* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download I. Testes
Survey
Document related concepts
Transcript
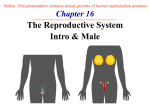
Male Reproductive Systems: For Discussion: True or False? 1. Sperm cells in the female reproductive tract are considered by a woman’s immune system to be “non-self” and are attacked by her phagocytic white blood cells. True 2. Sperm cells are considered by a man’s immune system as “non-self” and are attacked by a man’s own white blood cells. True 3. A woman, in her reproductive lifetime, has the potential to produce about 500,000 eggs, but she will only ever use about 500. True 4. The average man, in a single average ejaculation of semen, emits more reproductive cells than the average woman produces in her reproductive lifetime. True, about 420 million per average ejaculate, he produces about 4 million/hour 5. Only one sperm may fertilize an egg in humans. True 6. Only about 1 in 42,000 sperm, or 0.00238 % of the sperm in an average ejaculation reach the egg. True The Male Reproductive System -produces and maintains sperm cells and transports them, along with their supporting fluids, into the female reproductive tract -produces and secretes male sex hormones Ureter Large intestine Urinary bladder Seminal vesicle Pubic bone Penis Ejaculatory duct Ductus (vas) deferens Urethra Prostate gland Corpus cavernosum Bulbourethral (Cowper’s) gland Anus Corpus spongiusum Glans penis Epididymus Prepuce (foreskin) Testis Scrotum The Male Reproductive System I. Testes -male primary sex organs -produce sperm and male sex hormones -housed within the scrotum -form within the abdominal cavity, stimulated by Ever hear of a “gubanatorial testosterone to descend into the scrotum 1-2 months election”? It’s before birth through the inguinal canal, led by the from the Latin for “steersman!” gubernaculum, which anchors the testis to the bottom of the scrotum Rx – Inguinal hernia -in about one-fourth of males, the pouch of peritoneum that moves through the inguinal canal remains open; allowing for a loop of intestine to be forced through the inguinal canal under great vaginal process pressure, like getting dogpiled in a football game -if the loop becomes constricted in the inguinal canal, the blood supply can be cut off, creating a strangulated hernia, in which the tissue will die without prompt surgical treatment I. Testes Rx – Cryptorchidism -failure of one or both of the testes to descend into the scrotum, which has an internal temperature of about 34.4 °C (94 °F) -internal body temperature 37 °C (98.6 °F) is too high for sperm to survive -sperm-producing cells degenerate, leading to infertility -leads to increased risk of testicular cancer I. Testes -structure A. Tunica albuginea -tough, white fibrous capsule surrounding each testis and subdividing the inside of each testis into about 250 lobules B. Seminiferous tubules -each lobule contains 1-4 coiled seminiferous tubules, each about 70 cm long (210 total meters), which Ductus deferens unite to form the rete testis, which in Epididymus turn form ducts that empty in the epididymus, which continues into the ductus deferens Rete testis -cells with the walls of the seminiferous tubules called spermatogonia divide by mitosis when stimulated by testosterone to produce primary spermatocytes, Seminiferous tubules Tunica which divide by meiosis to produce albuginea spermatozoa Spermatogonia Spermatozoa I. Testes B. Seminiferous tubules Spermatozoa Sustentacular cells Nucleus of sustentacular cell Spermatid Secondary spermatocyte The sustenacular cells and the tight junctions between them form the blood-testis barrier, which prevents access to the sperm by the white blood cells, which would attack them as “nonself” Primary spermatocyte Tight junction New Type B spermatogonium New Type A spermatogonium Basement membrane I. Testes B. Seminiferous tubules 1. Spermatogenesis -creation of sperm within the walls of the seminiferous tubules -beginning at puberty, an increase in testosterone triggers meiosis of the primary spermatocyte n n n n n=23 2n=46 Meiosis I Reduction division Meiosis II Mitotic division Maturation n n n n n=23 Primary spermatocyte Secondary spermatocytes spermatids spermatozoa I. Testes B. Seminiferous tubules 1. Spermatogenesis -from puberty to old age, a man can produce about 100 million sperm per day, average sperm count in semen is 120 million sperm per mL, less than 20 million sperm per mL = infertility During synapsis of homologous chromosomes during Prophase I, crossing over occurs, resulting in new genetic variation I. Testes B. Seminiferous tubules 1. Spermatogenesis a. Sperm structure i. Head -made up of the acrosome, which allow the sperm to digest its way into the egg, and a highly compacted nucleus, which Acrosome Head contains 23 chromosomes in its diffuse Nucleus state chromatin ii. Midpiece -contains mitochondria to provide Midpiece energy to lash the tail iii. Tail -a single flagellum Tail (flagellum) I. Testes Rx – Testicular Cancer -accounts for only about 1% of the cancers in men in the U.S., causing about 390 deaths each year -most common type of cancer in young men, ages Seminiferous tubules 15-34, arises from epithelial tissue of tubules -treated with the surgical removal (orchiectomy) of the affected testicle and radiation and/or chemotherapy to prevent reoccurence -cured 95% of the time -incidence is on the rise for all men, incidence is the highest among