* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Pharmaceutical Care III Fall 2007
Adherence (medicine) wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug design wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug discovery wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Theralizumab wikipedia , lookup
Tablet (pharmacy) wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
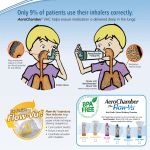
Pharmaceutical Care III Management of Asthma Angela Singh, PharmD Assistant Professor of Pharmacy Practice Florida A&M University College of Pharmacy Overview of Asthma • Inflammatory disease characterized by hyperresponsiveness of the airways. • Inflammatory mediators include prostaglandins, histamine and leukotrienes. • Inflammation results in bronchial smooth muscle spasms, vascular congestion, increased vascular permeability, mucous production and impaired ciliary function. Case • Chief Complaint – I have become increasingly short of breath over the past few weeks. • HPI – B.W is a 20 year-old woman who attends the university, majoring in business. She comes to the clinic today because she has noticed that she has been using her albuterol inhaler more frequently (3 to 4 times a week) and has also been experiencing symptoms at night more frequently (3 times/month). Case • SH – Denies any use of tobacco, consumes 10-12 drinks per week, usually on the weekends, drinks one Coke daily and denies any use of illicit drugs. • PE – Occasional expiratory wheezes bilaterally • Diagnostic Tests – Peak expiratory flow variability is 25% and her FEV1 is 85%. Current Medications • Albuterol inhaler 2 puffs q 4 hours as needed for shortness of breath and/or wheezing. • Ortho Novum as directed monthly. • Propranolol 40 mg twice daily • St. John’s Wort 300 mg three times daily. Categories of Asthma • Extrinsic/Allergic • Intrinsic Etiology • Innate Immunity • Genetics • Environmental Factors Pathophysiology • Acute Inflammation – Early response – Delayed Response • Chronic Inflammation • Bronchoconstriction • Airway Hyperresponsiveness • Airway Edema Key Symptoms of Asthma • Wheezing • History of any of the following – Cough – Recurrent wheeze – Recurrent difficulty in breathing – Recurrent chest tightness • Symptoms occur or worsen at night, awakening the patient • Symptoms occur or worsen in the presence of – Exercise – Viral infection – Inhalant allergens – Irritants – Changes in weather – Strong emotional expression – Menstrual Cycles Co-Morbid Conditions that may Worsen Asthma • • • • • GERD Obesity Obstructive Sleep Apnea (OSA) Rhinitis Stess/Depression Diagnosis • Medical History • Physical Examination • Spirometry – Forced Vital Capacity (FVC) – Forced Expiratory Volume in one second (FEV1) – FEV1 / FVC ratio Diagnostic Tests • FEV1/FVC ratio • Peak Flow Meters • Bronchoprovocation Test Peak Flow Meters Complications • Acute • Chronic Asthma Severity Classification Classification Mild Intermittent Mild Persistent Moderate Persistent Severe Persistent Frequency of Symptoms < 2 days/week > 2 days/week Daily Continual Night Time Symptoms <2 nights/month >2 nights/month > 1 night/week Frequent Peak Expiratory Flow Variability < 20% 20-30% > 30% > 30% Forced Expiratory Volume in 1 second > 80 % > 80% 60% to 80% < 60% Case • Based on her presentation how would you classify her asthma? Treatment Goals • Prevent chronic and troublesome symptoms • Require infrequent use of inhaled SABA (< 2 times per week) for quick relief of symptoms (not including prevention of exercise-induced bronchospasm (EIB)) Non-Pharmacological Approaches • Immunizations – Influenza vaccine – Doesn’t prevent asthma exacerbations during flu season • Allergen avoidance • Tobacco smoke, dust mites, animal dander, cockroach, pollen, mold, exercise • Education of the parents and the child. Education • Basic facts about asthma • Role of Medications • Patient Skills – Taking medications correctly – Identifying and avoid environmental exposures – Self Monitoring – Asthma Action Plan How to administer an inhaler… • Take off the cap and shake the inhaler • Breath