* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Butz AM, Eggleston P, Huss K, Kolodner K, Vargas P, Rand C. Children with asthma and nebulizer use: parental asthma self-care practices and beliefs. J Asthma. 200;38(7): p.565-73.
Transnational child protection wikipedia , lookup
Child migration wikipedia , lookup
Child protection wikipedia , lookup
Child Protective Services wikipedia , lookup
Unaccompanied minor wikipedia , lookup
Electronic prescribing wikipedia , lookup
Diseases of poverty wikipedia , lookup
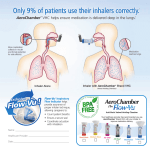
Journal of Asthma, 38(7), 565–573 (2001) ORIGINAL ARTICLE Children with Asthma and Nebulizer Use: Parental Asthma Self-Care Practices and Beliefs Arlene M. Butz, Sc.D., R.N.,1,2 Peyton Eggleston, M.D.,1 Karen Huss, D.N.Sc., R.N., F.A.A.N.,2 Ken Kolodner, Ph.D.,4 Perla Vargas, Ph.D.,5 and Cynthia Rand, Ph.D.3 1 School of Medicine, Department of Pediatrics, 2School of Nursing, and Pulmonary Medicine Department, The Johns Hopkins University, Baltimore, Maryland 4 Innovative Medical Research, Inc., Baltimore, Maryland 5 Department of Pediatrics, The University of Arkansas for Medical Sciences, Little Rock, Arkansas 3 ABSTRACT We examined demographic characteristics, patterns of medication use, asthma morbidity, and asthma self-management practices and beliefs among inner-city children currently using a nebulizer. We also describe the relationship between asthma self-management practices and beliefs and anti-inflammatory (AI) therapy. We observed a high rate of morbidity, including frequent emergency room visits, hospitalizations, symptom days and nights, and school absences in this group of school-aged children with asthma. More than three-quarters (81%) reported asthma symptoms consistent with mild persistent or greater severity of asthma, and therefore these subjects should be taking AI medications. Another 16% (36 of 231) of these children reported symptoms consistent with mild intermittent asthma. Only 1 out of 7 children in this study reported taking AI medications. We found that parents of children taking daily AI medications were more likely to agree with the belief that children should use asthma medications daily even when the child is not reporting any symptoms. Address correspondence to Arlene M. Butz, Sc.D., R.N., Department of Pediatrics, Johns Hopkins University, School of Medicine, 600 N. Wolfe Street, Baltimore, MD 21287-3144. E-mail: [email protected] 565 Copyright # 2001 by Marcel Dekker, Inc. www.dekker.com 566 Butz et al. KEY WORDS: Anti-inflammatory medications; Asthma; Asthma self-management; Nebulizer use. INTRODUCTION Nebulizers are medication delivery systems commonly used to deliver inhaled medications to infants and young children who are unable to use a metereddose inhaler (MDI) and/or to children with severe, symptomatic asthma. Aerosolized delivery of medications, either by MDI or a nebulizer, is ideal for asthma because drug delivery to the small airway is maximized and undesirable systemic effects are generally minimized (1). Studies indicate that there is no difference in efficacy between an MDI with spacer and a nebulizer when used for administration of inhaled albuterol to older children with mild to severe asthma (2–7). When there is difficulty in coordinating inspiration with MDI actuation, particularly in acutely ill children or dyspneic children with asthma, home nebulizer use is favored (8). Current National Asthma Education Prevention Program (NAEPP) Guidelines recommend nebulizer use for children less than 2 years of age and patients unable to use an MDI with spacer (9), yet the role of the nebulizer within guideline-based asthma management is unclear. Consistent with reports of others (10), we found high rates of nebulizer use observed in an inner-city school-age population with asthma (11). Approximately 45% of children enrolled in a communitybased asthma study reported having a nebulizer in the home and 33% of these school age children reported regular use of a nebulizer, defined as at least 1 or more days within the last month, in the management of their asthma (11). Although nebulizers appear to be an important component of asthma management practice within inner-city communities, little is known regarding how nebulizers are integrated into the overall asthma therapy of inner-city children with asthma. Current NAEPP guidelines