions per year 4 4 Philosophy of accomplishment "It's amazing how much you can accomplish when you don't care who gets the credit.“ Harry S. Truman (leave your ego at the door) Trust Speak the Truth Show Respect Communicate Relentlessly Physician Integration: Engaging Doctors in the Health Care Revolution---HBR Thomas Lee, MD, Toby Cosgrove, MD • Shared Purpose • Restore nobility of the calling • Self Interest • Financial Incentives • Lifestyle • Earning Respect • Reputational significance, competitive streak • Embracing Tradition • Stewardship of profession The Burning Platform? The call to action? Is US healthcare a bad deal? Does this motivate physicians? 8 Is it quality that is lacking in the industry or is it reliability? Gloria’s Email ….is John’s rehab physician. He also needs a medical doctor. Who would you recommend? ….I think it’s time. I need a new knee. Can you do it or who would you recommend? Desired Attributes of Health Care Excellent Safe Expert Reliable Trustworthy Reproducible Predictable Cleveland Clinic Tag Line “Every Life Deserves World Class Care” (Implied standard to aspire to) March 3, 2015 l 11 The Quality/Reliability Problem: Adverse event rate is high compared to other industries The A- surgeon phenomenon Do you ever choose your pilot when you fly? Why not? Is it because you know that they have standardized processes for safety? “Big Med” Atul Gawande Why Can’t Healthcare standardize like the Cheesecake Factory? March 3, 2015 l 14 Are there better comparisons? Mode of Transportation Mode of Transportation Comparatively reliable 98.5% What degree of sameness and reliability do we expect from a new car? Why is this missing in health care? We don’t all want the same car. But when we choose a product we expect to get what was promised Reliability in Industry : How do we move this in healthcare? Selection Training Credentialing Culture System and team based thinking Clarity of offering—standard product Standardization Process---4 E’s Engage Explain why the interventions are important Evaluate Educate Regularly assess for performance measures and unintended consequences Share the evidence supporting the interventions Execute Design an intervention “toolkit” targeted at barriers, standardization, independent checks, reminders, and learning from mistakes Pronovost PJ, et al. BMJ. 2008;337:963-5 . From Autonomy as the defining trait to system based thinking…The Elements of Change • • • • • • Culture is everything, need to get buy in Acceptance of current state and past success Burning Platform—What is the imperative? Shared Vision of Ideal state Direction and Path forward Can we think in new ways about how we deliver care? Why Health Care Is Stuck And How to Fix It Drive Value for Patients by Michael E. Porter and Thomas H. Lee, HBR Bundled Payments We All know what needs to be done: Keys to Driving Value in Health Care Care Coordination Best Practices Care Paths Reducing disutility Improving Quality Streamline Processes Eliminate Waste/Redundancy Shift Care to Lower Intensity Venue Reducing Cost How do we get physicians involved in improving quality and reducing cost? Sebastian Thun, on getting things done: ---Need an extrinsically set goal The big game, big test phenomenon Driverless Car DARPA Google Glass Innovation Challenge What is our external challenge? The Industry is Changing: Navigating the Affordable Care Act l 23 Our Catalyst for Change: 2010 PPACA Perhaps the most important Affordable Care Act mandate: the creation of the Center for Medicare and Medicaid Innovation to explore new payment models for integrating care ACO Model for Primary care Bundled Payments for Care Improvement Episode of Care Model gives physicians a vehicle to restore sense of professionalism • Fulfill a promise to patients—better care • Opportunity for Financial gain and ease of practice • Metrics of success • Competitive performance • Sustainability of the profession Health Care Reform: Approaches to Care Two paradigms in health care reform Medical Home/ACO Health Status 1 Managing baseline health needs (population health): preventive care, chronic care, health maintenance Episode Management/Bundles 2 Managing episodes of care: hospitalizations, surgical interventions (joint replacement) Baseline=40% Episode= 60% Cleveland Clinic Complete Care: Creating Value Through Episode Management Premise: When change in health status demands intervention, managing the entire episode is preferable to fragmented care delivery Tactic: Care redesign focusing on improved care