* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Survey
Document related concepts
Transcript
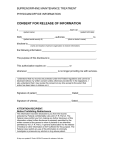
How to find your way around … You can play the PowerPoint and the Test here. START FINISH How to find your way around … Always click the ‘home’ icon to save your progress and log off. This is important! START FINISH Consent Training For clinical community healthcare staff. START FINISH Objectives This programme has been developed to inform all health care professionals and support staff, on the legal requirements for obtaining valid consent before starting treatment, physical investigation or providing personal care, for a patient, in line with Department of Health requirements. Responsibility A health care professional (including support staff) who does not respect the legal and ethical principle for obtaining valid consent may be liable both to legal action by the patient and action by their professional body. START FINISH Overview Patients have a fundamental legal and ethical right to determine what happens to their own bodies. Valid consent to treatment is therefore absolutely central in all forms of healthcare, from providing personal care to undertaking major surgery. Seeking consent is also a matter of common courtesy between health professionals and patients. Further guidance can be found on the Department of Health Website at :http://www.dh.gov.uk/en/Publicationsandstatistics/Publicati ons/PublicationsPolicyAndGuidance/DH_103643 START FINISH Obtaining consent Obtaining consent is a mutual decision making process which is thorough and in line with trust policies/procedures and legal consent processes. Agreement Context of Consent “Consent” is a patient’s agreement for a health professional to provide care. Patients may indicate consent non-verbally (for example by presenting their arm for their pulse to be taken), orally, or in writing. For the consent to be valid, the patient must: The context of consent can take many different forms; • Active request by a patient of a particular treatment (which may or may not be appropriate or available) • In some cases, the health professional will suggest a particular form of treatment or investigation and after discussion the patient may agree to accept it. • Passive acceptance of a health professional’s advice. • In others, there may be a number of ways of treating a condition, and the health professional will help the patient to decide between them. • • • Have capacity to take the particular decision; (refer to The Mental Capacity Act 2005) Have received sufficient information to take it; and Not be acting under duress. START FINISH Decisions Decisions must always demonstrate that the patient’s “best interest’s” are at the top of the decision making process!! Joint Decision Making Some patients, especially those with chronic conditions, become very well informed about their illness and may actively request particular treatments. In many cases, “seeking consent” is better described as “joint decision-making” the patient and health professional need to come to an agreement on the best way forward, based on the patient’s values and preferences and the health professional’s clinical knowledge. Guidance Where an adult patient lacks the mental capacity (either temporarily or permanently) to give or withhold consent for themselves, no-one else can give consent on their behalf, not even a relative, unless they have a valid lasting Power of Attorney or a Deputy Appointed by the Court of Protection Guidance with reference to the; Mental Capacity Act 2005 Deprivation of Liberty will need to be considered. All staff must follow guidance in Policy MCP1 and MCP2 and associated procedures, which are in line with the CQC’s regulatory framework and associated guidance and Risk Management Standards. START FINISH However! “Treatment may be given if it is in their “best interests” as long as it has not been refused in advance in a valid and applicable advance decision” An example of this would be:An individual may need antibiotics for a urinary tract infection which may greatly improve the quality of the patient’s life. For further details on advance decisions see the Department of Health’s Reference guide to consent for examination or treatment 2009 (chapter 1, paragraph 19). Trust Policy Guidelines CLPG6 which can be accessed from the Intranet library. START FINISH Case study Mary is a 75 year old lady who lives in a local care home and has a diagnosis of Lewy-Bodies Dementia. She is refusing to accept any pharmacological interventions for the condition. Mary has always felt strongly about this and she has a valid and applicable advanced decision that she has made in writing, when she had capacity stating “that she never wanted to be treated with any medication for dementia, specifically anti-psychotic medication or anxiolytics”. Her mother also had been diagnosed with dementia and had experienced “severe reactions” to these types of medications in the past. Mary had cared for her mother during the later stages of her condition and found these reactions extremely distressing to witness; hence her strong wish “never” to be treated with the same medications specifically in the later stages of her own condition. Mary is assessed as lacking capacity to make a decision in relation to accepting and refusing medication for the treatment of her distressing symptoms. It is felt that it would be in her “best interest’s” to give her these