* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Survey
Document related concepts
Transcript
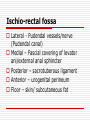
ANATOMY OF THE FEMALE PELVIC FLOOR AND PERINEUM Dr. A. O. FAWOLE DEPT. OF OB-GYN UCH Pelvic Floor and Perineum Anterior perineum Posterior perineum Pelvic Floor Perineum Borders of pelvic outlet Anteriorly – ischiopubic rami Posteriorly – coccyx and sacro-tuberous ligament Division (ischial tuberosities) Anterior perineum (urogenital triangle) Posterior perineum (anal triangle) Structures overly perineal membrane Anterior Perineum Structures of the Vulva Mons Labia Clitoris Vestibule Erectile structures Vulva Mons Hair-bearing skin Cushion of adipose tissue Labia majora Hair-bearing skin Termination of round ligaments of uterus Labia minora Hairless skin fold Lacks bed of adipose tissue Forms prepuce/frenulum of clitoris Glands of the vulva Labia majora – sebaceous gland Sweat glands Bartholin’s glands Superficial compartment Space between subcutaneous tissues and perineal membrane Clitoris Crura Vestibular bulb/Bartholin’s gland Ischicavernosus (from ischial tuberosity) Bulbospongiosus (from perineal body) Superficial transverse perineal muscle Muscles contained in superficial perineal pouch The Perineal Membrane Triagular sheet in anterior half of pelvic outlet Dense fibromuscular tissue Previously called urogenital diaphragm Functions Supports pelvic floor Counteracts effects of raised intra-abdominal pressure Counteracts effects of gravity The Perineal Membrane Complete sheet in males Arises from ischiopubic rami Attachments Urethra Vagina Perineal body Limits downward descent Perineal Body Mass of connective tissue Synonym: central tendon of the perineum Located between vagina and anus Attachments Perineal membrane Superficial transverse perineal muscle Bulbospongiosus Levator ani Coccyx (via external anal sphincter) Posterior Perineum Posterior triangle Anus Anal sphincter Levator ani Ischio-rectal fossa Ischio-rectal fossa Lateral - Pudendal vessels/nerve (Pudendal canal) Medial – Fascial covering of levator ani/external anal sphincter Posterior – sacrotuberous ligament Anterior – urogenital perineum Floor – skin/ subcutaneous fat Pudendal Nerve/Vessels Similar channels Nerve arises from sacral plexus (S2- S4) Sensory Motor Artery: anterior division of internal iliac artery Branches Clitoral Perineal (largest branch: muscles/skin) Inferior rectal Anal Sphincter External anal sphincter Superficial portion Deep portion Internal anal sphincter Thickening of circular smooth muscle of anal wall Important during repair of third (fourth) degree perineal laceration The Pelvic Floor Demands of upright posture Support for pelvic structures Passage of fetus Openings for waste elimination Fibromuscular floor Visceral ligaments/fascia Levator ani/Pelvic Wall Levator ani most important muscle Pubo-rectal Pubo-coccygeal Coccygeal Origin: Posterior aspect of pubic bone, fascia of pelvic side wall, ischial spine Insertion: Perineal body, anal sphincter, coccyx Constitute pelvic diaphragm Surfaces covered by fascia Pelvic Floor Pubo-rectal and pubo-coccygeal most medial Pelvic diaphragm forms U-shaped layer of muscle Opening end of U directed anteriorly (urogenital sinus) Urethra Vagina rectum Pelvic supports Condensations of connective tissue or endopelvic fascia Cardinal ligament Uterosacral ligament Pubocervical fascia Clinical significance Prolapse of pelvic structures Damage Weakness Cardinal ligament Transverse cervical/Mackenrodt’s ligament Attaches lateral cervix/upper vagina to pelvic side wall Connective tissue/involuntary muscle Ureter in upper part Uterosacral ligament Postero-lateral attachment of lateral vaginal fornix/cervix/isthmus to sacro-iliac joint/third piece of sacrum Pubo-cervical fascia Extends between cardinal ligament and pubis Lateral to the bladder Significant in repair operation for cystocoele (anterior colporrhaphy)