coordination and patient and provider engagement yields better care at lower cost Strategic Imperative: Providers who master this approach will have a competitive advantage in the marketplace Four Models of Bundled Payment offered by CMMI/BPCI 41% 36% Only Complete Episode 16% 7% I II III Model 1 2 and retrospectively Modeladjusts 3 Use current FFS paymentModel system Acute Inpatient And Prof Acute Inpatient Prof, Post-acute Post-Acute only IV Model 4 Payment Prospective Acute Inpatient And Prof. EH one of only 13 to go live “at risk” October 1, 2013 >4000 providers are in the pipeline with proposals Source: Advisory Board Bundled Payment for an Episode: TJR • Composite product, includes all care for the episode • Triggered by a Hospitalization/Surgical event • Coordinated to optimize resource utilization and outcome $$$ one price for episode Care coordinator $ $ Prim Care Ortho O O Jan Feb Mar Courtesy C. Donovan Apr $ PreAdmit May TJR Rehab/ Snf/hc Readmit? O H O Jun Jul Aug 7 days pre Prim Care H Sep O Oct 30-90 days post Nov Dec CMMI/BPCI Basics • A CMS contracting entity (initiator) chooses one or more Episodes from among 48 (covering 172 DRGs) • 10/13 CC/Euclid Hospital---DRG 469/470 Total Joint • CMS provides historic hospital specific MSPB* for the episode which sets the base price • Entity evaluates ability to beat that target price • Entity sets duration for the episode that defines discount • 3% discount for 30 day or 2% for 90 day • Price is locked in for 3 years • Physician billing and revenue cycle does not change under the program; CMS distributes BPCI gains retrospectively each quarter *Medicare Spend per Beneficiary Getting the work done: Define the episode Example of Joint Replacement Engage the team Steps Specifics for TJR 1. Medical Condition: Define the entity to be treated Advanced, symptomatic, recalcitrant arthritis hip/knee DRG 469,470 2. Health Outcomes of interest Pain free, functional joint by the end of the episode— interval outcomes that need to be addressed! 3. Define population: who are we treating? • Patients with the medical condition who are indicated and optimized for this treatment rather than none or alternate • Risk Stratification, Exclusion of certain populations 4. Define intervention Primary TKA, THA 5. Define initiating event and timeline -7,TJR,+30days, 90, 180 6. Define resources needed to produce outcomes: people, places, processes • Includes all professional, lab and technical components • Includes all preop and post op care, inpatient and outpatient care Euclid Hospital Episode BPCI summary Bundle MS DRGs 469 & 470 Primarily Total hip/knee replacements* Episode Duration 7 days prior and 30 days post Episode Initiator Target Price Euclid Hospital (EH) $18,948 (MS-DRG 470) $28,673 (MS-DRG 469) 3% off 2009-2011 EH MSPB for DRG Patient Population Medicare fee-for-service patients Duration of contract 3 years (10/1/13 – 9/30/16) All costs of care above CMS contracted price including readmissions within 30 days Savings beyond 3% cost reduction for episode Risk Reward *These MS-DRGs also include ankle replacements and some hip fractures Key Provisions: Waivers and Gainsharing Waivers • 3-day hospital stay for PAC payment • Home bound status for Home Care • Pre-hospital home safety check Gainsharing • • • • Opportunity to share risk and reward among providers Physicians can receive up to 50% bonus over FFS rates Based on performance measures and rules Within a CIN or other collaborative arrangement The Business Case: Value is Created by Better Episode Management through Care Redesign Traditional fragmented delivery Cost (revenue) Portion of savings to payer Value creation Available margin for provider New Model of Care Time The Patient Perspective: Viewing Care as a Complete Episode is What Patients Want Provider Centered: Bundled Payment Patient Centered: Complete Care 35 Episode-Based Complete Care Philosophy Our Promise to Patients: We will deliver all the care needed to get you through entire episode of care Care Path utilization: Following best practices Care Coordination: Working seamlessly together Connected Care: Providing care in appropriate venue Patient Commitment: You must be engaged in the process, bring resources, get educated and work to modify your risk 36 Care Redesign Opportunities: Complete Care Principles • Patients do not want unneeded interventions • Patients want to go home as soon as it is safe • It is our job to: • Arrange and optimize the entire episode up front • Educate them on the options for