medications, as they may alleviate or minimise the delusions and hallucinations she is continually experiencing. START FINISH When do Health Professionals need consent? Who is the right person? Before examining, treating or caring for a child, you must seek consent. Young people aged 16 and 17 are presumed to have competence to give consent for themselves. Younger children who understand fully what is involved in the proposed procedure can also give consent (although parents will ideally be involved) For Example: - Blood transfusion or chemotherapy. In other cases where a child is not deemed competent, someone with parental responsibility must give consent on the child’s behalf, unless they cannot be reached in an emergency. For example: - A child falls in the playground and fractures their arm as their circulation may be compromised they need urgent medical treatment in this case a schoolteacher may be needed to intervene. If a competent child consents to treatment, a parent cannot over-ride that consent an example of this is an adolescent requesting contraception. It should be noted however that there are very rare exceptions to this, and further advice and guidance on this is available within the Consent Policy. START FINISH Covering the Bases Is Consent Voluntary? “If a patient is not offered as much information as they reasonably need to make their decision, and in a form they can understand, their consent may not be valid” Consent must be given voluntarily; not under any form of • Duress • Undue influence from health professionals, family or friends. Refusals of treatment Competent adult patients are entitled to refuse treatment, even where it would clearly benefit their health. Although the above statement is in the main true it should be noted that there are exceptions to this rule; • Where the treatment is for a mental disorder and the person is detained under the Mental Health Act 1983 • A competent pregnant woman may refuse treatment, even if this would be detrimental to the foetus. START FINISH Advanced Refusal If an incompetent patient has clearly indicated in the past, while competent, that they would refuse treatment in certain circumstances (an advanced refusal Advanced Decisions CLPG 6), and those circumstances arise, you must abide by that refusal. All answers are based on information within appendix A of CLP 16 For further details, consult the Reference guide to consent for examination or treatment, available from the NHS Response Line 0541 555 455 and at www.doh.gov.uk/consen Further Advice Specific guidance, incorporating both the law and good practice advice, is available for health professionals working with children, with people with learning disabilities and with older people. Copies are available on the Trusts Intranet site (see clinical governance/clinical effectiveness) and may also be accessed on the Internet at www.dh.gov.uk/consent. START FINISH Question Competent adult patients are entitled to refuse treatment, even where it would clearly benefit their health. FALSE TRUE Continue START FINISH Documentation For significant procedures, it is essential for health professionals to document clearly both a patient’s agreement to the intervention and the discussions which led up to that agreement. This may be done either through the use of a consent form (with further detail in the patient’s notes if necessary), or through documenting in the patient’s notes that they have given oral consent. Considerations Consent maybe incorrectly equated with a patient’s signature on a consent form. A signature on a form is evidence that the patient has given consent, but is not proof of valid consent. If a patient is rushed into signing a form, on the basis of too little information, the consent may not be valid, despite the signature. Similarly, if a patient has given valid verbal consent, the fact that they are physically unable to sign the form is no bar to treatment. Patients may, if they wish, withdraw consent after they have signed a form: the signature is evidence of the process of consent-giving, not a binding contract. START FINISH Written Consent It is rarely a legal requirement to seek written consent, (The Mental Health Act 1983 and the Human Fertilisation and Embryology Act 1990 require written consent in certain circumstances) but it is good practice to do so if any of the following circumstances apply; The treatment or procedure is complex, or involves significant risks (the term risk. is used to refer to any adverse outcome, including those which some health professionals would describe as side-effects. or complications.) The procedure involves general/regional anaesthesia or sedation providing clinical care is not the primary purpose of the procedure There may be significant consequences for the patient’s employment, social or personal life The treatment is part of a project or programme of research approved by this Trust. Consent will always be sought if examination or treatment of an intimate nature is required i.e., Smear Test or Enema or Suppositories START FINISH Trust forms Completed forms must be kept with the patient’s notes. Any changes to a form, made after the form has been signed by the patient, should be initialled and dated by both patient and health professional. Forms can be located in the appendices of CLP16. It will not usually be necessary to document patients consent to routine and low-risk procedures, such as providing personal care or taking a blood