* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 1e4cb96be631de9
Survey
Document related concepts
Transcript
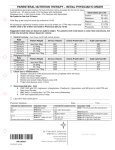
TPN Total Parenteral Nutrition Outlines • • • • • • • • Definition Indication. Types of parenteral Nutrition TPN Solution Content Equipment Administration Montoring. Nursing skills TPN • TPN therapy is the abbreviation for Total Parenteral Nutrition. • TPN therapy is the delivery of all essential nutrients required by the body through the blood stream. • (TPN) is a method of feeding that bypasses the gastrointestinal tract. Fluids are given into a vein to provide most of the necessary nutrients the body needs. The method is used when a person cannot or should not receive feedings or fluids by mouth. Indication • Trauma to the GIT. • Pre-operative malnutrition. BMI less than 15. • Post-opertaive complication delying Enteral feeding. • Malabsorption as in cancer pt., radiotherapy, chemotherapy. • hyper metabolic rate as in sever trauma, burn, sepsis…. • Nausea, vomitind syndrom relates to CNS. Types of parenteral Nutrition Type Uses TPN by C.V.P , internal or external Jagular Catheter ► Nutritionally complete. ► High hypertonic solution. TPN by Periphereral Catheter ► Nutritionally complete. for short time. 2 wks or less. ► Provide up to 2000 C/ day. ► Not used in nutritional depleted pt. ► Not used in volume restricted pt. ► Maintain adequate nutrition status. ► As effective as re-assume bowel function and oral feeding after few days. ► Provide large calories and nutrients need. ► When need 2 wks or more Nutrition ► used in nutritional depleted pt ► Improve tolerance of surgery. Lipid emulsion ► May interfere with immune mechanisms. ► In pt. with respiratory compromise, reduce co2 build up. ►In pt. with respiratory compromise, reduce co2 build up TPN Solution Content • TPN requires water (30 to 40 mL/kg/day), • energy (30 to 60 kcal/kg/day, depending on energy expenditure), • amino acids (1 to 2.0 g/kg/day, depending on the degree of catabolism), • Glucose ,usually D50W or D20W, (25- 35%) • Lipids (10-20%) • Essential fatty acids • Electrolytes • Minerals • Vitamins TPN Content Value Basic Adult Daily Requirements for Total Parenteral Nutrition Nutrient Amount Water (/kg body wt/day) 30–40 mL Energy* (/kg body wt/day) Medical patient 30 kcal Postoperative patient 30–45 kcal Hypercatabolic patient 45–60 kcal Amino acids (/kg body wt/day) Medical patient 1.0 g Postoperative patient 2.0 g Hypercatabolic patient 3.0 g Minerals Vitamins *Requirements for energy increase by 12% per 1° C of fever. Equipment • • • • • • • • • • • • Strict aseptic technique. Central venous cath. Triple / double lumen, Hickman or C.V. Sub Xylocaine numbing Betadine. 4x4’s guaze. Heparin lock solution. Syringes to flush. IV fluid & line and caps & Pumps. Stitch to secure. Transparent obsite. CXR for placement . Health care team A variety of members of the health care team may be involved in the decisions to order parenteral nutrition and in the care required to administer it. These include: • • • • physicians pharmacists dieticians nurses administration: • Because the central venous catheter needs to remain in place for a long time, strict sterile technique must be used during insertion and maintenance. • The TPN line should not be used for any other purpose. • External tubing should be changed q 24 h with the first bag of the day. • In-line filters have not been shown to decrease complications. • Dressings should be kept sterile and are usually changed q 48 h using strict sterile techniques. • The solution is started slowly at 50% of the calculated requirements, using 5% dextrose to make up the balance of fluid requirements. • The amount of regular insulin given (added directly to the TPN solution) depends on the plasma glucose level; • if the level is normal and the final solution contains 25% dextrose, the usual starting dose is 5 to 10 units of regular insulin/L