* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ulcerative colitis
Onchocerciasis wikipedia , lookup
Meningococcal disease wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Chagas disease wikipedia , lookup
Oesophagostomum wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Schistosomiasis wikipedia , lookup
Leptospirosis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
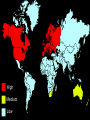
Inflammatory bowel diseases (I.B.D) IBD TWO MAIN FORMS: ULCERATIVE COLITIS- AFFECTS LARGE BOWEL ONLY CROHN’S DISEASE- AFFECTS ANY PART OF GIT Epidemiology of IBD Incidence (US) Age of onset Male:female ratio Smoking Oral contraceptive Ulcerative colitis Crohn’s disease 11/100 000 7/100 000 15-30 & 60-80 15-30 & 60-80 1:1 1,1-1,8:1 May prevent disease May cause disease No increased risk Relative risk 1,9 Appendectomy Not protective Protective Monozygotic twins 8% concordance 67% concordance High Medium Low Epidemiology UC ► Highest incidence in Europe, United Kingdom, North America Incidence per person-years 2.2–14.3/100,000 Age of onset 15–30 & 60–80 Male:female ratio 1:1 Smoking May prevent disease Oral contraceptives No increased risk Appendectomy Protective Monozygotic twins 6% concordance Dizygotic twins 0% concordance Epidemiology Crohn,s disease Incidence: 7/100 000 pop/yr World wide distribution but more common in the West. The incidence is lower in non-white races. Females are affected more than males 1.2:1 Epidemiology Jews are more affected than non-Jews Bimodal age distribution: 20-40 yrs/60-80 yrs Prevalence: 100/100 000 pop/yr The incidence is rising Etiology ► Genetic ► Defective immune regulation ► Exogenous factors Etiology & Pathogenesis The aetiology of IBD disease is unknown. There are many proposed pathogenic mechanisms, some of which are represented in this diagram. Genetic susceptibility Environmental factors Host Immune Response IBD As there is no one cause, it is likely that IBD disease is an outcome of interactions between genetic predisposition, environmental factors and the subsequent reaction of the host immune system. Genetic: ► IBD patients have disease-associated foci on chromosome 16, 12,7,5,3,1 (gene NOD-2) ► Ulcerative colitis express HLA DR2 and CD express DR5 DQ1, DRB0301. ► IBD patients with HLA DRB10130, have extensive disease and extraintestinal manifestation such as : mouth ulcers,arthritis,uveitis Immune dysregulation in IBD NORMAL normal IBDIBD Antigen and flora Antigen and flora Dysregulation ? CD4+ T Inhibitory cytokines IL-10,TGF-b CD-TH1 CD -TH2 IL-4,IL5,IL13 ING- ,TNF Inflammatory cytokines Oral tolerance Crohn,s colitis Ulcerative colitis Pathology Ulcerative colitis : (1)Is a mucosal disease of colon (2) 40-50% involve rectum ,30-40% rectosigmoid ,20% pancolitis (3) Backwash ileitis :10-2%% (4) Mucosa is erythematous , hemorrhage ,ulcerations , pseudopolyps Pathology( crohn,s): ► Affect any part of GI from mouth to anus ► 30-40% small bowel ► 40-55% small and large bowel ► 15-25% alone colitis,” cobblestone” ► 90% terminal ileum is involved ► is a transmural disease with skip area , rectum is spared ,preanal lesion like fistula ,fissures , abcesses,anal stenosis in see in 30%. Normal colon ULCERATIVE COLITIS CONTINUOUS INVOLVEMENT CROHNS vs PM COLITIS Clinical: ► Intestinal ► Extraintestinal Ulcerative colitis Disease distribution Ulcerative Colitis Left sided cloitis Proctitis Proctosigmoiditis Disease distribution ► The disease typically is most severe distally and progressively less severe more proximally. ► In contrast to Crohn's disease, continuous and symmetrical involvement is the hallmark of UC, with sharp transition between diseased and uninvolved segments of bowel Clinical Features diarrhea tenesmus rectal bleeding passage of mucus urgency abdominal pain Clinical Features The onset of UC typically is slow and insidious. Symptoms have usually been present for weeks or months by the time the patient seeks medical attention. The median interval between the onset of symptoms and diagnosis of UC is approximately 9 months. Some patients with UC may present much more acutely, with symptoms mimicking infectious colitis. Intestinal symptoms of UC ► Diarrhea, rectal bleeding ,tenesmus, passage of mucus crampy pain, incomplete evacuation. ► Intestinal complications : bleeding, toxic colon, perforations , obstructions Intestinal symptoms of CD : ► Ileocolitis : diarrhea and chronic RLQ pain ► Jejunoileitis :malabsorption ► Colitis :diarrhea, low grade fever,pain, some times hematochezia ► Gastroduodenal : G.O.O ► Intestinal complications :fistula, perforation, intestinal obstruction, hemorrhage, preanal diseases. Extraintestinal Manifestations of IBD Skin Erythema nodosum Pyoderma gangrenosum Joints Peripheral arthritis Sacroileitis Ankylosing spondylitis Eye Uveitis Episcleritis Iritis Hepatobiliary complications Gallstones PSC Renal complications Nephrolithiasis Recurrent UTIs Extraintestinal complications of I.B.D Oral : Dermatologic : (1)Erythema nodosum, CD, 15% (2)Pyoderma gangrenosum , UC ,1-12% Extraintestinal complications of I.B.D Rheumatologic : (1)Peripheral arthritis, CD,15-20% (2)Ankylosing spondylitis : CD, 10%, and 2/3 have positive test fir HLA-B27,no relation to activity (3)Sacroiliitis :CD=UC, No relation to activity Extraintestinal complications of I.B.D Ocular :1-10% (1)Conjuntivitis (2)Anterior uveitis/iritis (3)Episcleritis Extraintestinal complications of I.B.D Hepatobiliary: (1)Hepatic steatosis :50% (2)Cholelithiasis : CD>UC is seen in 10-35% patients with ileitis (3) Primary sclerosing cholangitis :1-5%of I.B.D patients have PSC 50%-75 of patients with PSC have I.B.D (4)Peicholangitis : Extraintestinal complications of I.B.D Urologic : (1)Calculi :CD, 10-20% (2)Ureteral obstruction (3)fistula Lab in IBD ► In ESR,CRP, Hb ► PANCA :Is positive in 5% population, 5-10% in first degree relatives 5-10% in CD , 6070% in UC ► ASCA : 5% Population ,10-15% in UC, 6070% in CD ► ANCA positivity is more associated with pancolitis, early surgery, pouchitis, PSC. Medical treatment (1)Sulfasalazine Adverse Effects of Sulfasazine Dose related ► nausea ► vomiting ► anorexia ► folate malab. ► Headache ► alopecia Not dose related ► skin rash ► hemolytic anemia ► agrannulocytosis ► fibrosing alveolitis ► hepatitis ► male infertility ► colitis Newer therapy: (2) 5-ASA a-azo-band : olsalazine b-5-ASA dimer(resin) :delayed release, pH dependent , Asacol c: sustained released: ethylcellulose microgranules , PENTASA Treatment (continuous): (3)Glucocorticoids : a-oral b-Iv c-suppository and enema (4) Antibiotics : metronidazole, ciprofloxacin. fistula , preanal lesions (5)Azthioprine,,methotrexate,cyclosporine(iv dose2-4mg/kg 82% effective in UC refractory to therapy ) 6-MP (6)Anti-TNF antibody (infliximab) : dose 5mg/kg ,65% of refractory CD respond,repeat every 8 weeks. Treatment protocol is based in two factors: ► Colonic ► DAI involvement extent Disease distribution Ulcerative Colitis Left sided cloitis Proctitis Proctosigmoiditis FACTORS MODIFYING RISK Cancer risk in IBD: OF COLITIS-ASSOCIATED CANCER Primary sclerosing cholangitis Family history of colorectal cancer pseudopolyp Cancer in I.B.D Sporadic colonic cancer (SCC) arise from adenomatous polyp; colitis associated colonic cancer(CACs ) arise from flat dysplasia or dysplasia-associated lesion or mass (DALM) ► Multiple synchronous cancers occurs in3-5% SCC and in 12% CAC ► Mean age SCC is 60 and CAC 30 years ► SCC exhibits a left- sided predominance ,CAC distribute uniformly ► Mucinous and anaplastic cancers are more common in CAC than SCS ► Inflammatory bowel diseases & pregnancy ► Patients with quiescent UC and CD have normal fertility rates ► With increased activity patients have chance of abortion , stillbirths and developmental defects, but not due to medications ► Antibiotics like ampicillin, cephalosporin,ormetronidazole for short courses are safe ► Methotrexate and ciprofloxacin are contraindicated ► Sulfasalazine , 5-ASA and Glucocorticoids are safe Indications for surgery: Ulcerative colitis Intractable disease Fulminant disease Toxic megacolon Colonic perforation Massive colonic hemorrhage Extracolonic disease Colonic obstruction Colonic cancer Crohn,s disease CD of small intestine: Stricture,obstruction,fistula Refractory to medical therapy Abscess CD of colon and rectum: Intractable Preanal disease,fistula, obstruction refractory to therapy cancer