white men, especially those of Scandanavian descent Interstitial cells C. Interstitial Cells -cells of Leydig -lie between seminiferous tubules in testes -produce and secrete into the bloodstream the male sex hormones II. Epididymides -long (6 m) coiled tubules emerge from top and descend down the back of the testes -continuous with ducts inside testes, receive the immature, non-motile sperm from seminiferous tubules -cells of epididymis secrete glycogen and other substances that support sperm and promote their maturation, rhythmic peristaltic contractions move sperm down the length of the epididymis, violent peristaltic contractions during emission of orgasm propel sperm into ductus deferens Epididymis III. Ductus (Vas) Deferentia -muscular tubes 45 cm long leading from the lower end of the epididymis and through the inguinal canal to fuse with the duct of the seminal vesicle to form the ejaculatory duct -sheathed together with the veins, arteries, and nerves that supply the Seminal testes to form the spermatic cord, vesicle which testes are suspended from Ductus deferens -violent peristaltic contractions during emission propel sperm into ejaculatory duct to mix with the secretions of the Epididymis seminal vesicles and prostate gland to form semen, which fills the urethra Ejaculatory duct IV. Seminal Vesicles -contract during emission to secrete a slightly alkaline fluid to prevent semen from becoming too acidic as it travels through the urethra -seminal fluid also contains fructose to provide energy for the sperm as they swim and prostaglandlins, which stimulate muscle contractions within the female reproductive Seminal tract, aiding in the movement of sperm towards vesicle the egg (can also help initiate labor) Ductus deferens Epididymis Ejaculatory duct V. Prostate Gland -contracts to secrete a thin, milky alkaline fluid that forms the bulk of semen, neutralizing acidic waste products produced by the sperm that inhibits their motility -alkalinity enhances motility of sperm and neutralizes the much more acidic contents of the vagina to protects sperm Seminal vesicle Ductus deferens Epididymis Prostate gland Ejaculatory duct V. Prostate Gland Rx – Benign Prostatic Hypertrophy -enlargement of the prostate gland in 50% of all men over age 50, and 90% of all men over age 70 -pressure on bladder leads to increased frequency of urination and urine retention, which can lead to infection, bladder stones and kidney disease -can also indicate prostate cancer Rx – Prostate Cancer -most common cancer in men after skin cancer, 235,000 new cases per year, 70% in men over age 65, causing 27,000 cancer deaths per year -more common in African American men than in Caucasian men, genetic tendency perhaps linked to a diet high in saturated fat -treated by surgical removal of entire prostate and sometimes surrounding lymph nodes, and radiation VI. Bulbourethral (Cowper’s) Gland -secretes a small amount of mucus-like fluid in response to sexual stimulation, which cleanses the urethra of urine residues prior to ejaculation and provides lubrication for sexual intercourse Seminal vesicle Ductus deferens Epididymis Prostate gland Ejaculatory duct Bulbourethral glands VII. Scrotum -houses testes -protects and regulates temperature at 34.4 ºC (94 ºF) -dartos muscle contracts to elevate testes as part of the sexual response to shorten distance sperm have to travel during emission, contracts to elevate testes to protect them from cold and to protect them from physical damage in response to activation of ‘fight-orflight’ mechanism -padded with fat to protect testes VIII. Penis -male copulatory organ -houses urethra, which conveys urine and semen to the outside of the body -contains erectile tissues, which enable the penis to become engorged with blood so that it becomes erect and can penetrate vagina VIII. Penis A. Erectile tissues -Corpus cavernosa and Corpus spongiosum -fill with blood in response to sexual stimulation, as parasympathetic nerve impulses cause arteries leading into erectile tissues to dilate, increasing blood flow and at the same time pressing veins leading out of erectile tissues flat, accumulation of blood leads to erection Penis Corpus cavernosa Corpus spongiosum VIII. Penis B. Glans penis -cone-shaped distal end of penis -houses external urethral orifice -covered by the sheath-like prepuce, which is often removed at birth by the surgical procedure of circumcision -thin-skinned, with many sensory receptors for sexual stimulation Penis Corpus cavernosa Prepuce Glans penis External urethral orifice Corpus spongiosum VIII. Penis -during orgasm, the process of emission mixes sperm with the secretions of the seminal vesicles, prostate gland, and bulbourethral gland, filling the urethra with 2-5 mL of semen containing 240-600 million sperm -during ejaculation, skeletal muscles at the base of the erectile columns of the penis contract, increasing the pressure in the erectile tissues, and forcing semen from the urethra at a speed of 29 kph (18 mph), depositing semen far up into vagina near cervix Rx – Erectile Dysfunction -impotence, the inability of the penis to become erect or sustain an erection -usually a complicating factor of diabetes, paralysis, prostate surgery, or drug use -most often treated with therapy by drugs like Viagra®, which blocks the enzymatic breakdown of the neurotransmitter cGMP, which relaxes the arteries leading into the erectile tissues, allowing them to dilate