recommend long-term control medications in addition to the quick-relief medications for the treatment of asthma in children with persistent moderate to severe asthma (9). Antiinflammatory (AI) medications (e.g., inhaled corticosteroids or cromolyn) are the most effective long-term control medications recommended for use in treatment of moderate persistent to severe persistent asthma in children (12). Underuse of AI medications has been associated with increased hospitalization rates (13) and may place these children at risk for increased morbidity and mortality (14). Several studies have reported physician nonadherence (either failure or resistance) with the NAEPP prescribing guidelines recommending the use of AI medication in children with persistent asthma. In addition, child nonadherence with AI use has been reported in multiple studies (15–17). Patient and caregiver beliefs have been suggested to be one contributing factor in AI medication poor adherence or refusal, either with MDI and spacer, or by nebulizer delivery. There are no data describing the asthma management practices and beliefs of parents of inner-city children with mild or moderate persistent to severe persistent asthma who use a nebulizer for administration of their medication. Understanding the practices and beliefs of these families may improve adherence with prescribed asthma medication therapy. The objectives of this study were to describe the patterns of asthma nebulizer medication use, morbidity, asthma management and beliefs, and the relationship between asthma management practices and beliefs and AI therapy in a group of caregivers of children with mild persistent to severe asthma who currently use nebulizers. METHODOLOGY This study was a cross-sectional design using baseline data collected from parents/caregivers of children with asthma enrolled in two communitybased asthma intervention studies in Baltimore, MD, and Washington, DC. The two studies used identical sample selection, subject identification, and data collection instruments. The first study (Community Based Adherence Intervention for African-American Children with Asthma) tested the effectiveness of a school-based asthma education and community health worker intervention on reducing emergency room visits, hospitalizations, and school absences, and promoting asthma care practices (18). The second study (Aþ Asthma Partnership for Minority Children with Asthma) examined the effectiveness of a community physician educational program on Parental Asthma Self-Care Practices 567 Criteria for inclusion were doctor-diagnosed asthma based on parent and school health record reports and self-report of nebulizer use at least 1 or more days within the last month for the past 6 months. Children participating in other asthma studies were excluded. Data were collected using a 170-item baseline questionnaire that included questions in five domains: sociodemographic, asthma morbidity, health care utilization (asthma as well as primary care), asthma medication use, and asthma self-care management practices. Nebulizer use was ascertained by asking, ‘‘Do you have a nebulizer (a special machine that gives prescribed medicines) in your home for your child’s asthma?’’ and ‘‘How many times in the last 30 days did you use the nebulizer (mist machine) for your child’s asthma?’’ Children were defined as nebulizer users if they reported use of a nebulizer at least 1 or more days per month during the last 6 months. Assessment of asthma morbidity included number of symptom (cough or wheeze) days and nights in the last 6 months, number of school absences due to asthma in the last 12 months, number of times oral steroids were taken in the last 12 months and past 30 days, and current use of oral steroids. Healthcare utilization items included the number of hospitalizations in the child’s lifetime and in the last 6 months, the number of emergency department visits in the child’s lifetime and in the last 6 months, and the number of physician visits for regular asthma care in the last 12 months. Asthma medication use was assessed using items asking name of asthma medication, frequency of use, and mode of medication administration (i.e., oral or inhaled) at present and during the last 6–12 months. Assessment of asthma management included (a) practices, such as peak flow meter use or allergy skin test performed; (b) beliefs