* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Microsoft PowerPoint - 2-2013 Patient Safety Goals [Compatibility
Survey
Document related concepts
Transcript
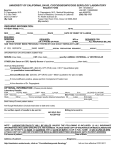
Use at Least Two Patient Identifiers Name & MRN WHEN Administering meds, blood, or blood components Transfusions require 2 person check Collecting blood samples & other specimens Label containers used for blood & other specimens in the presence of the pt. Providing other treatments or procedures Eliminate Transfusion Errors Before initiating a blood or blood component transfusion: Match the blood or blood component to the order Match the patient to the blood or blood component Patient identifiers: two licensed individuals (RN, LVN, MD, CRNA, etc.) must positively identify blood products with patient’s name and medical record number as printed on the patient’s ID band in the presence of the patient. Check the blood against tag on unit for patient's name, medical record number, group and type of blood, number of unit and date of expiration. RN enters second verifier’s name into Health Connect prior to transfusion Any discrepancies Stop - send unit back to Blood Bank Improve the Effectiveness of Communication among Caregivers Verbal Orders & Test Results Write down (pull up from computer screen) orders/results Read them back to the person providing them Get confirmation from the person Critical Tests & Results Communicate results ASAP to Provider Document TIME of notification Provider must respond to values within ONE hr. Escalate if response is not received in timely manner when paging Provider to give results Improve the Effectiveness of Communication among Caregivers Follow Hand-off Communications Must include opportunity to ask & respond to questions Use SBAR whenever possible Review anything pertinent to pt’s care Give next caregiver a better idea of what to expect Teamwork Patient & nursing personnel at ease Does not replace written report or physical assessment of the pt. SBAR – Situational Briefing Situation – State the problem clear and concise Background – Provide Info that is brief and to the point Assessment – What do you think/know Recommendation – Proposed action (What do you want & when) Improve the Effectiveness of Communication among Caregivers: Do Not Use/Accept Abbreviation List Do Not Use Potential Problem Use Instead U, u (unit) Mistaken for “0” (zero), the Write (or accept order) number “4” (four) or “cc” "unit" IU (International Unit) Mistaken for IV (intravenous) or the number 10 (ten) Write (or accept order) "International Unit" Q.D., QD, q.d., qd (daily) Q.O.D., QOD, q.o.d, qod (every other day) Mistaken for each other Period after the Q mistaken for "I" and the "O" mistaken for "I Write (or accept order) "daily" Write (or accept order) "every other day" Trailing zero (X.0 mg) Lack of leading zero (.X mg) Decimal point is missed Write (or accept order) X mg Write 0.X mg MS MSO4 and MgSO4 Can mean morphine sulfate Write (or accept or magnesium sulfate order)"morphine Confused for one another sulfate" Write "magnesium sulfate" Joint Commission, 2004 7 RIGHTS of Medication Safety 1. RIGHT Patient (2-identifiers!) 2. RIGHT Route 3. RIGHT Dose 4. RIGHT Time 5. RIGHT Medication 6. RIGHT Reason 7. RIGHT Documentation Improve the Safety of Medication Use Be familiar with steps to prevent errors due to look- alike/sound-alike meds & high alert meds Be AWARE of look-alike/sound-alike medications Be AWARE of high alert medications Label all meds/solutions containers on & off sterile field Review safety measures for anticoagulation therapy Properly Label & dispose Multi-dose & Single-use vials Be familiar with Black Box Warnings Practice the 7 Rights of medication safety LABEL Requirements Labeling MUST occur when any med or solution is transferred from the original package to another container 1. 2. 3. 4. 5. Name of drug/solution Strength of medication Amount Expiration Date: 28 days Initials of preparer Look-Alike Sound-Alike Medications General Recommendations Verbal & phone orders are Discouraged unless truly necessary Must be read-back per required verbal order procedure Products are NOT stored next to each other in pharmacies, pt. care units, clinics, & pt. homes Report errors or potentially hazardous conditions by completing a UOR Assure meds are clearly labeled High Alert Medications: Safety Practices Independent Double Check - Performed independently by two qualified licensed practitioners Right Pt identification using two identifiers (name, MRN) Right Drug Right Dose, Right Route & Time of administration Verify setting, rate on IV pump (use guardian mode) Document on the MAR & Health Connect Time Out – a period of time immediately before administration /procedure when two qualified practitioners, at pt’s side, Check special equipment or requirements Correct pt identity, side/site, pt. position Agreement on the med administration/procedure with pt./family Document Time Out on medical record Medication Safety Verification Record – documentation tool to record Independent Double Checks & Time Outs Hand-off – an interactive process of passing pt. specific info from one caregiver to another Improve the Effectiveness of Communication among Caregivers Follow Hand-off Communications Must include opportunity to ask & respond to questions Use SBAR whenever possible Review anything pertinent to pt’s care Give next caregiver a better idea of what to expect Teamwork Patient & nursing personnel at ease Does not replace written report or physical assessment of the pt. SBAR – Situational Briefing S B A R Situation Background Assessment Recommendation (or Request) Anticoagulation Therapy Safety Pts. on warfarin receive baseline International Normalized Ration (INR) to monitor & adjust therapy IV Heparin is administered using an IV pump Independent Double Check required for IV Heparin – before start, with each change of container or rate, & at change of shift handoffs Document “Double Check Required” on the eMAR (Health Connect) Baseline & ongoing lab tests required for heparin therapies Pt./Family Education Follow-up monitoring