* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
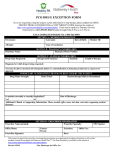
Consult Formulary Before Making an ePrescribing Decision August 25, 2005 HIMSS ePrescribing Webinar Series Co-presenters: Sandra White, Vice President MediMedia Information Technologies Michael Burger, Sr. Product Analyst Emdeon Corporation (formerly WebMD) Presentation Outline • Formulary overview – Different Types – How Constructed • ePrescribing Overview • How Formulary Fits within ePrescribing • Content Supplier-Software Company Interaction • Demonstration of Physician View • Formulary & Medicare Part D 2 What is a Formulary? • A continually updated list of medications that are covered under a plan or benefit: – – – – Managed Care Organizations (MCOs) Pharmacy Benefit Managers (PBMs) Hospitals Group Practices • Represents the current clinical judgment of physicians, pharmacists and other experts in the diagnosis and treatment of disease • Purpose is to maintain quality patient care while meeting cost-containment objectives 3 Construction Process • Content springs from recommendations of a pharmacy and therapeutics committee (P&T Committee), an independent panel of: – – – – Primary care physicians Specialists Pharmacists Other health care professionals 4 P&T Committee … • Objectively appraises, evaluates and selects drugs • Meets as frequently as necessary to review & update formulary • Establishes policies and procedures that educate and inform providers • Oversees quality improvement programs • Implements generic substitution and therapeutic interchange programs • Develops protocols and procedures for the use of and access to non-formulary drugs Source: Academy of Managed Care Pharmacy, Alliance of Community Health Plans, American Medical Association, American Society of Health-System Pharmacists, Department of Veterans Affairs, National Business Coalition on Health, U.S. Pharmacopeia 5 Myth: Formularies Are About Cost-cutting Only • P&T Committees first look at medications that are clinically effective. – Assess peer-reviewed literature – Compare the efficacy, type and frequency of side effects, and potential drug interactions – Evaluate benefits, risks and potential outcomes • When two or more drugs produce the same clinical results, the the P&T Committee considers: – Cost – Supplier Services – Ease of Delivery 6 Types of Formulary • There are three formulary categories in today’s marketplace: – Open (or voluntary) – includes all drugs, with a preferred ranking – Closed (or restricted) – only covers certain drugs; patient generally pays for non-covered. – Limited – limiting prescribing choices within certain therapeutic classes and offering unlimited choices in the remaining drug classes 7 Popular Formulary •A popular managed program is a “tiered” formulary. A common construct: Tier 4 Tier 3 Tier 2 Tier 1 • $5-$10 for 1 month supply • Generic drugs • $15-$20 for 1 month supply • Brand name drugs with no generic equivalent • $25-$30 for 1 month supply • Brand name drugs that have generic or therapeutic equivalents • Co-payment is 25-50% of drug cost • Formerly noncovered drugs (e.g. gene therapy) and lifestyle drugs Source: AIS, A Guide to Drug Cost Management Strategies 8 ePrescribing Overview 9 What is ePrescribing? EHR Connected Medication Mgmt Prescription Writer w/Data Stand-alone Prescription Writer Electronic Reference . Source: eHealth Initiative 10 Where are we today? 5-18% MDs prescribing electronically (eHealth Initiative, 2004) 85% pharmacies enabled for ePrescribing (SureScripts, ProxyMed, Emdeon, eRx Networks) 5% US hospitals using CPOE for Rx orders (KLAS, 2005) 14-39% Outpatient EMR use (California Healthcare Foundation, David Brailer, MD, 2004) $29 billion potential annual ePrescribing savings (Center for Information Technology Leadership, 2004) 11 Benefits: Prescribers Reduce Cost Increased quality of care by enabling easy access to computerized medication history Decreases potential medication errors due to illegible prescriptions Reduced waiting time at pharmacy Aura of high tech Improve quality of care Improve patient satisfaction Reduce phone calls Reduce chart pulls More time for patient care Low impact to existing workflow 12 Benefits: Payers/PBMs Decreases potential medication errors due to illegible prescriptions Reduced phone calls Better utilization of cost-effective alternatives Improve quality of care Reduce cost Improve customer satisfaction Employers: lower premium growth due to reduced drug spend Prescribers: Fewer hassles over coverage and prior authorization Consumer: Reduced wait time at pharmacy 13 Benefits: Pharmacies Reduce Cost Improve quality of care Improve customer satisfaction & care Reduce telephone calls Automate manual processes Reduce multiple eligibility inquiries Decreases potential medication errors due to illegible prescriptions Provides more time for patient counseling Patient: Reduce wait time Prescriber: Fewer interactions over coverage and prior authorization 14 Current, Paper Rx Process • Physician often prescribes medication unaware of drug’s formulary status or coverage information • Pharmacist alerted to formulary status upon submitting claim to payer • Pharmacist must call physician and request alternative; physician still unaware of status or coverage 15 The Electronic Prescription • Prescriber makes fully informed decision as he or she is presented with status and coverage information before selecting a medication • Prescriber can counsel patient before receiving medication • Pharmacist receives prescription with prescribers’ decision fully documented; claim adjudicated without alert 16 Formulary & ePrescribing 17 Point-of-Care Formulary • There are four sources of formulary information at the point of care: 1. 2. 3. 