* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download POST-TRAVEL CONSULTATION
Neonatal infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Typhoid fever wikipedia , lookup
Gastroenteritis wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Infection control wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Germ theory of disease wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
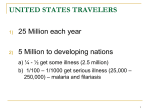
Post-Travel Health Consultation Dr Peter A. Leggat MD, PhD, DrPH, FAFPHM, FACTM, FFTM Associate Professor School of Public Health and Tropical Medicine James Cook University & Visiting Professor School of Public Health University of the Witwatersrand About the author Dr Peter Leggat has co-ordinated the Australian postgraduate course in travel medicine since 1993. He has also been on the faculty of the South African travel medicine course, conducted since 2000, and the Worldwise New Zealand Travel Health update programs since 1998. Dr Leggat has assisted in the development of travel medicine programs in several countries and also the Certificate of Knowledge examination for the International Society of Travel Medicine. Objectives of the session Review statistics Briefly review the sorts of problems travelers have abroad Examine why it may be important to see travelers if they are unwell on return and what policies may be applicable in practice Document some important aspects of the post-travel history and examination Some References Steffen et al. Manual of Travel Medicine and Health. Decker, 2003 Sec 4. Leggat et al. Primer of Travel Medicine. ACTM Publications, 2002 Ch. 19. The Continuum of Travel Medicine Pre-Travel Preventive Medicine Visitors Contingency During Travel Planning Treatment & Post-Travel Rehabilitation The Good News Most travelers report no major problems whilst travelling and most are asymptomatic on return Travelers are exposed to a variety of hazards Swiss Travelers 15-50% of travelers to developing countries report some illness or injury 8% in the study of 10,000 Swiss travelers consulted a medical officer 1% required hospitalization and 3% had time off work Insured Australian travelers* Approx 20,000 policies issued each year (incl. Exec. Gold) About 1600 claims (8%) 400 claims for emergency assistance (2%) 80 ER or clinic referrals (0.4%) 46 Hospital admissions (0.2%) 10 Aeromedical evacuations (0.05%) *Leggat et al (2005) Emergency assistance provided abroad to insured travellers from Australia. Travel Med Inf Dis 3: 9-17 Common things occur commonly Gastrointestinal-diarrhoeal diseases effecting 20-40% or more of short term travelers Respiratory tract infection Cutaneous infections Trauma and injuries (accidents- commonest cause of preventable death) Sexually transmitted infections Dental problems Others (remember malaria) Post-Travel Consultation Many travel related problems are self-limiting Why might it be important to see travelers who have an illness post-travel? The traveler may have a life threatening infections Malaria due to P. Falciparum Viral hepatitis Typhoid Amoebiasis/Amoebic liver abscess Legionnaire’s disease Melioidosis Rabies Others Travelers may have infections that pose a risk to public health Dengue (2-5 days) Lassa, Ebola and others (3-21 days) Japanese Encephalitis (3-7 days) Yellow fever (3-6 days) Typhoid (1-2 days) Malaria (Pv-10 days to year-relapses; Pf 10-28 days) SARS (2-10 days) Others It is important to develop policies in travel medicine Policy and procedures, including – Policy of follow-up of travelers – Policy on notifiable diseases – Policy on reporting adverse reactions – Policy on “eradication” treatment Policy on follow-up of travelers Do you see travellers Symptomatic on return? Symptomatic whilst aboard? Asymptomatic abroad and asymptomatic now? To complete immunization courses? It is important that the clinic have a written policy It is essential that travellers who become ill on return seek medical attention as soon as possible The traveller should be advised to inform the clinic that they have been or are currently traveling It is also important to ask if patients: “Have you been traveling recently?” Policy on reporting notifiable diseases and adverse reaction Is it a notifiable disease? Early liaison concerning suspected cases and formal notification to public health units Keep a list of notifiable diseases and reporting forms Document and report any possible serious adverse reactions to immunisations and chemoprophylaxic and other medications experienced by traveller whilst abroad Is the traveler part of a clinical trial? Travel medicine has assumed a major role in monitoring global trends in infectious disease, especially emerging infectious