* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Speech and Language Team and Nursing Staff
Survey
Document related concepts
Transcript
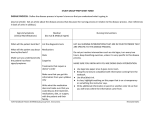
Speech and Language Therapist and Nursing Staff Joint Initiative - Oral Hygiene Our story so far Oral Hygiene Joint Initiative • Main hypothesis is to show how an oral care assessment tool, alongside an educational package can improve oral care of patients Why is Oral Hygiene Important? • Patient comfort • Psychological wellbeing • Prevention of migration of oral / dental bacteria which can lead to aspiration pneumonia Why Nursing Staff ? • Oral Hygiene is an important element of nursing care. • We wish to improve the care we give our patients. Why Nursing Staff? • Nursing Staff should be aware of how uncomfortable it can be for our patients who experience dry and sore mouths due to their illness and the use of certain medications. Why Speech Therapists? • SLTs are frequently involved in oral care as part of treatment of speech and swallow disorders • Spend lots of time observing and manipulating structures within the oral cavity • Both speech and swallow are hindered by dry, cracked, coated, uncomfortable lips and tongue Oral Hygiene Assessment • There is much variability in methods and therefore effectiveness of oral assessment and oral care given • Variations in: frequency process equipment products Oral Hygiene Assessment • Consensus in the literature that an evidence based, standardised assessment should be the basis on which a care plan is devised, tailored to each individual and prevent secondary clinical complications Oral Hygiene Assessment • Oral care is often not specific to the individual or clinical presentation and so may not improve oral health Oral Hygiene Assessment • There is no universally agreed tool to assess oral hygiene • Standardised assessment should be carried out at regular intervals to monitor and adapt the care plan as clinical improvement or deterioration occurs Our Oral Assessment • Based on the Revised Oral Assessment Guide (ROAG) by Andersson et al (2002) which is modified from Eilers at al (1988) • ROAG demonstrated inter-rater reliability, was clinically effective and represented a standardised approach to oral assessment Our Oral Assessment • The ROAG comprises 8 parameters and for each parameter a method of assessment is outlined. • The instructions were elaborated upon for some parameters to make them easier to assess and score Our Oral Assessment • Parameters: voice lips mucous membranes tongue gums teeth / dentures saliva swallow • Each scored out of 3: 1 – normal 2 – moderate problems 3 – severe problems Our Oral Assessment • Further risk factors for poor oral hygiene from the literature have been included: steroid treatment diabetes oxygen therapy mouth breathing radio / chemotherapy modified fluids NBM smoking • Who is administering oral hygiene has also been added. Our Oral Assessment • The completed assessment is scored out of 40 • Score indicates a treatment plan, including frequency of oral care needed, fluids and products to use Research Design • The research design used is based on the stages of the action research process identified by McGarvey 1993 Action Research A reflective stage follows where changes and modifications to the solution can be made The plan is put into action and its workings observed and monitored The problem to be studied is identified Problem concepts are investigated and related literature is studied The plan of action to solve the problem is designed Methodology • To create an oral assessment tool which is supported by an educational package • To audit the effectiveness of the tool by piloting it first on the Macmillan unit, then to invite other units such as MFE and Critical Care areas to pilot the tool, (educational sessions). Methodology • To design a treatment plan and a decision tool to guide the use of oral care products. • To disseminate to the Hospital Trust by changing the nursing policy and planning targeted educational sessions. Methodology • To design an educational approach throughout – Face to Face teaching followed by Pictorial/DVD guide “How to Guide”, easy reference and e – learning package which is accessible to all areas, (this will be audited after 12 mths following the roll out of first teaching sessions.) Time Scale • February 2009 – Teaching sessions to show the Nursing staff how to assess a patient’s mouth, the importance of oral care/health and how to use the tool and oral care products. • March 2009 – Roll out of the oral care assessment tool pilot Time Scale • June 2009 - revise the oral care tool following an audit of the tool and asking the nursing team to make comment and changes of the tool. • March 2009 – November 2009 to design a full educational package to support the tool. Time Scale • September 2009 – January to liaise with the Policy and Standards Group to introduce the proposal to change the nursing policy. • September 2009 – January 2010 to target/invite other units such as MFE and Critical Care to begin to pilot the tool in their areas Time Scale • January – March 2010 to roll out educational sessions and support to areas. • March 2010 to begin the pilot of the Oral Assessment Tool. References •McGavery, H. 1993. Participation in the research process: action research in nursing. Professional Nurse. March p 372-376 •Andersson P, Hallberg IR, Renvert S: Inter-rater Reliability of an Oral Assessment Guide for Elderly Patients Residing in a Rehabilitation Ward. Spec Care Dentist 22: 5, 181-186, 2002 •Rolfe G (1994) Towards a new model of nursing research. Jnr of Advanced Nursing 19, 969-975 •Rolfe, G. 1996 Going To Extremes: Action Research Grounded Practice and The Theory-Practice Gap In Nursing. Journal Of Advanced Nursing 24,13141320.