4. Formulary booklets Web sites Reference Sources ePrescribing 18 Electronic Prescribing and Formulary Databases EMR Connected Formulary Database Medication Mgmt Prescription Writer w/Data Stand-alone Prescription Writer Electronic Reference . Source: eHealth Initiative To Bring value, formulary information should cover 70% of a prescriber’s patients 19 Key Decision-support Tool Electronic formulary databases provide: • Status of medications – On/off/preferred – Prior authorization – Tier • Preferred alternatives • Coverage information – – – – Co-payments Relative cost Restrictions (age, quantity, etc) Step therapy 20 Get It Right The First Time! • Formulary within the context of ePrescribing reduces telephone calls back to the prescriber: Formulary Management Calls Rx Clarification Calls DUR Calls RDUR Prior Authorization Calls Renewal Requests Formulary Compliance Mailings 21 • In a 2003 study, Medco found a 42% reduction in pharmacy calls to practices. • In July 2002, Aetna found a 53% reduction in calls from, and 62% reduction in calls to, the retail pharmacy. • In 2002, Tufts saw a 35% reduction in calls between participating physician and pharmacists and found that physicians saved 2 hours per day. Formulary Aggregators Aggregator Type of Data Data for Comments MediMedia status, alternatives, relative cost, restrictions, Health plans, PBMs Employer Groups, Medicare, Medicaid Mapped to 3700 plan, PBM & employer names; normalized file structure. RxHub status, alternatives PBMs Only CareMark, Express Scripts and Medco; requires real-time interface CAQH status, alternatives Health plans Distributes data through RxHub; only the top 25 health plans Health plans, PBMs Employer Groups Availibility on a plan-by-plan basis Off-line reference ePocrates status 22 Formulary Databases Operate Behind the Scenes Plan, PBM or Employer A Extracts data, transmits to aggregator via flat file, Excel, MS Word, fax, eMail, CD-Rom Formulary Database B C Extracts plan & PBM demographic identifiers from POMIS Transmits data to software partner weekly, monthly via CD-Rom or FTP 23 D E Aggregator normalizes files for comprehension, ease of use Aggregator maps data to formulary files Formulary Databases Seamlessly Fit into the Office Workflow A Practice collects health or PBM card from patient, inputs into POMIS or EMR POMIS B Data shared with EMR, ePrescribing system in real-time, batch or one-time. Formulary Database Demographic Database C Practice “Source of Truth” Formulary linked to health or PBM identifiers 24 Demonstration 25 Formulary & Medicare Part D 26 Medicare Act of 2003 • Directs HHS to conduct a voluntary electronic prescription pilot project in 2006, unless there is already adequate experience. • Establishes a real-time ePrescribing program to be used by prescribers, pharmacies and pharmacists who serve Medicare patients – No mandate, but if used, standards must be followed – Standards via National Committee on Vital and Health Stats • Information provided electronically includes: – Benefits, formularies and tiering and coverage limitations – Information on drug being prescribed, patient’s history, DUR – Information on therapeutic alternatives 27 Medicare Part D (cont.) • Other components: – Discretionary grants to be made available to prescribers – Plans, hospitals, groups may purchase hardware for MDs – Plans may pay additional fees for reduced medication errors, improved formulary compliance & fewer adverse drug events Deadline for Secretary to develop ePrescribing Standards Sept 1, 2005 Launch 1-yr voluntary ePrescribing pilot program; plans can offer P4P Jan 1, 2006 Evaluation results of pilot program due to Congress Apr 1, 2007 28 Deadline for Secretary to finalize and release standards Apr 1, 2008 All Medicare providers using ePrescribing must adopt finalized standards April 2009 Proposed ePrescribing Rules • Final rules due in September • Names 3 foundation standards (asserting they have adequate industry experience): – NCPDP SCRIPT (sans Fill Status) – X12N 270/271 Eligibility (between Provider & PDP) – NCPDP Telecom (between pharmacy & PDP) • Plans two formats as foundation standards – Drug History – Formulary & Benefits 29 Components of Formulary & Benefit Standard • • • • Product Name (Health Plan) Formulary Status List Preferred Alternatives Coverage List – – – – – – – Product Exclusions Prior Authorization Medical Necessity Step Therapy Age, Quantity, Gender Limits Resource Link Text Messages • Copay Lists 30 What’s next? 31 Trends in electronic formulary • • • • Integrated data vs reference Increased inclusion of Medicare formularies More plans making formularies available Deeper data sets mirroring more complex pharmacy benefits • Automating related processes – E.g. prior authorization 32 Task Group Overview • Task Group Name: – Prior Authorization Workflow-to-Transactions • Date Task Group Formed: – November 18, 2004 • Task Group Participants: • Objectives: – Promote standardized automated adjudication of prior authorization – Coordinate the further development and alignment of standards – Identify additional needed standards 33 Proposed workflow PATIENT Visits Physician PRESCRIBER • Writes Prescription • Completes a structured Q&A • Submits PA Request • Transmits Prescription Drugs can be flagged as requiring PA, and simple rules applied via NCPDP Formulary & Benefit Standard PAYER • • • • Submit Required Patient Information via X12N-278 X12N-275 with HL7 Attachment Prescriptions are submitted via NCPDP SCRIPT 34 Determines PA Status Compiles PA clinical rules Processes PA Requests Processes Drug Claims Drug Claims are Submitted via NCPDP Telecommunication PHARMACY • Dispense Drugs • Files Drug Claims In Summary • A formulary is a continually updated list of drugs whose purpose is to maintain quality while containing costs • Electronic prescribing is gaining marketshare • Integrated within the electronic prescribing process, formulary provides a great deal of value as a decisionsupport tool that helps you “get it right the first time.” • Formularies are considered a critical component of the Medicare Part D benefit, as plans and coalitions are distributing their formularies through aggregators • Electronic formularies are becoming more comprehensive and providing more data • There is a trend to automate processes tangential to formulary such as prior authorization 35 Healthcare Information and Management Systems Society 230 East Ohio St., Suite 500 Chicago, IL 60657 312-664-4467 Please remember to complete the online evaluation. The link can be found with dial-in instructions Thank you! Copyright © HIMSS Not to be reproduced without permission 36