of TPN fluid. Monitoring Suggested monitoring schedule Baseline Acute patient Stable patient Blood chemistry Yes 2 - 3 times/week Weekly Lytes, BUN, creatinine Yes Daily 1-2 times/week Triglycerides Yes Weekly Weekly CBC w/diff Yes Weekly Weekly PT, PTT Yes Weekly Weekly Glucose 3 times/day 3 times/day until <200 consistently 3 times/day until <200 consistently Weight Yes Daily 2-3 times/week • If possible, blood tests should not be done during glucose infusion. • Physical examination; Obesity and the Metabolic Syndrome: Body composition analysis. Complications • Mechanical: Pneumothorax, hemothorax, air embolism, catheter misplacement, thromboembolism. • Infection: Prevent by using aseptic tech. During insertion & post care. Use in line filter, Chg. Tubing q new bag. • Metabolic: Hyperglycemia –rarely hypoglycemia. • Others: Fluid Imbalances Electrolyte Imbalances Acid-base Imbalances (acidosis) Fluid over-load Pulmonary edema, CHF. DO • Refrigerate the TPN solution until 30 minutes before using it • Avoid infusing it immediately after refrigeration. • Check the bag against the order for the correct patient name, formula components, and expiration date. • Explain the procedure to the patient. • Use a filter to administer TPN solution. Initiate therapy at a rate of 40 to 50 ml/hour, then increase the rate by 25 ml/hour every 6 hours (as tolerated) until reaching the desired infusion rate. Infuse TPN at a constant rate. • Every 24 hours, change both the bag and the tubing. • Be sure to clamp the central line (to prevent air from entering the catheter and causing an embolism). • Check the venous access site for redness and drainage and monitor the patient for signs and symptoms of sepsis. Using aseptic technique, change the dressing every 48 hours or whenever it becomes soiled or loose. DO NOT • Don't store TPN solution at room temperature, which would promote bacterial growth. • Don't allow a bag of TPN solution to hang longer than 24 hours. • Don't add medication to a TPN bag, piggyback anything into a TPN line, or administer other medications through the same lumen as TPN solution. • Don't administer TPN solution that has a brown layer, which indicates that the lipids have separated from the solution. Nursing Care, Skills • Daily Weight. • Prevent infection, air embolism. • Maintain fluid & electrolyte balance. • Encourage ambulation, ADL’s & comfort. • Educate patient & family. • NPO stress. • Dressing change. • No meds backed into TPN • No blood drawn from TPN port • Always chart port being used • Always on Infusion Pump!!!! • TPN order checked against label, checked by 2 RN’s & signed • Gradually rate increased when beginning • When discontinuing- gradual decreasing Discontinuing Central Line • • • • • • • MD ORDER! Suture removal kit Sterile gloves Remove suture, pull out in one motion Hold pressure sterile gauze Sterile dressing – check for drainage PRN culture cath tip. After care Patients who have been receiving parenteral nutrition for more than a few days, and have been given permission to start eating again, should reintroduce foods gradually. This will give the digestive tract time to start functioning again. References • Wikipedia , last modified on 15 January 2010 . • McConnell, Edwina A "Administering total parenteral nutrition". Nursing. FindArticles.com. 31 Mar, 2010. • Copyright Springhouse Corporation Nov 2001 Provided by ProQuest Information and Learning Company. • http://findarticles.com/p/articles/mi_qa3689/is_20 0111/ai_n8997797. • Bare, B. & Smeltzer, S. (2004\0: Medical Surgical Nursing. Loppincott. • Alexander, M., et al . (2007). 3rd Ed. Nursing Practice. The Adult. Churchill Livingstone. • Hardine, S., Kaplow, R. (2008). Critical Nursing Optimal Outcomes. Jones Bartelett Publisher.
























![Adult Peripheral Parenteral Nutrition [31152] 31152 Adult Peripheral](http://s1.studyres.com/store/data/008026131_1-d48ced12e0c1aec6da28b090ad0e5917-150x150.png)