* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Introduction to HNI/HNC 370
Survey
Document related concepts
Transcript
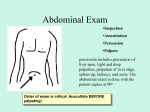
Introduction to HNI/HNC 370 Definition of Health Influencing Factors Philosophy Practice Health Care System Practices Behaviors Influenced by cost/insurance Definition of Health Health is a dynamic state in which the individual adapts to changes in the internal and external environment to maintain a state of well being. Health is a state of complete physical, mental, spiritual, and social well-being. Internal Environment Genetic and psychiatric variables Intellectual and spiritual dimensions Physiological and physical disease processes External Environment Physical environment Social relationships Economic variables Internal and external environment may continually change; individual must adapt to maintain a state of well being. Theoretical Models R/T Health Developmental theories provide a framework for the practitioners psycho-social and cultural profile. Maslow’s Hierarchy of Needs: Cognitive Development by Piaget: People are innately motivated towards psychological growth, selfawareness & personal freedom. A person understands whatever fits into his established view of the world, when the info does not fit, he must re-examine & adjust his thinking to accommodate the new info. A person should reach this level by adolescence. Culture Transcultural Nursing Madeline Leininger “Theory of Transcultural Nursing” Defined: “Focuses upon the differences and similarities among cultures with respect to human healthcare, health (well-being) and illness. Bases upon the people’s cultural values, beliefs, practices, and use of this knowledge to provide culturally specific or culturally congruent nursing care.” Cultural Assessment Ethnic Origin Race Habits/customs/beliefs Behaviors valued by culture Cultural sanctions and restrictions Healing beliefs Child rearing/child care Spiritual Factors Educational Factors Occupational Factors Economic Factors Assessment of the Family Assessment of the Home Assessment of the Community Levels of Prevention I. Primary Prevention True Prevention Precedes disease/dysfunction Applied to Healthy Population It is NOT therapeutic Does not involve symptom ID Secondary Prevention Provides screening and treats early stages of disease. Limits disability Tertiary Prevention Occurs when a deficit or disability is permanent or irreversible. Focus on rehabilitation- assist person to attain highest level of functioning. Nursing Process Assessment-Data Collection Data Validation Organize Data Diagnosis Planning Implementation Evaluation Assessment Focus: Data collection Data collection is a systemic method of gathering information about the client. Method: Four Components History taking- Primary Source-Patient Secondary SourceMedical Records Family Health Professionals Physical Examination Lab. Results Other sources, x-ray, MRI, CT Scan, EKG Types of Data Subjective Data: Information described by the patient to the nurse. Objective Data: Information collected by using the senses, IPPA. Inspection, percussion, palpation, auscultation Data Validation Is the patient data normal or abnormal? Is the information collected accurate? Data Organization Cluster similar data to assist in the identification of a health pattern. Elements of The Health History Biographical Data Chief Complaint History of Present Illness Past Medical History Past Surgical History Family History Review of Systems Psychosocial History Biographical Data Name Age (DOB) Race Sex Birthplace Source of HX. Occupation Chief Complaint Why is the patient seeking health care? Should be in patient’s own words and include a time frame when possible. Ex. “I have a pain in my back for 3 days.” Ex. “I haven been admitted for evaluation of my heart.” History of Present Illness A clear chronological narrative beginning with the earliest onset of the CC and describing its progression to the present. Starts with: This is a Report of symptoms should include: SLIDTA Foramat SLIDTA Format S L I D T A Severity Location Influencing Factors Duration Type Associated Symptoms Example CC: “I have a belly ache for two months” HPI: This is a thirty-one year old white female that presents today complaining of stomach pain occurring on and off for two months. The pain is described as burning, with a pain level of 8/10 that often prevents her from falling asleep. The pain is deep, approx. 4 finger breaths above the umbilicus. Pain occurs after eating, occasionally on an empty stomach and is relieved with Tums, 2 tablets. The pain increases when lying down, and relieved in an upright position. Spicy foods, nuts, fruits and vegetables increase pain. Denies associated symptoms of nausea and vomiting. Presented today because past remedies no longer working. Past Medical History (PMH) Communicable diseases Immunizations Major Illnesses-include date & place in chronological order ’82 NIDDM ’88 Lyme Disease Past Surgical History (PSH) Same as medical history, but describes surgical procedures ’89 L AKA ’92 R Carotid Endarterectomy Medications Prescription, OTC, Dose, Route and Frequency Include Allergies, animals, blood, contact agents (LATEX), food, drugs. If none state no……….. If allergy present, describe reaction. Social History Habits- Smoking (Pack Years), Alcohol (How Much), IVDA. Living arrangements: marital status, employment status. Genogram ADL Nutrition-24 hour intake, approx. amounts and time. Exercise, recreation, rest, sleep Ask “what is a typical day for you?” Psychosocial History Interpersonal functioning: Relationships with family, friends, spouse. Intapersonal Functioning:Stress and coping mechanisms. Values and Beliefs. Review of Systems Reviews all current and pertinent past symptoms to be sure that no important clues have been overlooked, either by the patient or practitioner. If you obtain a Positive response, elicit further information. THE PATIENT’S RESPONSES ARE RECORDED, NOT PHYSICAL FINDINGS. IPPA There are four classic techniques of the physical examination: I Inspection P Palpation P Percussion A Auscultation Inspection The process of observation. Adequate lighting and proper exposure essential. Preliminary Observations: Gait, ROM, Eye Contact, Skin Color, Body Language. Inspection continues throughout the examination. Palpation Use of the hands/fingers to gather information through the sense of touch. The hand is an important diagnostic tool to distinguish between:hard and soft, rough and smooth, stillness from vibration. Dorsal surface of the hand is used to estimate temperature. Palpation can be light (up to 1 cm) or deep (up to 4 cm). Light palpation should precede deep. Ballottment Percussion Striking a portion of the body to evaluate the condition of underlying structures. Degree of tone is determined by the density of the medium through which sound waves travel. Sound vibrations are best transmitted through firm solids, less transmission through fluid, and poorest through air. ExampleConsolidation of advanced pneumonia. Percussion cont. Tympany-Abdomen Dullness-Liver Resonance-Lungs Percussion cont. Technique: Hold pleximeter finger flat on the surface to be percussed using the tip of the plexor finger, strike the dip joint of the pleximeter finger. The strike should be brisk and short Remove the plexor immediately after contact with the pleximeter. The strike should bounce off the pleximeter fingers, not poke. Use your sense of touch and hearing as you percuss. Auscultation Try for a quiet environment. Learn to isolate sounds. Diaphragm transmits higher pitched sounds, press firmly on the surface. Bell is useful for lower pitched sounds and to listen to a limited surface area. Press lightly on the skin, if pressed tightly bell becomes a diaphragm.