* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download January 2014 Balancing Incentive Program national call
Survey
Document related concepts
Transcript
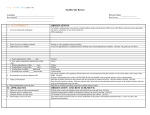
BALANCING INCENTIVE PROGRAM NATIONAL CALL January 15th, 2014 CMS in collaboration with Mission Analytics Group and New Editions Consulting Presentation Outline 1. 2. 3. 4. CMS Updates Mission Analytics Updates Disseminating Quality Data State Updates Medicaid Adult Core Set Core Set of 26 measures identified through multistakeholder process and publicly released in 2012 Voluntary reporting Began December 2013 CMS updates technical specifications manual annually Technical Assistance and Analytic Support Program for states Improvements to Core Sets are required (first update released Dec 2013) Core measure data feeds into information loop CMS collects, analyzes, and make publicly available the information reported by the states (Annual Secretary’s Reports, Reports to Congress) States use data to drive quality improvement Adult Medicaid Quality Grant Program 25 states participating in a two-year grant program that began December 2012 Three grant program goals: 1. Collect and report Adult Core Set measures in varying delivery care settings (e.g. managed care, fee-for-service, long term care settings such as nursing homes and intermediate care facilities) 2. Develop staff capacity to report, analyze, and use data for monitoring and improving access and the quality of care in Medicaid 3. Conduct at least two Medicaid quality improvement projects relating to Adult Core Set measures Adult Medicaid Quality Grant Program Grantees’ quality improvement topics relevant to BIP grantees: Care transitions from nursing facilities Initiation and treatment of substance use Integration of physical and behavioral health Follow-up care for mental health hospitalizations Chronic conditions (diabetes, adult asthma, cardiovascular health) States must report to CMS the methodology for collecting… Service data: Reports all community long-term services and supports individuals receive at the individual level Quality data: Captures the extent to which providers are supplying comprehensive, quality care Outcomes data: Assesses beneficiary and family caregiver experience and satisfaction with providers Methods for Collecting Quality Data Clinical measures Medicaid Adult Health Care Quality Measures (6) Healthcare Effectiveness Data and Information Set (HEDIS) (6) Waiver performance measures (5) Other mechanisms Money Follows the Person (MFP) Quality of Life survey (4) State-specific surveys and reports (4) Assessment data (1) Analyzing and Disseminating Findings Identifies systemic and plan- or providerspecific issues Encourages quality improvements Engages stakeholders Method 1: Discussions with Case Managers and Providers Georgia: State data quality and measures group reviews Healthcare Effectiveness Data and Information Set (HEDIS) measures and identifies trends within each waiver program Data group meets monthly or quarterly with providers and case managers to: Discuss source of identified trends. Suggest best practices to remedy trends. Georgia Performance Improvement Plan Method 2: Provider-Specific Reports and Follow Up Maryland: Waiver reports with provider-specific data are mailed to providers Corrective and preventive action plans are required Method 2: Provider-Specific Reports and Follow Up New York: Plan-specific quality data are distributed to the respective managed care plans Plans will be soon be able to access crude quality indicator (HCQI) reports directly from the state’s Uniform Assessment System (UAS-NY)* The UAS-NY will include features that allow: Automatic production of the crude HCQI reports. The NYS Office of Quality and Patient Safety to review and “approve” the reports before they can be accessed by plans. * The crude reports are not risk adjusted nor do they represent all of the information on quality data that will be available to plans. Method 3: Online Report Makes plan- and provider-level performance public Encourages plans and providers to improve performance to attract clients Augments transparency and accessibility Method 4: Collaborate with the state EQRO Illinois: The Illinois Department of Healthcare & Family Services, State Medicaid Agency, contracts with the Health Services Advisory Group (HSAG) to serve as the External Quality Review Organization (EQRO) for the state’s Managed Care Organizations (MCOs). The EQRO performs external oversight, monitoring, and evaluation of the quality assurance component of managed care. The EQRO process includes review of MCO compliance with State standards for access to care, structure and operations, and quality measurement and improvement. Validation of Performance Measures & PIPs Monitoring of Corrective Action Plans Method 4: Collaborate with the state EQRO (continued) Illinois: HSAG findings are communicated to the MCO’s and stakeholders via: Monthly conference calls Written report following the EQRO’s on-site record review for the MCOs Quarterly face to face meetings EQR Technical Report: aggregated information on quality, timeliness, and access to health care services that the MCOs furnish to Medicaid recipients Development of a Performance Tracking Tool (PTT) to be used by each MCO to monitor and trend results for each performance measure Stakeholder meetings Program Resources Approved State applications and Work Plans Revised Implementation Manual, FAQs, State Summaries, State Profiles, and other resources Email CMS: [email protected] Email Mission Analytics: [email protected] Quality Data Resources Adult Core Set Measures CMCS Informational Bulletin outlining 2014 update to Adult Core Set 2013 Technical Specifications and Resource Manual Adult Medicaid Quality Grant Program States can submit measurement questions to: [email protected] 2014 Adult Core Measure Set NQF # Measure Name Measure Steward 0039 Flu Shots for Adults Ages 50-64 NCQA n/a Adult BMI Assessment NCQA 0031 Breast Cancer Screening NCQA 0032 Cervical Cancer Screening NCQA 0027 Medical Assistance with Smoking and Tobacco Use Cessation NCQA 0418 Screening for Clinical Depression and Follow-Up Plan CMS 1768 Plan All-Cause Readmission NCQA 0272 PQI 01: Diabetes, Short-Term Complications Admission Rate AHRQ 0275 PQI 05: Chronic Obstructive Pulmonary Disease (COPD) Admission Rate AHRQ 0277 PQI 08: Congestive Heart Failure (CHF) Admission Rate AHRQ 0283 PQI 15: Adult Asthma Admission Rate AHRQ 0033 Chlamydia Screening in Women Ages 21-24 NCQA 2014 Adult Core Measure Set (continued) NQF # Measure Name Measure Steward 0576 Follow-Up After Hospitalization for Mental Illness NCQA 0469 PC–01: Elective Delivery Joint Commission 0476 PC–03 Antenatal Steroids Joint Commission 2082 Viral Load Suppression HRSA 0018 Controlling High Blood Pressure NCQA 0063 Comprehensive Diabetes Care: LDL–C Screening NCQA 0057 Comprehensive Diabetes Care: Hemoglobin A1c Testing NCQA 0105 Antidepressant Medication Management NCQA 1879 Adherence to Antipsychotics for Individuals with Schizophrenia CMS 0021 Annual Monitoring for Patients on Persistent Medications NCQA 0006/000 7 CAHPS Health Plan Survey v 4.0—Adult Questionnaire with CAHPS Health Plan Survey v 4.0H—NCQA Supplemental AHRQ, NCQA 0648 Care Transition—Transition Record Transmitted to Health Care Professional AMA-PCPI 0004 Initiation and Engagement of Alcohol and Other Drug Dependence Treatment NCQA 1391 Prenatal and Postpartum Care: Postpartum Care Rate NCQA 19