* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Conjunctivitis
Survey
Document related concepts
Transcript
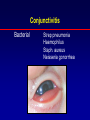
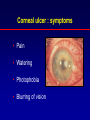
Red Eye in Children Diagnosis and Management Ronit Friling M.D. SCHNEIDER MEDICAL CENTER ילדים Red Eye Disorders: Non-Vision -Threatening Conjunctivitis Blepharitis Subconjunctival hemorrhage Dry eyes Chalasion Corneal abrasions (most) Red Eye Disorders: Vision -Threatening Corneal infection Iritis Scleritis Acute glaucoma Hyphema Foreign body Anamnesis: • How long has the eye been red? • Does the vision seem to be okay ? • Do the eyes move normally ? • Is the infection in both eyes ? Anamnesis: • Does the child wear contact lenses ? • Is there a history of trauma ? • How long has the eye been red ? • Is the pupil round ? Dacryocystitis Naso Lacrimal Duct Obstruction Signs: Red painful swelling above lacrimal sac History of chronic eye watering Dacryocystitis Dacryocystitis Dacryocystitis Pathogens: Staphylococcus aureus, Strep pneumonia Treatment: conservative until 1 yr (antibiotics after culture, hygiene, massage?) Surgery at 1 yr - probing, silicone tubes, rarely DCR Conjunctivitis Bacterial Chlamydia Viral Allergic Conjunctivitis: symptoms & signs Symptoms: Sore, red, sticky eyes. Signs: Red conjunctiva, discharge. Viral & Chlamydial: Follicles, swollen lids, enlarged preauricular node. Conjunctivitis Bacterial Strep pneumonia Haemophilus Staph. aureus Neisseria gonorrhea Conjunctivitis Chlamydia Ophthalmia Neonatorum Any conjunctivitis during the first month of life Ophthalmia Neonatorum Etiology thought to have been acquired in birth canal: chlamydia, gonococcus, other bacteria Regard chlamydia and gonococcus as systemic disease and treat systemically Corneal ulcer : symptoms • Pain • Watering • Photophobia • Blurring of vision Corneal ulcer : signs • Red eye • Epithelial defect fluorescein staining • Corneal infiltrate • A/C inflammation, Hypopyon Corneal ulcer : risk factors • Contact lens wear • Dry eye • Insesitive eye • Blepharitis • Herpes virus- zoster, simplex Corneal ulcer : risk factors • Ectropion • Bell’s palsy • Corneal surgery, injury, foreign body Corneal ulcer : pathogens • Bacterial Pseudomonas Staphylococcus Streptococcus • Viral Herpes simplex • Fungal Corneal ulcer : treatment Referral to hospital - culture Admission Urgent topical antibiotic treatment: Cefazolin - Gentamicin drops Fluoroquinolon (ciloxan, oflox) drops q 1h - q 1/2h Conjunctivitis Viral Adenovirus Herpes simplex virus Herpes simplex keratitis Primary infection during childhood Herpes simplex keratitis Usually unilateral Dendritic pattern Often recurrent Corneal sensation reduced. Conjunctivitis: treatment Bacterial Chloramphenicol Phenymixin (Chloramphenicol + polymixin B) Gentamicin Bamyxin Chlamydia Topical Tetracycline 3 weeks Systemic Tetracycline 2 weeks Viral As bacterial or topical steroids Conjunctivitis: treatment Herpes simplex keratitis : treatment Topical Acyclovir 3% ointment 5 times / day Systemic Acyclovir 400 mg x 5/day in immunesupressed or severe infection. Herpes zoster ophthalmicus Usually above age 50 Immune supressed - HIV Rx: PO zovirax 800 mg X 5 Orbital & periorbital celullitis Signs: periorbital swelling and redness fever lethargy proptosis decreased eye motility abnormal pupillary reaction optic nerve swelling or pallor Orbital & periorbital celullitis Orbital & periorbital celullitis Signs: Limitation of abduction of involved eye Orbital & periorbital celullitis Orbital & periorbital celullitis Etiology: Sinusitis Trauma URI Orbital & periorbital celullitis Treatment: Periorbital PO antibiotics Orbital – Hospitalization – CT – IV antibiotics Blunt Ocular Trauma: Anterior segment Iris - hyphema - mydriasis - iridodialysis - angle recess VERNAL KERATOCONJUCTIVITIS (VERNALIS) Usually bilateral Seasonal Atopic history: Asthma, rhinitis, atopic dermatitis Palpebral : cobble stones VERNAL KERATOCONJUCTIVITIS (VERNALIS) Treatment of exacerbations Topical steroids Systemic steroids Lubricants Mast cell stabilizers: Sodium chromoglycate Alomide Zaditen Livostin Red Eye in Children