Compliance Dietary restrictions Potential adverse drug reactions & interactions Specimen Equipment and Supplies Obtain containers, labels, requisition forms, and the preservative or fixative appropriate for the type of testing or delivery. Collection containers must be impervious and of an adequate size to easily contain a specimen Sterile receptacles and equipment must be used for specimens when sterility must be maintained Specimen Labeling Identify patient using two verifiers: Verify with specimen collector • Name • Source/site of specimen • Medical Record Number • Name of test to be done • Timing of test: Routine or Stat Specimen Labeling Key Steps: The specimen label is applied by the collector or clinical support staff witnessing the collection Label any specimen collected in the back office in the presence of the patient Unlabeled specimens cannot be removed from the collection area (e.g. exam room) to another area for labeling Labels may be printed or handwritten Handwritten labels must be legible and written in black ink Requisition/Transmittal Slip and Label Criteria Reacquisition/Transmittal Slip must contain: Full name, MR number, Date, time of collection, Specimen source/type, name of the collector, clinical staff Initials. Use pencil to label slides and slides must contain the patient’s complete name and MRN Label is placed on each specimen container and NOT on the lid or transport bag Unlabeled or mislabeled specimens will not be tested unless they meet the “exceptions list criteria” e.g. .body fluids other than blood or urine, tissue, bone marrow, blood for drug levels, blood cultures, specimens) Chain of Custody Establish mechanisms for chain of custody to ensure accountability Complete transmittal slip and send with specimen to lab Consistent communication patterns should be established between personnel at change of shift or relief Multi Dose Vials Proper Labeling & Disposal Write date 28 days from initial opening Write date 28 days from initial opening Discard on 28th day or if sterility compromised Examine vial for visible signs of contamination or deterioration Multidose Vial Adapter Good for 24hrs only Withdrawals from vial MUST Use sterile technique DO NOT leave needle or needle sheath in the vial top for ease of access! Single-Dose Vials Proper Labeling & Disposal Contain ONLY ONE dose of medication, use ONCE & DISCARD after use! Single- dose vials are meant for Check mfr. exp. Date BEFORE use ONE time DO NOT use SINGLE-use vials as MULTI-dose vials! All withdrawals require sterile technique use ONLY! Black Box Warnings Emphasize the potential health risk of a drug FDA requires drugs with serious, life-threatening side effects, or there are more risks than most other prescription drugs carry a black box warning! Black box warnings have a heavy bold line or box box around the warning. Black Box Warning These drugs are effective, although high risk, its benefits outweigh the risks. KP HealthConnect provides a hyperlink that links to drug information – this is where the Black Box warning will appear. Contact Pharmacy for questions. Accurately & Completely Reconcile Medications Across the Continuum of Care All pt’s must have complete list of current meds, including herbal remedies, vitamins, OTCs, etc., as part of initial assessment Medication reconciliation must be complete at every visit Medication reconciliation must occur whenever a pt. is transferred or there is a change in the level of care Reduce the Risk of Health Care Associated Infections Wash hands for 15 seconds when visibly soiled or contaminated, otherwise use waterless gel, alcohol based hand rub Keep nails short and clean Use only approved lotion Wear gloves – Latex-free Prevent surgical site infections: Use appropriate sterile/aseptic technique, wash hands, use electric clipper for hair preps Decontaminate hands BEFORE Contact w/pt’s Donning sterile gloves associated urinary tract infections Secure catheters for unobstructed urine flow and drainage Maintaining the sterility of the urine collection system Decontaminate hands AFTER Contact with pt. & objects close to pt. Removing gloves Taking a break Prevent indwelling catheter- Reduce the Risk of Health Care Associated Infections Be AWARE! WASH with CARE! 1. WET hands with water 2. Apply hand wash – 1 pump 3. Lather & Wash – 15 seconds 4. Rinse both sides of hands with water 5. Dry hands 6. Shut off faucet with hand towel Follow the Universal Protocol Conduct pre-procedure verification process Involve patient, verify consent for procedure Check for correct patient, site, procedure Mark procedure site – done by licensed practitioner performing procedure “X” marks the site! TIME-OUT performed prior to starting procedures DOCUMENT Universal Protocol & Time-out Improve the Safety of Clinical Alarms Clinical alarm systems are intended to alert caregivers of potential patient problems, but if they are not properly managed, they can compromise patient safety. This is a multifaceted problem. In some situations, individual alarm signals are difficult to detect. Many patient care areas have numerous alarm signals and the resulting noise and displayed information tends to desensitize staff and cause them to miss or ignore alarm signals or even disable them. Monitor and respond to alarms. Do not turn off alarms unless you have authority to do so. Identify patients at Risk for Suicide Suicide of a patient while in a staffed, round-the-clock care setting is a frequently reported type of sentinel event. Identification of individuals at risk for suicide while under the care of or following discharge from a health care organization is an important step in protecting these atrisk individuals. 1. Conduct a risk assessment that identifies specific patient characteristics and environmental features that may increase or decrease the risk for suicide. 2. Address the patient’s immediate safety needs and most appropriate setting for treatment. 3. When a patient at risk for suicide leaves the care of the hospital, provide suicide prevention information (such as a crisis hotline) to the patient and his or her family.