diseases Travel medicine networks GeoSentinel (ISTM/CDC) – May provide early warning of outbreak amongst travelers returning to disparate locations TropNet Europ WHO Local networks Other networks Eradication Policy Do you prescribe empiric “eradication” treatment? If so, what groups of travelers? Eradication “Treatment” Malaria - primaquine (check G6PD deficiency), (tafenoquine) Deworming agent for soil transmitted “roundworms” (consider strongyloides) Deworming agent for “flatworms”praziquantel Deworming agent for filariasis albendazole Antiprotozoal agent - giardiasis Others (?) Groups where eradication treatment may be considered Medium to long term travelers or overseas workers Those travellers at high risk of infection Those where diagnosis suggestive but investigations inconclusive Where required by authorities-refugees Even when on preventive measures! Occasionally preventive measures do fail Immunizations and chemoprophylactic agents and personal protective measures are not 100% protective Variable compliance with preventive advice Incorrect/insufficient advice/health intelligence Post-travel Consultation History Examination Investigations Screening History Are they symptomatic now or have been? Risk assessment - leading to specific history of possible exposures, e.g. schistosomiasis, zoonotic disease, sexual history, recently been diving, have they been bitten? Is there correspondence in relation to treatment abroad? Travel history can be important in terms of working out possible incubation period and differential diagnosis Screening History Prophylaxis and compliance - was the prophylaxis appropriate? Could it be a pre-existing condition? Could it be related to an occupational/recreational exposure? Screening Examination Post-travel physical examination for most short term travelers is usually unremarkable for disease, but may be useful for assessment of injuries Signs of “tropical” disease can be subtle and can be missed unless specifically looked for, e.g. rashes, eschar, jaundice Abnormalities unrelated to travel Look for the “spot” diagnosis Hookworms and cutaneous larva migrans: tracking lesions on the foot (or other body areas in contact with sand/soil) Look for the “spot”diagnosis Leishmaniasis: non-healing skin ulcers/lesions, especially on exposed areas and been to endemic areas Eschars-may be associated with rickettsial infectious such as scrub typhus Skin infection: bacterial and fungal (ask for occupational and recreational history) Others Screening Examination When sending specimens to lab, document current medications, history, what you think Liaise with lab if unsure what tests available Stool microscopy M/C/S, O/C/P-most diarrhoeal disease bacterial>>parasitic>viral Urine tests-dipstick urinalysis, “terminal” urine for ova of S. haematobium Full Blood Count and differentialeosinophilia, anaemia, thrombocytopenia Screening Examination Rapid tests, e.g. Immunochromographic tests (ICT)-often used for initial screening for malaria, Bancroftian filariasis, (dengue), etc Serological investigations, e.g. schistosomiasis, filariasis Blood films for malaria HIV/STI serology TB screening-useful if you can compare with pre-travel Does the traveler have diarrhea? Most travelers’ diarrhea is brief, self-limiting and non-inflammatory (about 4 days in duration) About 20% of travelers have fever and/or bloody diarrhea Enterotoxigenic Escherichia Coli is probably the most frequent pathogen in about 40-75 of cases Travelers’ diarrhea Inflammatory diarrhea may be caused by Campylobacter, Shigella or Salmonella infection Fever, cramping abdominal pain, pus and/or blood in the stool Quinolone antibiotics often employed (some resistance) Remember amoebic dysentery and giardiasis Travelers’ diarrhea Persistent diarrhea may be giardiasis, which may need treatment with tinidazole or metronidazole Chronic diarrhea may need further investigation and referral Does the traveler have fever? Possible serious infectious disease causes in travelers returning from tropical regions: – Malaria-great mimicker – Hepatitis A – Enteric fever (incl typhoid) – Dengue fever – Others Has the traveler been injured abroad? Need to document extent of injuries Are they covered by any insurance or superannuation policy? Arrange for any further treatment and follow-up Liaise with airlines if further travel required Arrange for assessment for rehabilitation as necessary Post-Travel Consultation It is important to elicit a history of travel. Many short term travelers will present with illness when they get back, following the incubation period. Investigation and management of some post-travel illnesses will be urgent because they are life threatening and/or a threat to public health.