out all the way • Hold your inhaler one of the following ways – Hold inhaler 1 to 2 inches in front of your mouth (about the width of two fingers) – Use a spacer/ holding chamber. These come in many shapes and can be useful to any patient. – Put the inhaler in your mouth. • Breathe in slowly • As you start breathing in slowly through your mouth, press down on the inhaler one time (If you use a holding chamber, first press down on the inhaler. Within 5 seconds, begin to breathe in slowly. • Keep breathing in slowly, as deeply as you can. • Hold your breath • Hold your breath as you count to 10 slowly, if you can. • Wait about 1 minute between puffs. Tips for Using an Inhaler • • • • • Rinse mouth with water or mouth wash after using corticosteroid medication to prevent hoarseness and fungal infections in the mouth and throat. If you are taking more than one inhaled medication, it is important to take them in the correct order. Bronchodilating medications are usually taken first to open the airways and allow other types of medications to be more effectively inhaled into the lungs. Corticosteroids and cromolyn are inhaled after bronchodilating drugs. Avoid the use of over-the-counter inhalers. Most of these contain epinephrine, which is effective for only a short time and may cause rebound bronchospasm (making it more difficult to breathe). Take only the recommended number of puffs prescribed by your provider; over-use or incorrect use can be dangerous. Notify your doctor if any of the following occur: – You do not get relief from your metered dose inhaler – You have increasing shortness of breath despite use of inhalers – You are experiencing weakness, increased heart rate, shakiness, insomnia, nervousness, headaches, nausea or vomiting CFC vs HFA Inhalers • Due to the Clean Air Act Chlorofluorocarbon (CFC) inhalers are being phased out of the market and replaced with hydrofluroalkane (HFA) inhalers. • These inhalers require different instructions for priming, storage and use. Pharmacologial Approaches • • • • • • Beta Agonists Corticosteroids Leukotriene Modifiers Mast Cell Stabilizers Theophylline Monoclonal Antibodies Short Acting Beta Agonists (SABA) Used for the Prevention and TREATMENT of Bronchospasms Brand Name Generic Name Formulations Comments Xopenex® Xopenex HFA® Pregnancy Category C Levalbuterol Nebulizing Solution Oral Aerosol Store at room temperature. Protect from light. Contains 200 actuations. Vials should be used within two weeks after opening protective pouch. Proventil HFA ®, Proair HFA ®, AccuNeb® Ventolin HFA® Combivent® (combination product), VoSpire ER® Pregnancy Category C Albuterol Oral Aerosol Nebulizer Solution Tablet Extended Release Tablet Syrup Store at room temperature, each inhaler contains 200 actuations, Use nebulizing solution within one week of opening foil pouch. Maxair ® Pregnancy Category C Pirbuterol Oral Aerosol Autohaler Contains 400 inhalations, Store at room temperature Alupent® Pregnancy Category C Metaproterenol Oral Aerosol Nebulizer Syrup Tablet Store in a tight, light resistant container. Contains 200 actuations. Do not use if solution is brown or contains a precipitate. Long Acting Beta Agonists (LABA) Used for the PREVENTION of bronchospasms Brand Name Generic Name Dosage Forms Comments Foradil® Perforomist ® Symbicort ® (combination product) Pregnancy Category C Formoterol Aerosol Powder Nebulizing Solution Store Foradil® in refrigerator prior to dispensing, after dispensing store at room temperature. Remove capsules from blister pack immediately before using. Use within 4 months of purchase. Serevent Diskus® Advair HFA ® (combination product) Pregnancy Category C Salmeterol Aerosol Powder Store at room temperature away from direct light or heat. Stable for 6 weeks after removal from foil pouch. Not for the use of acute control of bronchospasms. Major substrate 3A4. Beta Agonists • Side Effects – – – – – – – – Tachycardia Insomnia Nervousness Hypokalemia Hyperglycemia Diarrhea Dry Mouth Tremors • Drug Interactions – – – – MAOIs Sympathomimetic Agents Beta Blockers P450 3A4 Inhibitors & Inducers • Salmeterol – Caffeine – Yohimbine Spacing Devices Corticosteroids Generic Name Brand Name Formulations Beclomethasone Pregnancy Category C QVAR ® Oral Aerosol 100 Actuations Traimcinolone Pregnancy Category C Azmacort ®, Oral Aerosol 240 actuations Flunisolide Pregnancy Category C Aerobid ® Aerospan HFA Oral Aerosol 100 actuations Fluticasone Pregnancy Category C Flovent HFA ® Flovent Diskus ® Advair ® Oral Aerosol 120 actuations Mometasone Pregnancy Category C Asmanex ® Aerosol Powder 200 Actuations Budesonide Pregnancy Category B Pulmicort Flexhaler ® Pulmicort Respules ® Symbicort ® Aerosol Powder 120 Actuations Nebulizer Corticosteroids • Oral Agents – Prednisone – Methylprednisilone – Prednisilone • Adverse Effects – Oral candidiasis – Hoarseness – May slow bone growth in children. – Cushing’s Effects – Osteoporosis – Hypertension – Cataracts – Glucose Intolerance – Skin Thinning – Depression • Comments – Use SPACERS to minimize local and systemic adverse effects. – RINSE MOUTH with water after inhalations to prevent thrush infections. – Use steroid inhalers as scheduled not as needed. – Consider calcium and Vitamin D supplementation. – Pulmicort Respules is the only nebulized approved steroid. Corticosteroids: Drug Interactions • Anti-diabetic agents • 3A4 Inhibitors & Inducers – Flunisolide, Fluticasone, Mometasone, Budesonide Mast Cell Stabilizer Brand Name Generic Name Formulations Intal Cromolyn Sodium Oral Aerosol 200 actuations Nebulizing Solution Mast Cell Stabilizers • Adverse Effects – Unpleasant taste – Cough • Drug Interactions – No significant drug interactions • Comments – Slow onset: may take 4-8 weeks for expected effect. – Alternative to steroids in children. – Not for rapid relief. Theophyilline ( Theodur, Uniphyl, Theo-24) • Dose 10 mg/kg/day given BID-TID with a maximum dose of 900 mg daily. • Therapeutic Levels – 5-15 mcg/mL • Formulations – Controlled Release Tablet (Uniphyl) – Extended Release Capsule (Theo-24) – Elixir (Elixophyllin) • Side Effects – – – – – – – – Nausea Vomiting Nervousness Tremors Insomnia Headache Arrhythmia Seizures Theophylline cont. • Drug Interactions – 3A4 and 1A2 Inhibitors & Inducers – Caffeine • Comments – Beneficial for night symptoms. – Not for acute relief. Leukotriene Modifiers Generic Name Brand Name Formulation Montelukast Singulair Tablets Chewable Tablets Granules Zafirlukast Accolate Tablets Leukotriene Modifiers • Drug Interactions – Montelukast • Inhibitors & Inducers of 2C9 & 3A4. – Zafirlukast • Inhibits 2C9, 3A4 • Inhibitors & Inducers of 2C9 (it is a major substrate). • Adverse effects – Hepatotoxicity • Liver function tests at baseline, every month x 3 months for one year – Headache – GI Upset Zileuton (Zyflo®) • Inhibits the production of leukotrienes. • Available as an extended release tablet • Useful in mild persistent asthma and in combination with corticosteroids in moderate persistent asthma. • Used in pateints > 12 years of age. • Adverse Effects – Elevated liver enzymes. – Monitor hepatic enzymes • Drug Interactions – Zileuton is a 1A2 and 3A4 inhibitor. Omalizumab ( Xolair) • Monoclonal antibody that acts by inhibiting IgE binding to mast cells and basophils. • Administered subcutaneously every 2-4 weeks • Must be refrigerated. • Helpful in moderate to severe persistent allergyrelated asthma. • Use in > 12 years old • Second line therapy • Very expensive Omalizumab (Xolair) • Drug Interactions – No significant drug interactions • Adverse Effects – – – – Injection site reaction Urticaria Thrombocytopenia Anaphylaxis Case • Based on her medication profile are there any medications that may be interfering with the efficacy of albuterol? Are there any drug interactions within her profile? Stepwise Approach to Asthma • Intermittent = Step 1 • Mild = Step 2 • Moderate = Step 3 or Step 4 • Severe = Step 5 or Step 6 Stepwise Approach of Management of Asthma Management of Exacerbations • Assess Severity • Initial treatment – Short acting beta agonist • Good Response • Incomplete Response • Poor Response Questions • • • • Angela Singh [email protected] 599-3359 Office # 345