* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Psoriasis
Survey
Document related concepts
Transcript
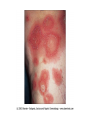
An Overview of Psoriasis Rich Callahan MSPA, PA-C Fletcher Allen Health Care, Dept. of Dermatology Burlington, Vermont ICM I – Summer 2009 Clinical Overview of Psoriasis: What Is It? • True understanding involves knowing the pathophysiology, which boils down to 3 characteristics: • The disease you see clinically is a disorder of cellular differentiation and kinetics • Psoriasis is mediated by autoimmune elements which are partially understood. • Psoriasis is passed on genetically Epidemiology: Psoriasis in U.S. • 5 to 7 million Americans have it • 150,000 to 260,000 new cases/year – mean age at presentation is 28 • 1.7 million treated – 600,000 of them for moderate/severe disease • 400 Psoriasis-related deaths/year. (Toxicity of medications > Suicide.) • (Data from Nat’l Psoriasis Foundation – Data on File) Classification • Falls under the category of papulosquamous diseases – skin conditions whose primary features are scaling papules and plaques. • There are over a dozen distinct subtypes of psoriasis: Chronic plaque, guttate, generalized pustular, scalp sebo-psoriasis, palms and soles (both plaque and pustular,) inverse psoriasis, nail psoriasis, psoriatic arthritis, light-sensitive, erythrodermic, Reiter’s syndrome. We will focus on 3 most common Psoriasis subtypes • Chronic Stable Plaque Psoriasis – Most common subtype. What most people visualize when they think of Psoriasis. • Guttate Psoriais – Acute papulosquamous eruption. Can evolve into chronic Psoriasis. • Palmoplantar Pustular Psoriasis (PPP) – Debilitating, chronic eruption of the palms and soles. Clinical Presentation of Psoriasis • Chronic Stable Plaque: Relatively fixed and stable pink to erythematous scaling papules and plaques primarily on trunk, scalp and flexor extremities. Lesions are sharply marginated and often slightly raised above surrounding skin. May/may not be mildly pruritic. Rarely affects face, genitals, soles of feet. Lesions occassionally correspond to areas subject to repetetive trauma. Chronic Stable Plaque Psoriasis Most common form of the disease with a wide range in severity; can be a small, fixed plaque that doesn’t move or change. Can also be large, confluent groups of papules and plaques covering 20-70% of a patients BSA (body surface area.) • The problem again is unpredictability: A patient with one stable plaque can suddenly explode into 20-30% BSA involvement with no apparent cause or explanation, at any stage in life. Life stress/ETOH can be precipitants! Clinical Presentation of Psoriasis • Guttate: Sudden eruption of brightly erythematous, round, scaling papules, usually 1cm or less in diameter, trunk and extremities. Again, sharply marginated. Spares palms and soles. Usually preceded by streptococcal or viral URI. Often a patients first experience with their psoriasis. Patients often seem sick, with a history of “not quite getting over that cold a few weeks ago.” Guttate Psoriasis • Comes from the Latin word for “raindrop” as patients with this type of psoriasis literally look like they have drops of red paint splattered haphazardly on their trunk and extremities. • Lesions are clearly defined and often brightly erythematous, though less firm and scaly than plaque psoriasis. • Often associated with preceding streptococcal or viral pharyngitis, URI or tonsillitis. • Sometimes it is a young person’s first experience with their psoriasis. Important to instill realistic expectations in these patients as many develop chronic plaque disease later. Presentation of Guttate Psoriasis • Even if patients don’t give a history/show signs of prior URI/pharyngitis, still a good idea to do throat culture, lymphatic exam and treat empirically with antibiotics. • Many patients will improve after a short course of antibiotics even if they don’t seem sick. • Throat cultures sometimes positive for strep. There are two patterns to this presentation, and two different prognoses: • 1.) Middle to older aged patient with long history of mild chronic stable plaque psoriasis who gets a nasty URI and has sudden guttate flare. Good prognosis for return to baseline after treatment with antibiotics. • 2.) Young adult without prior history of psoriasis gets nasty URI and has sudden guttate flare. Often alarming, often misdiagnosed as infectious. Guttate lesions often slow to improve with slow shift into chronic plaque psoriasis. Clinical Presentation of Psoriasis • Palmoplantar pustular (PPP): Deeply seated, non-rupturing pustules on palms/soles which emerge over time at skin surface to form scale/crust and then slowly peel. Pustules are sterile, and only infected secondarily. Tends to run a chronic course. Resistance to treatment is common. Patients with severe disease can become depressed secondary to difficulty performing at work and ADL’s. Psychological Impact of Moderate/Severe Disease • Patients with extensive BSA involvement often afraid to be in public or wear revealing clothing. • Some patients shed scale constantly onto clothing, furniture, floors, etc. • Many patients eventually become depressed if disease poorly controlled. • Aggressive treatment of the patient’s disease is often warranted in these cases as the severity of the disease justifies the risks/side effects inherent in the treatments. • Patients often motivated to try anything that might be effective. It is well documented that drugs can exacerbate Psoriasis • • • • • ETOH Beta-blockers Lithium carbonate Antimalarials Interferons Clinical Pearl – Auspitz’s Sign • A patient presents with new onset of an erythematous, crusted, keratotic plaque on the left anterior thigh. Suspecting fungal disease, the PA scrapes the plaque with a #15 blade to collect scale for KOH microscopic exam. The dry, white scale is easily scraped away, yielding numerous tiny, brisk, pinpoint bleeders in the inflamed tissue below. This is called Auspitz’s sign, in which inflamed, dilated capillaries of the hyperactive epidermis are traumatized. Although it isn’t considered diagnostic of psoriasis, Auspitz’s is an important hint to look further in that