sample. HOWEVER ASK YOURSELF....... If any of these are the case then it would be helpful to do so! START FINISH Procedures Procedures to follow when Patients lack capacity to give or withhold consent Where an adult patient does not have the capacity to give or withhold consent to a significant intervention, This fact should be documented in form 4 (for adults who are unable to consent to investigation or treatment CLPG16) Along with the assessment of the patient’s capacity, why the health professional believes the treatment to be in the patient’s best interests, Involvement of people close to the patient. The standard consent forms should never be used for adult patients unable to consent for themselves. For more minor interventions, this information should be entered in the patient’s notes. START FINISH Question Where must completed forms be kept? In an office In a safe With the patients notes Placed in the ‘in’ tray Continue START FINISH Lack of capacity An apparent lack of capacity to give or withhold consent may in fact be the result of communication difficulties rather than genuine incapacity. You should involve appropriate colleagues in making such assessments of incapacity, such as specialist learning disability teams and speech and language therapists, unless the urgency of the patient’s situation prevents this. If at all possible, the patient should be assisted to make and communicate their own decision, for example by providing information in non-verbal ways where appropriate. Information disclosed will vary from each patient, relatives and carer’s, some require comprehensive information, including rare risks, to some who ask health professional to make decisions on their behalf. Sound clinical judgment is required in determining the information given. However, the presumption must be that all patients will be treated with the upmost respect and all information will be imparted allowing the patient to make an informed decision. START FINISH The following sources of patient information are available in this Trust: Ward and service leaflets Touch screen information kiosks,(the touch screen Information Kiosks in Essex provide web links to many on-line sources of information) In addition, the PALS Service (Patient Advice and Liaison Service) and NHS Direct can assist patients to access more detailed information. Written fact sheets on common mental health conditions and drugs For example; All written information can be translated on request, or made available in large print, braille or recorded onto tape or CD. Departmental managers or the PALS will advise of all local advocacy services. A provision for patients where English is not their first language; This Trust is committed to ensuring that patients whose first language is not English receive the information they need and are able to communicate appropriately with healthcare staff. It is not appropriate to use children to interpret for family members who do not speak English. START FINISH Useful Contacts For interpreting and translation services please contact:Essex Interpreting Service on 01375 842244 Bedfordshire and Luton: Milton Keynes community Language Service on 01908 253253 or www.milton-keynes.gov.uk /community language service The information contained in the consent policy can also be produced in other formats on request. Please contact the Communication Department at Pride House Further Considerations The Human Rights Act 1998 Article 2 Protection of right to life Article 3 Prohibition of torture and inhumane or degrading punishment Article 5 Right to liberty and security Article 9 Freedom of thought, conscience and religion START FINISH Responsibility of Health Professionals It is a health professional’s own responsibility to: To adhere to Trust policies and Procedures at all times. Adhere to professional codes of conduct To ensure that when they require colleagues to seek consent on their behalf they are confident that the colleague is competent To work within their own competence and not to agree to perform tasks which exceed that competence. If you feel pressurised to seek consent, when you do not feel competent do so. You must contact your line manager immediately for advice. Ensure where possible that professionals adhere to Multidisciplinary Team working. Keep clear, concise and up to date records START FINISH Remember, if you want to find more information / evidence about this subject or anything else which is relevant to your work or study, join your local healthcare library. For staff in Essex contact Basildon Healthcare Library. www.btuheks.nhs.uk [email protected] 01268 524900 EX3594 It may be that you work in a different area, for example Luton. Details of all the Health Libraries in the East of England can be found at this site… www.eel.nhs.uk You are welcome to join any of these. START FINISH Review of Objective(s) Before completing the test, please ensure you have acquired the relevant knowledge against the modules objective(s) below: “To inform all health care professionals and support staff, on the legal requirements for obtaining valid consent before starting treatment, physical investigation or providing personal care, for a patient, in line with Department of Health requirements.” If not, please take this opportunity to revisit the presentation content. CONTINUE START FINISH You now need to take the test! Remember to click the ‘home’ icon when you have finished the test to save your results! START FINISH