about side effects of asthma medications, and taking asthma medications daily without symptoms; and (c) satisfaction with child’s medical care. Measures Data Analysis Baseline study data were obtained via telephone interview after obtaining written parental/legal guardian consent and child assent. The 30-min telephone survey was conducted by professional interviewers from June 1994 to June 1998 of families of children with asthma enrolled in either study. Families without telephones or those who could not be contacted were mailed a card with a toll-free number to call, which linked them to an interviewer who administered the interview. Families without telephones were sent a $20.00 incentive after completion of the interview. Data were summarized by examining frequency distributions for all sociodemographic, asthma morbidity, healthcare utilization, asthma medication, and asthma management variables for all 231 participants who were currently using nebulizers. Categories of asthma medications were created by examining the pattern of medication use across all participants and were collapsed into the five most common patterns: (a) b-adrenergic agonist and/or theophylline only; (b) b-adrenergic agonist and cromolyn theophylline; (c) inhaled corticosteroids and b-adrenergic agonist cromolyn or inhaled corticosteroids and increasing asthma management knowledge and skills of community physicians and reducing emergency room visits and hospitalizations in inner-city children with asthma. Both intervention studies were approved by the Institutional Review Boards of the Johns Hopkins Medical Institutions, Baltimore, MD, and the Howard University College of Medicine, Washington, DC. Parental consent and child assent were obtained for each child enrolled in the community-based studies. Subjects A total of 686 children, 6–12 years old, were identified with physician-diagnosed asthma from 42 elementary schools from September 1992 through June 1996. Of the 686 children, almost half (312 children, 45%) reported having a nebulizer machine in the home and 231 of these children or 74% (231 of 312) reported current nebulizer use at least 1 or more days within the last month for the past 6 months for which results are presented (11). We previously reported on nebulizer use among innercity children with asthma (11). This paper presents additional data on self-care practices and asthma health beliefs among children with asthma who are currently using a nebulizer. Inclusion Criteria 568 Butz et al. theophylline cromolyn; (d ) inhaled corticosteroid only or in combination with cromolyn, or cromolyn only; or (e) no medication. Children using inhaled corticosteroids or cromolyn sodium were further classified as inhaled AI users. No children reported using leukotriene modifier medications. Bivariate analyses of AI users were examined using w2 analysis for the categorical variables (i.e., use of peak flow meter and asthma management beliefs) and Student’s t-test for the continuous variable of mean number of visits to physician for regular asthma care in the past 12 months. Differences in asthma morbidity measures and asthma management characteristics were analyzed by use of inhaled AI (use of AI medication versus no AI use). All data analysis was conducted using SAS 7.0 (19). RESULTS Child and Parent Characteristics Children were primarily male (62%), African American (97%), and had a mean age of 7.9 years (range 5–12 years) (Table 1). Most respondents (89%) were the child’s biological parent (i.e., mother or father). Most parents (76%) reported at least a high school education or graduate equivalency diploma (GED). More than one-third (42%) reported five or more people living in the household. Table 1 Child and Parent Sociodemographic Characteristics (N ¼ 231) Characteristic Child sociodemographic characteristics Gender Male Female Race/ethnicity African American Caucasian/other Age in years 5–6 7–8 9–10 11þ Parent sociodemographic characteristics Parent education <High school High school graduate/GED Some college/technical Missing Number of household members 2 3–4 5–6 7þ Type of health insurance Medical assistance plan Family income/year <$10,000 $10,000–20,000 >$20,000 Receive AFDC in past 12 months Yes Number (%) 144 (62.3) 87 (37.7) 224 (96.9) 7 (3.1) Mean ¼ 7.9 (SD 1.9) 61 (26.4) 78 (33.8) 70 (30.3) 22 ( 9.5) 54 (23.4) 123 (53.2) 53 (22.9) 1 (0.4) 19 (8.2) 113 (48.9) 80 (34.6) 19 (8.2) 152 (65.8) 95 (41.1) 59 (25.5) 73 (31.6) 124 (53.6) Parental Asthma Self-Care Practices 569 Although most mothers (79%) reported they did not have asthma, more than half (54%) reported other family members with asthma. Two-thirds reported medical assistance as the child’s type of medical insurance, and half (54%) reported receiving Aid to Families with Dependent Children (AFDC) or welfare. cromolyn sodium use in combination with b-adrenergic agonist with and without theophylline. Inhaled corticosteroid use either alone or in combination with a bronchodilator was low (35 of 231, 15%) as recommended by the NAEPP guidelines (9). Type of medication use was missing for 6% of the subjects. Asthma Morbidity Pattern of Asthma Medication Use As seen in Table 2, use of a b-adrenergic agonist medication alone or in combination with theophylline was the predominant (46%) type of asthma medication use. One third of the children reported As seen in Table 3, approximately one-quarter (26%) of the children reported a hospitalization, more half (57%) reported 15 or more symptom days and nights during the last 6 months, and almost one-third (30%) reported missing 11 or more school Table 2 Pattern of Medication Use ( N ¼ 231) Excluding Short-Burst Oral Steroid Use Medication Number (%) b-Adrenergic agonist and/or theophylline only b-Adrenergic agonist þ cromolyn theophylline Inhaled steroid þ b-adrenergic agonist cromolyn or inhaled steroid theophylline cromolyn Inhaled steroid only or cromolyn Cromolyn only None or missing 105 (45.5) 76 (32.9) 32 (13.8) 3 (1.3) 2 (0.9) 13 (5.6) Table 3 Asthma Morbidity for Children Using Nebulizers ( N ¼ 231) Characteristic Hospitalized during the last 6 months Yes Number days and nights symptoms last 6 months 1–15/month 15þ/month Number school days missed during last year None 1–5 days 6–10 days 11 þ days Missing Number emergency room visits in last 6 months None 1–2 3þ Number of nebulizer treatments in past 30 days Number of times oral steroid (daily or as-needed) used in past 12 months Number (%) 60 (26.0) 99 (42.9) 132 (57.1) 37 (16.0) 67 (29.0) 55 (23.8) 70 (30.3) 2 (0.9) 60 (26.0) 85 (36.8) 86 (37.2) Mean (SD) 23.5 (30.2) 3.4 (7.0) 570 days during the last year. More than one-third (37%) reported three or more emergency room visits within the last 6 months. The mean number, standard deviation (SD), and median of nebulizer treatments used within the last 30 days was 23.5 times (SD ¼ 30.2; median ¼ 6) and the mean number of times oral steroids were taken during the past 12 months was 3.4 (SD ¼ 7.0; median ¼ 2). Asthma Morbidity by Inhaled AI Use Children reporting taking inhaled AI medications, defined as any cromolyn sodium or inhaled corticosteroid, had increased morbidity as evidenced by a significantly higher rate of a hospitalization in the past 6 months (AI users, 34.5% and AI nonusers, 17.8%; w2 ¼ 8.39, df ¼ 1, p ¼ 0.004); higher number of days and nights with symptoms (greater than 15 days and nights per month: AI users, 65% and AI nonusers, 50%; w2 ¼ 5.03, df ¼ 1, p ¼ 0.03); more children with three or more emergency department visits in the last 6 months (AI users, 45% and AI nonusers, 30%; w2 ¼ 5.96, df ¼ 2, p ¼ 0.05); and higher mean number of nebulizer treatments in the last 30 days (AI users, 31.8 times and AI nonusers, 15.5 times; t-test ¼ 4.25, df ¼ 216, p ¼ 0.0001). There were no significant differences in the number of times oral steroids were used in the past 12 months or number of school days missed by use of inhaled AI medications. Asthma Management and Beliefs by Inhaled AI Use As seen in Table 4, children reporting taking inhaled AI medications reported having a peak flow meter in the home significantly more often ( p ¼ 0.001) than did noninhaled AI users. The two groups did not differ regarding number of physician visits for regular asthma care in the past 12 months, having a regular source of asthma care, or receiving allergy skin testing. Few caregiver beliefs about asthma care differed by use of inhaled AI medications. Significantly more parents of inhaled AI users reported that they agree that ‘‘children should take asthma medications daily even when they have no symptoms’’ ( p ¼ 0.001), and reported that they disagree or strongly disagree that ‘‘doctors don’t care if patients worry’’ ( p ¼ 0.02). There were no differences by inhaled AI use in the parent’s beliefs of ‘‘satisfaction with medical care for Butz et al. my child,’’ ‘‘physician explains what medications do and how to use them,’’ ‘‘physicians always treat their patients with respect,’’ ‘‘medical care for my child could be better,’’ or ‘‘my beliefs about my child’s care conflict with the beliefs of my child’s doctor.’’ Most caregivers (92%–96%) agreed or strongly agreed that they were very satisfied with the medical care for their child. However, almost one-third of parents in both groups reported that their beliefs about their child’s care did conflict with their doctor’s beliefs (noninhaled AI users: 32%; inhaled AI users: 29%). DISCUSSION We observed a high rate of morbidity in children with asthma who currently used nebulizers, including frequent emergency room visits, hospitalizations, symptom days and nights, and school absences. Despite the fact that the majority of children reported asthma symptoms consistent with persistent asthma and 74% reported an emergency room visit in the prior 6 months, very few children (15%) in this study reported taking AI medications. Although this is contrary to NAEPP guidelines (9), it is consistent with previous reports of low AI use in inner-city pediatric populations (15). This lack of inhaled AI therapy may be a major contribution to poor asthma control (20–22) as evidenced in this sample. Our data indicate serious undertreatment of an identified high-risk group of children with asthma based on current use of a nebulizer. It is unclear if this low inhaled AI use is a result of physicians not following clinical practice guidelines (23), or the family’s failure to fill or adhere to prescribed medications (24–27). Considerable failure to refill medication was shown in one pediatric asthma study in which 63% of caregivers reportedly were out of albuterol for their child when the child presented to the emergency room (26). The low use of AI medication is of great concern, particularly considering the high morbidity we observed in this study.Alternatively, it is possible that AI therapy was prescribed only to children with the more severe asthma. Regardless of the reason for lack of AI use, it remains a concern that these children experienced increased morbidity. These findings indicate the urgent need for increased attention Parental Asthma Self-Care Practices 571 Table 4 Parental Asthma Management Practices and Beliefs by Inhaled AI Use ( N ¼ 231) No Inhaled AI (N ¼ 118) Mean (SD) Inhaled AI Use (N ¼ 113) Mean (SD) 4.5 (7.6) 5.3 (6.2) t-test ¼ 0.86, df ¼ 221, p ¼ 0.39 Number (%) Number (%) p Value 40 (35.1) 74 (64.9) 66 (60.0) 44 (40.0) w2 ¼ 13.94, df ¼ 1, p ¼ 0.001 115 (97.5) 3 (2.5) 112 (99.1) 1 (0.9) w2 ¼ 0.30, df ¼ 1, p ¼ 0.58 48 (42.1) 66 (57.9) 59 (54.6) 49 (45.4) w2 ¼ 3.03, df ¼ 1, p ¼ 0.08 48 (42.9) 64 (57.1) 80 (77.7) 23 (22.3) w2 ¼ 26.9, df ¼ 1, p ¼ 0.001 22 (18.6) 76 (64.4) 20 (17.7) 13 (11.5) 91 (80.5) 9 (8.0) w2 ¼ 7.73 df ¼ 2, p ¼ 0.02 109 (92.3) 4 (3.4) 5 (4.3) 108 (95.6) 3 (2.7) 2 (1.7) w2 ¼ 1.32 df ¼ 2, p ¼ 0.52 96 (82.8) 11 (9.5) 8 (6.8) 1 (0.9) 99 (87.6) 10 (8.8) 3 (2.7) 1 (0.9) w2 ¼ 2.33, df ¼ 3, p ¼ 0.51 93 (78.8) 100 (88.5) w2 ¼ 4.92, df ¼ 2, p ¼ 0.09 Disagree/strongly disagree Not sure Medical care for my child could be better Strongly agree/agree 15 (12.7) 10 (8.5) 10 (8.8) 3 (2.7) 59 (50.0) 45 (39.8) Disagree/strongly disagree Not sure My beliefs about my child’s care conflict with the beliefs of my child’s doctor Strongly agree/agree 45 (38.1) 14 (11.9) 54 (47.8) 14 (12.4) 38 (32.2) 32 (28.3) 68 (57.6) 12 (10.2) 72 (63.7) 9 (8.0) Asthma Care Practices Number of visits to doctor for regular asthma care in past 12 months Peak flow meter in the home Yes No Child has regular source of asthma care Yes No Received allergy skin testing (N ¼ 222) Yes No Statistical Test and p Value Asthma Care Beliefs Children should take asthma medications daily even when they have no symptoms? Yes No Doctors don’t care if patients worry Strongly agree/agree Disagree/strongly disagree Not sure I am very satisfied with the medical care for my child Strongly agree/agree Disagree/strongly disagree Not sure Physician explains what medications do and how to use them All of the time Most of the time Some of the time None of the time Physicians always treat their patients with respect Strongly agree/agree Disagree/strongly disagree Not sure w2 ¼ 2.59, df ¼ 