* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download NSAIDs: Friend or Foe
Drug interaction wikipedia , lookup
Prescription costs wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Environmental persistent pharmaceutical pollutant wikipedia , lookup
Toxicodynamics wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Non-specific effect of vaccines wikipedia , lookup
Psychopharmacology wikipedia , lookup
Theralizumab wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
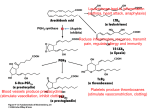
NSAIDs: Friend or Foe Hot Topic Presentation Lars Halford, GP ST3 March 2010 Non-Steroidal AntiInflammatory Drugs Acetylsalicylic acid first produced by Charles Frederic Gerhardt in 1853 Not until1897 that Bayer, a drug and dye firm, began investigating its use as a less irritating version of standard salicylate medicines. By 1899, Bayer was distributing their Aspirin around the world Ibuprofen launched in 1969 COX-2 enzyme discovered in 1988 Celecoxib launched in 1999 How do they work? Cyclo-oxygenase (COX) enzyme used by cells in the synthesis of prostaglandins Exists in 2 forms – COX-1 and COX-2 Analgesic and anti-inflammatory effect mainly dependent on COX-2 Unwanted GI side effects due to inhibition of COX-1 GI Effects Traditional NSAIDs (tNSAIDs) associated with 4-fold increase in incidence of severe upper GI ulcer complications (e.g. bleeding or perforation) No clear consistent evidence that any nonaspirin tNSAID is any better than another COX-2 selective NSAIDs (coxibs) result in significant decrease in upper GI complications Renal Effects NSAIDs inhibit prostaglandininduced vasodilation Potentially causes reduced renal blood flow and can precipitate renal failure Likelihood highest if existing renal impairment, CCF, liver cirrhosis and those on ACE inhibitors, ARBs or diuretics No difference between tNSAIDs or coxibs What about CV effects? Natural balance between: Pro-thrombotic Thromboxane A (synthesised by platelets using COX-1) Anti-thrombotic Prostacyclin (synthesised in vascular endothelium by COX-2) Prostanoid hypothesis Aspirin is an irreversible non-selective inhibitor of COX-1 and COX-2. Platelets have no nucleus so blockade from aspirin lasts for their entire lifespan Prostacyclin can be synthesised de novo by endothelial cells so aspirin tips balance to anti-thrombotic side Hence aspirins use in secondary prevention of CV disease Does this explain NSAID CV risk? Other NSAIDs not irreversible blockers so may tip things into prothrombotic balance (especially coxibs) – or so the theory goes Thought to be oversimplistic, however… No alternative full and credible mechanism for CV s/e of NSAID’s yet been demonstrated Vioxx (Rofecoxib) Large RCT by Bombardier et al (2000) found higher rate of MI in patients taking Vioxx compared to naproxen Subsequent studies found Vioxx to be associated with significant increase in thrombotic events Worldwide withdrawal of Vioxx in 2004 Sparked numerous further trials looking into CV safety of coxibs and tNSAIDs (e.g. ADAPT, CLASS, MEDAL, TARGET) Meta-analysis Drug RR of CV events (95%CI) Rofecoxib <25mg/d 1.33 (1.00-1.79) Rofecoxib >25mg/d 2.19 (1.64-2.91) Celecoxib (all doses) 1.06 (0.91-1.23) Meloxicam 1.25 (1.00-1.55) Diclofenac 1.40 (1.16-1.70) Naproxen 0.97 (0.87-1.07) Ibuprofen 1.07 (0.97-1.18) McGettigan P, Henry D. JAMA 2006;296(13);1633-44 So what does this mean for us? BOTH tNSAIDs and coxibs are associated to varying degrees with increased CV risk We must consider co-morbidities and concurrent medications that may sway risk Older patients are at increased risk of CV, GI and renal side effects – weigh up risk/benefit Both tNSAIDs and coxibs are viable and effective options to treat pain and have manageable side effect profiles Practical Advice In terms of CV effects, naproxen is associated with lowest risk and diclofenac the highest All NSAIDs contraindicated in active peptic ulceration but coxib may be used in those with a history of ulceration Always consider prescribing gastric protection in form of PPI for those requiring long-term tNSAIDs OR coxibs NICE judged that it is cost-effective to add generic PPI to tNSAIDs or coxibs used as treatment for rheumatoid or osteoarthritis NICE advises against use of any NSAID in those taking low-dose aspirin Avoid tNSAIDs and coxibs in those with history of heart failure Avoid tNSAID or coxib in those with GFR <30, use with caution when GFR 30<60 Practical Advice – Bottom Line Prescribe lowest effective dose for the shortest period of time In chronic pain consider as required dosing and review regularly Advise patient regarding potential side effects and do what you can to minimise risks Monitor BP, renal function and liver function in those on long term The Future Await results of trials such as PRECISION (Prospective Randomised Evaluation of Celecoxib Integrated Safety versus Ibuprofen or Naproxen)