care and enable early return to home • Make them feel safe • Eliminate unnecessary interventions Complete Care Principles • Leadership is essential – Physician is the team leader • Builds culture, restores joy and professionalism • But it takes a team approach, must engage team • Eliminate unneeded steps or resources • Patients don’t want unnecessary care • Time in an institution should be minimized • Resist impulse to do something as the default • More is not always better: be thoughtful • Engaged/educated patients are our greatest assets • The care we offer should integrate into their lives What’s old is new again…but with better tools to implement Care Redesign Opportunities Across the Care Continuum The Cleveland Clinic Complete Care Framework Developed by a collaborative team to direct the work (100’s) Patient Presents with Medical Condition Indications for proposed intervention Pre Operative Patient Optimization and Risk Assessment Shared Decision Making Care Path Implementation Decision support Best Practice-EBM Discharge planning: Rapid Recovery protocol Connected Care Team Care Coordination Patient Engagement Family and Community Support and safe home environment Resource optimization Risk and Complete Care Management: Principles agreed to by physician leaders • Modify the risk factors that the patient brings • Factors that impact anesthetic/mortality risk • Factors that impact wound healing • Factors that impact rehabilitation potential • Inform patient about the impact that risk factors confer on outcomes • Engage patient in managing and optimizing medical and social determinants of success Two Separate Processes: Indication vs. Optimization Is this patient indicated for surgery? • • • Sufficient symptoms interfering with ADL, work or recreation, QOL Inability of alternative treatment to resolve symptoms Objective evidence of joint disease amenable to surgical correction Is this patient optimized for surgery? Should it be scheduled or delayed based on: • Psychologically and Medically fit for surgery • Adequate support and home environment TJA Preoperative Planning and Assessment: invest up front in process Change the work flow for surgical scheduling from Indication----Scheduling---Optimization to Indication----Optimization----Scheduling Allows optimal patient, family and system preparation to ensure shared decision making and smooth care through episode Preoperative Checklist: Managing Risk for Readmission and increased LOS after TJR Role of Predictive Analytics 1. Diabetes: Hgb A1c if >7.9 delay and refer 2. Smoker: if YES then refer to smoking cessation 3. BMI: if >40---refer for counseling, metabolic consult 4. Anemia: if Hgb <12 in females and <13 in males, delay and refer for wu or blood management* 5. Staph colonization: if in HC facility or HC worker or hx of MRSA, screen and decolonize 6. Narcotic dependence, manage upfront 7. Anticoagulation history or need perioperatively 8. Lack of supportive home environment Care Path Protocols: Eliminating Unnecessary interventions Physicians must drive standardization No more daily lab draws No X-ray in PACU for knees No IV PCA No Ice Man or CPM No Femoral Block No bipolar sealer No bulky dressing, drains No routine Foley Catheter Use TXA. Local blocks Rapid Recovery Protocol 2012: Home-Going rates by Surgeon Unwarranted Variation % of Patients Discharged to HOME / HOME CARE: DRG 470, Medicare Patients, All Hips and Knees (n=2,281) 75% 70% 65% Rapid recovery patients, who go through education US News Ortho Top 20 benchmark (51.1%) 60% 55% 50% 45% Includes surgeons with >=10 total cases Dark Blue = Employed surgeon; Light Blue = Community 40% 35% Traditional unmanaged patients 30% 25% 20% 15% 10% 5% 0% 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 Surgeon Patient/Family Engagement and Home environment: An underutilized opportunity Standardize the approach across practices •Go into the home pre-op and make modifications •Preoperative education and counseling is key •Rapid Recovery Identify a reliable care giver / support Must agree on a discharge date and venue of post acute care All patients coming from home should plan to go home Decide up front on transportation Identify impediments to home DC Stairs/bedroom/bathroom on same floor Distance from hospital Building Business Intelligence Tools to Clearly Define and Track Performance Clinical Outcomes Patient Safety Process measures Physical therapy day of surgery Decrease in pain medications needed Compliance with Care Path Core measures Patient