2, p ¼ 0.27 w2 ¼ 1.27, df ¼ 2, p ¼ 0.53 572 to both provider and patient education regarding preventive therapy. Our data also suggest that patient beliefs may play an important role in the use of controller medication. We found that parents of children reporting use of daily AI medication were more likely to agree that children should take asthma medications daily (even when they had no symptoms) as compared to parents of children not reporting use of AI therapy. AI medication use was more likely to be reported by children with more severe disease (e.g., higher number of days and nights with symptoms). Parental misunderstanding of the rationale of regular prophylactic therapy includes either unconvincing evidence of the benefits of AI medications or fear of the side effects of the AI medications (22). This suggests that targeting parent’s beliefs about daily asthma medication use, despite the lack of evident symptoms in their child, is critical to increasing adherence to AI therapy for children. Some evidence exists that this subgroup of children taking AI medications demonstrated a pattern of receiving more NAEPP guideline-based management including a greater likelihood of having a peak flow meter. Of concern is the finding that almost one-third of all nebulizer users reported conflict between themselves and the physician’s beliefs about the care of their child. We were unable to determine if this conflict is related to nebulizer or medication use or other aspects of their child’s medical care. This study’s findings should be interpreted with some caution. This study relied upon a structured parental interview rather than clinical records, so it is likely that parental reports of asthma morbidity are subject to recall bias. In addition, all surveyed families had consented to participating in a schoolbased or a home-based asthma education program. Therefore, this sample might be biased toward families that are either more concerned about their child’s asthma or more in need of asthma education and services. However, the asthma morbidity and healthcare utilization baseline data found in this intervention study are remarkably similar to other inner-city asthma surveys that did not enroll participants in an asthma intervention (28,29). Another caveat with our self-reported data is that we are unable to determine if a medication was not prescribed or whether there was poor adherence with a prescribed treatment plan. However, families were asked to obtain all of their child’s medications at the beginning of the interview so that the parent Butz et al. could read the label for medication name and instructions for use. CONCLUSIONS We observed a high rate of morbidity, including frequent emergency room visits, hospitalizations, symptom days and nights, and school absences in a group of school-aged children with asthma who were currently using nebulizers. More than threequarters (81%) reported asthma symptoms consistent with mild or greater persistent asthma, yet only 1 out of 7 children reported taking AI medications. In addition, we observed that parents’ beliefs about the value of long-term controller medication use were associated with the use of AI medication. Further studies need to carefully evaluate the value of nebulizer delivery systems in the management of persistent asthma, its effect on adhering to AI medication use (i.e., if the reliance of children on nebulizer therapy discourages adherence to AI medication use), and the factors determining underuse of AI medication in these high-risk children. ACKNOWLEDGMENT This research was supported by the National Heart, Lung, and Blood Institute, NIH Grant Nos. HL52013 and HL52833. REFERENCES 1. 2. 3. 4. 5. Lemanske, R.F.; Busse, W.W. Asthma. JAMA 1997, 278, 1855–1873. Karem, E.; Levison, H.; Schuh, S.; O’Brodovich, H.; Reisman, J.; Bentar, L.; Canny, G.J. Efficacy of Albuterol Administered by Nebulizer Versus Spacer Device in Children with Acute Asthma. J. Pediatr. 1993, 123, 313–317. Lewis, R.A.; Fleming, S.S. Fractional Deposition from a Jet Nebulizer: How it Differs from a Metered Dose Inhaler. Br. J. Dis. Chest 1985, 79, 361–367. Chou, K.J.; Cunningham, S.J.; Cramer, J. MeteredDose Inhalers with Spacers vs Nebulizers for Pediatric Asthma. Arch. Pediatr. Adolesc. Med. 1995, 149, 201–205. Freelander, M.; Van Asperen, P.P. Nebuhaler Versus Nebulizer in Children with Acute Asthma. Br. Med. J. 1984, 288, 1873–1874. Parental Asthma Self-Care Practices 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Lin, Y.Z.; Hsieth, K.H. Metered Dose Inhaler and Nebulizer in Acute Asthma. Arch. Dis. Child. 