direction for a diagnosis. Pathophysiology of Psoriasis – an expert summary • As explained by Charles Camisa, MD, in his book Handbood Of Psoriasis: • “Psoriasis is the result of a hyperproliferation of the epidermis, concommitant inflammation and vascular changes, which occur in response to the proper combination of genetic and environmental pressures.” Camisa, con’t, on pathogenesis of psoraisis • Psoriatic epidermis has 26.6% of the proliferative cells in the DNA synthesis (S) phase compared to 7.8% in normal skin. The growth fraction increases from 60 to 100% and the size of the population of proliferative cells is doubled, but the main defect in epidermal kinetics is the overall eight-fold increase in the germinative cell cycle compared to that occuring in normal skin. The result is a cell cycle shortened from 311 to 36 hours and an epidermal turnover time, that is the time it takes a basal cell reach the stratum corneum, accelerated from 27 to 4 days.” (From Camisa, Charles MD, Handbook of Psoriasis, Blackwell Pub., 2004. p. 45) There is a hyperproliferation of epidermal cells, but that’s half the story • Also a disorder of cell differentiation. • Granular layer is reduced or absent and there is a massive overproduction of keratin known histopathologically as hyperkeratosis and parakeratosis. • This process creates the thick, white scaly plaques we see in psoriasis. The pathophysiology of psoriasis is pretty well studied, but there is a lot to learn about its autoimmune basis and underlying etiology. • Multiple physiologic and immune entities have been found to play a role in the pathway that mediates the development of psoriasis: Polymorphonuclear leukocytes, neuropeptides, T-lymphocytes, inflammatory cytokines, interleukins, TNF-alpha cells, etc. • The newest class of psoriasis medications, the “biologics,” target specific players in this pathway. • It’s not so much that medical science knows exactly what’s going on, but rather we do know that when certain immune elements in the pathway are blocked, patients psoriasis gets better (sometimes.) Diagnosis of Psoriasis • Usually a clinical diagnosis, but skin biopsy is almost always diagnostic. • New onset Guttate Psoriasis gets throat culture to r/o chronic strep infection. • Occassionally need to biopsy PPP to differentiate from dyshidrotic eczema. • Isolated, unilateral lesion should get scraped to exclude fungus. Treatment of Plaque Psoriasis • Moderate to high potency topical steroid creams, gels and ointment. Classified by potency as I-VII-strong antiinflammatories • Topical calcipotriene inhibitors (dovonex) – thins epidermis • Topical coal tar derivatives (anthralin/LCD) and retinoids (Tazorac) – anti -inflam • Phototherapy with narrowband UVB and PUVA (“psoralen and ultraviolet light”) • Methotrexate, a potent antimetabolite and immune suppressant. • Cyclosporine, a potent immune suppressive drug Newest on the scene: The Biologics • Self-injected by patient once or twice weekly, or bimonthly infusion at IV center. • Expensive drugs – made of engineered recombitant proteins. • We don’t completely understand why they work, but for some patients they provide dramatic improvement, without all the side effects inherent in older immusuppressant medications like methotrexate or cyclosporine. Newest on the scene: The Biologics • Many poorly understood risks/SE’s including reactivation of prior malignancy/TB. Increased risk of developing lymphomas/cancers in clinical trials. Evidence of “unmasking” of prior latent demyelinating disease – significance not fully understood. • Should only be administered by dermatologists/derm PA’s who are experienced with them. How are Biologics Made? • Derived from whole human cells, blood, hybridomas, recombitant DNA technology. • Produced within living organisms • Usually large molecules • Always administered by injection or IV The Theory Behind the Biologics The newly developing psoriasis lesion is precipitated by an autoimmune reaction wherein there is a genetic defect inherent in the interaction between keratinocytes, macrophages (otherwise known as antigen presenting cells, or APC’s) and T-lymphocytes (T-Cells.) For reasons that are poorly understood, the macrophages appear in the epidermis and proceed to identify the keratinocytes as foreign antigens. These antigens are then presented to T-lymphocytes which form large populations which then incite the inflammation of psoriasis. Large populations of activated T-Cells are found in bases of Psoriasis plaques. We don’t have time today for a lecture on the workings of the immune system in depth. • Let it suffice to say that numerous experimental studies and clinical trials have shown that Psoriasis is a T-Cell mediated disease. • “Biologic” Psoriasis drugs target and disable particular steps along the pathway of T-Cell activation and homing in on target tissues (keratinocytes in skin) which ultimately results in clinical disease improvement in most patients. The Biologics • • • • • • Enbrel (etanercept) Amevive (alefacept) Humira (adalimumab) Remicade (infliximab) Raptiva (efalizumab) The suffix at the end of the trade name denotes class of protein • -ximab = chimeric monoclonal antibody • -zumab = humanized monoclonal antibody • -umab = human monoclonal antibody • -cept = receptorantibody fusion protein Treatment of Guttate Psoriasis • Oral antibiotics such as penicillin, erythromycin and azithromycin. • Topical steroids • Narrowband UVB and natural sunlight. • Tincture of time as majority of cases will resolve spontaneously in a 4-6 wk period. • Be ready to explain to younger patients that Guttate Psoriasis can develop into chronic stable plaque psoriasis Palmoplantar Pustular Psoriasis (PPP) Treatment • This is a stubborn disease – I have several patients on multiple medications where clinical improvement is gauged by ability to perform ADL’s/depression. • First-line is super-potent topical steroid ointments under occlusion at qhs under plastic wrap. Sometimes it works. • Can try topical coal tars and UV light treatments • Most effective for mod/severe disease is acitretin (Soriatane) an oral retinoid – slows growth of epidermis. • Combination therapy is usually the rule.