optimization prior to surgery Outcomes measures PRO, HOOS/KOOS Return to work/sports Range of motion PT test, Pain free Pt safety indicators, SSI, Readmissions, Re-operations, Post operative falls, Post-op nausea/vomiting Transfusion Process measures Outcomes measures Patient Experience Efficiency Patient and family education Engaged and activated patients Family/Support person involvement Quality shared decision making Appt. when wanted Feel prepared for discharge Joint class Resource utilization Cost of care Utilization Review: avoiding unnecessary tests, Reduced LOS, Discharge disposition Rapid Recovery program HCAHPs Return/second surgery Total cost of care Contributions to cost (acute, post acute venue, complications, readmissions) 48 Quality and experience are improved Q1 2013 Q1 2014 SNF 56% 22% DC Home 39% 77% CAUTI rates 5.2% 0 Transfusion rate 15% 2% Infection rate .75% 0.0% Readmission 5% 1.6% IP LOS 3.4 2.8 49 Transparent Sharing of Performance Measures: Cost and Quality Metrics by Physician and versus the target price Revenue Reconciliation per case with CMS 51 Q4 2013, Q1 2014 CMS Revenue Reconciliation DRG 470 469 Benchmark Price $19,319 - Target Price $18,739 - Episode Cases Target Amount Medicare Spend 165 $3,091,935 $2,905,605 0 - Gain Due to Euclid $186,285 - Note: Total Cost per Case = 17,610 Margin = $1129 per Medicare TJR Care Redesign reduced FFS revenue by $281,985 • In FFS model, CMS would have all savings, in BPCI model. CMS gets $95,700 savings • Euclid is receiving a $186,285 gain share BPCI is an excellent model for providers to both deliver value to payers and retain value created Pre BPCI FFS episode payments Cost (revenue) CMS limited to 3% $95,000 Value creation Episode of care payment in BPCI Better Quality/lower cost CCF retains value created $186,000 Available for GainSharing Gain Sharing: Guidelines • Develop Risk Pool • As part of Quality Alliance • Clinically Integrated Network • Process Metrics • Participation in development, reporting • Compliance with Complete Care protocols • explain deviation when appropriate--learning • Outcome of the cohort • specialty specific • entire cohort Offering a New Product to the Market: Benefiting Patients, Engaging Physicians Cleveland Clinic Complete Care Episodes Clinically based End to end redesign Lead with Quality Differentiated Clinical Capabilities Care Path Care Coordination Connected Care Clear Metrics Analytic capabilities Value Proposition: Complete Care Management Patient Centered Better patient decisions, less anxiety Least disutility of care, complications, pain Improved outcomes Physician Friendly More efficient care delivery Gain Sharing opportunities Better patient satisfaction, experience = referrals System resources deployed to free surgeon Health System Friendly Efficient use of resources Financially remunerative Attracts Physicians and Patients Next Steps: Additional CMS 48 Standard Bundles Acute myocardial infarction AICD generator or lead Hip & femur procedures except major joint Chest pain Lower extremity and Combined anterior humerus procedure posterior spinal fusion exept hip, foot, femur Other vascular surgery Stroke Pacemaker Pacemaker device replacement or revision Percutaneous coronary intervention Syncope & collapse Complex non-cervical Amputation spinal fusion Major bowel Transient ischemia Congestive heart Major cardiovascular Atherosclerosis failure procedure Urinary tract infection Major joint replacement of the Red blood cell Back & neck except COPD, lower extremity disorders spinal fusion bronchitis/asthma Major joint upper Removal of orthopedic CABG Diabetes extremity devices Double joint replacement of the Medical non-infectious Cardiac arrhythmia lower extremity orthopedic Renal failure Esophagitis, gastroenteritis and Medical peripheral Revision of the hip or other digestive Cardiac defibrillator disorders vascular disorders knee Fractures femur and Nutritional and Cardiac valve hip/pelvis metabolic disorders Sepsis Gastrointestinal Other knee procedures Simple pneumonia and Cellulitis hemorrhage respiratory infections Spinal fusion (nonCervical spinal fusion GI obstruction Other respiratory cervical) Lessons Learned Based on Early Experience • Physicians embrace key leadership role in episode management—drivers of change • Financial opportunities to gain share • Embrace change and opportunity: competitive advantage • Patients Benefit Care Redesign Patient Engagement Quality Improvement Cost Reduction Thank You Regional Hospitals March 3, 2015 l 59