1995, 72, 214–218. Schuh, S.; Johnson, D.W.; Stephens, D.; Callahan, S.; Winders, P.; Canny, G.J. Comparison of Albuterol Delivered by a Metered Dose Inhaler with Spacer Versus a Nebulizer in Children with Mild Acute Asthma. J. Pediatr. 1999, 135, 22–27. Canny, G.J.; Levison, H. Aerosols: Therapeutic Use and Delivery in Childhood Asthma. Ann. Allergy 1988, 60, 11–20. National Asthma Education and Prevention Program. Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma, NIH Publication No. 97-4051; National Heart, Lung and Blood Institute, National Institutes of Health, Bethesda, MD, 1997. Neville, R.G.; Hoskins, G.; Smith, B.; Clark, R.A. How General Practitioners Manage Acute Asthma Attacks. Thorax 1997, 311, 153–156. Butz, A.M.; Eggleston, P.; Huss, K.; Kolodner, K.; Rand, C. Nebulizer Use in Inner-City Children with Asthma. Arch. Pediatr. Adolesc. Med. 2000, 154, 984–990. Kerrebijin, K.R.; van Essen-Zandvliet, E.E.; Neijens, H.J. Effects of Long-Term Treatment with Corticosteroid and b2-Agonist on the Bronchial Responsiveness in Children with Asthma. J. Allergy Clin. Immunol. 1987, 79, 653–659. Gottlieb, D.J.; Beiser, A.S.; O’Connor, G.T. Poverty, Race and Medication Use Are Correlates of Asthma Hospitalization Rates: A Small Area Analysis in Boston. Chest 1995, 108, 28–35. Strunk, R.C.; Mrazek, D.A.; Fuhrmann, G.S.; LaBreque, J.F. Physiologic and Psychological Characteristics Associated with Deaths Due to Asthma in Childhood. JAMA 1985, 254, 1193. Eggleston, P.A.; Malveaux, F.J.; Butz, A.M.; Huss, K.; Thompson, L.; Kolodner, K.; Rand, C.S. Medications Used by Children with Asthma Living in the Inner City. Pediatrics 1998, 101, 349–354. Milgrom, H.; Bender, B.; Ackerson, L.; Bowry, P.; Smith, B.; Rand, C. Noncompliance and Treatment Failure in Children with Asthma. J. Allergy Clin. Immunol. 1996, 98, 1051–1057. Coutts, J.A.; Gibson, N.A.; Paton, J.Y. Measuring Compliance with Inhaled Medications in Asthma. Arch. Dis. Child. 1992, 67, 332–333. 573 18. Rand, C.S.; Butz, A.M.; Huss, K.; Kolodner, K.; Eggleston, P.E. Emergency Department Utilization of Urban African-American Children with Asthma. J. Allergy Clin. Immunol. 2000, 105, 83–90. 19. SAS Institute. SAS Users Guide: Statistics, Version 7.0; SAS Institute: Cary, NC, 1999. 20. Newhouse, M.T. Emergency Department Management of Life-Threatening Asthma. Are Nebulizers Obsolete? Chest 1993, 103, 661–663. 21. Bender, B.; Milgrom, H.; Rand, C.; Ackerson, L. Psychological Factors Associated with Medication Nonadherence in Asthmatic Children. J. Asthma 1998, 35, 347–353. 22. Gibson, N.A.; Ferguson, A.E.; Aitchison, T.C.; Paton, J.Y. Compliance with Inhaled Asthma Medication in Preschool Children. Thorax 1995, 50, 1274–1279. 23. Cabana, M.D.; Rand, C.S.; Powe, N.R.; Wu, A.W.; Wilson, M.H.; Abboud, P.; Rubin, H. Why Don’t Physicians Follow Clinical Practice Guidelines? JAMA 1999, 282, 1458–1465. 24. Celano, M.; Geller, R.J.; Phillips, K.M.; Ziman, R. Treatment Adherence Among Low-Income Children with Asthma. J. Pediatr. Psychol. 1998, 23, 345–349. 25. Winkelstein, M.L.; Eggleston, P.E.; Huss, K.; Vargas, P.; Butz, A.; Rand, C. Factors Associated with Medication Self-Administration in Children with Asthma. Clin. Pediatr. 2000, 39, 337–345. 26. Simon, H.K. Caregiver Knowledge and Delivery of a Commonly Prescribed Medication (Albuterol) for Children. Arch. Pediatr. Adolesc. Med. 1999, 153, 615–618. 27. Vargas, P.; Rand, C.S. Concordance Between Patient Self-Reported and Physician Reported Asthma Regimen in Low-Income, Minority Children with Asthma. Am. J. Resp. Crit. Care Med. 1999, 159, A267. 28. Mak, H.; Johnston, P.; Abbey, H.; Talamo, R.C. Prevalence of Asthma and Health Service Utilization of Asthmatic Children in an Inner City. J. Allergy Clin. Immunol. 1982, 70, 367–372. 29. Fisher, E.B.; Sussman, L.K.; Arfken, C.; Harrison, D.; Munro, J.; Sykes, R.K.; Sylvia, S.; Strunk, R.C. Targeting High Risk Groups. Neighborhood Organization for Pediatric Asthma Management in the Neighborhood Asthma Coalition. Chest 1994, 106, 248S–259S. Copyright of Journal of Asthma is the property of Taylor & Francis Ltd and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.