* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Kidney Transplantation in Infants and Small Children, Blanche
Clostridium difficile infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hepatitis B wikipedia , lookup
Leptospirosis wikipedia , lookup
Hepatitis C wikipedia , lookup
Neonatal infection wikipedia , lookup
Oesophagostomum wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
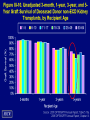
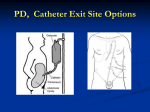
Kidney Transplantation in Infants and Small Children The Good, The Bad, and the Ugly Blanche Chavers, M.D. Professor of Pediatrics University of Minnesota Amplatz Children’s Hospital Disclosure Information Blanche Chavers, MD • I have no financial relationship to disclose • I will not discuss off label use and/or investigational use of drugs in my presentation How is ESRD Defined and How Common is it in US Children? • End stage renal disease - GFR < 15 mL/min/1.73 m2 • 1% of new US ESRD patients • 1.5% of prevalent US ESRD patients • On average, 7000 US children receive ESRD treatment each year Incident ESRD rates, by age figure 6.1, per million population, adjusted for gender & race (2001 USRDS ADR) 35.0 Rate Per Million Population 30.0 25.0 Ages 0-4 Ages 5-9 20.0 Ages 10-14 Ages 15-19 15.0 10.0 5.0 0.0 90 991 992 993 994 995 996 997 998 999 000 001 002 003 004 005 006 007 9 1 1 1 1 1 1 1 1 1 1 2 2 2 2 2 2 2 2 Incidence of Pediatric End-Stage Renal Disease by Race (per million age adjusted population per year, 2008 USRDS ADR) • Black 24 • Native American 19 • Asian/Pacific Islander 15 • White 13 Renal dysplasia/hypoplasia Prune-belly syndrome Intrauterine bladder outlet obstruction associated with • renal dysplasia • hypoplasia of abdominal musculature Posterior Urethral Valves FINNISH-TYPE CONGENITAL NEPHROTIC SYNDROME (NPHS1) Onset of proteinuria occurs in utero Massive proteinuria edema malnutrition hypothyroidism hypercoagulability infection With supportive care only: ESRD by 2-3 yrs, high morbidity/mortality from infection, thrombosis Excellent survival, QOL with BNx @ 4-6 mos, aggressive nutrition, transplant @ 8-10 kgs Etiology of Kidney Disease in 207 Infants 62 Hypoplasia 42 Obstructive Uropathy 26 Cong Nephrotic Synd 18 Oxalosis 11 Cortical Necrosis 10 Polycystic 9 Hemolytic Uremic S 8 Glomerulonephritis 6 Drash 4 Hypoxia at birth 3 Steroid res neph s Jeune's 2 Anatomic 2 4 Unknown 0 10 20 30 40 Number 50 60 70 Treatment Options for ESRD • Dialysis – Peritoneal – Hemodialysis • Kidney transplantation Special issues in 0-5 year olds Benefits of transplantation • Improved patient survival • Improved growth and development • Improved quality of life • Avoidance of dialysis complications Indications for Kidney Transplantation in Children • ESRD unresponsive to medical management • Progressive growth failure • Developmental delay • Progressive renal osteodystrophy • Failure to thrive Contraindications for Kidney Transplantation in Children • Active malignancy or less than 12 months post treatment for malignancy • Human immunodeficiency viral infection • Positive current T cell crossmatch • Nonadherence with medical management Timing of the Transplant • Optimal age for kidney transplant in the infant with ESRD remains controversial • University of Minnesota minimum requirements are 6 months of age and • 8 - 10 kg in body size Transplant Surgeon is key Transplant Nephrologist is key Pediatric Transplant Team • • • • • • • • • • • • • • Pediatric Nephrologist Surgeon Anesthesiologist Urologist Pediatric Intensivist Neurologist Psychiatrist / Psychologist Dialysis and Transplant Ward Nurses Transplant Nurse Coordinator Dietitian Social Worker Transplant Pharmacist Child Family Life Specialist Occupational/Physical and Speech Therapists Transplant the patient under the best possible conditions Optimize medical management pretransplant Optimize medical management pre transplant – Early referral and evaluation at transplant center – Screen for infections – Ensure up-to-date immunizations including influenza – Correct urological abnormalities pretransplant – Optimize dialysis treatment and encourage compliance with treatment regimen – Correct malnutrition, anemia, acidosis, renal osteodystrophy, growth failure Optimize medical management pre transplant – Correct hypercoagulable state – Pretransplant nephrectomy of native kidneys as indicated – Document patency of the aorta and inferior vena cava – Identify potential living donors or list for deceased donor transplantation – Screen for antileukocyte antibodies in potential deceased donor recipients – Provide psychosocial support to child and family Technically Challenging Special issues in 0-5 year olds: Risks -Graft thrombosis Very Big Kidney-->Infant & Small Child • Adult-sized kidney • Big Kidney: Hemodynamics – Blood flow – Blood pressure – Blood volume Note: The kidney will shrink to size and GROW with child Consequences of Hypovolemia Hypovolemia Acute tubular necrosis Graft thrombosis/infarction Hypotension Renal hypoperfusion Protecting intravascular volume following kidney transplantation • Vigorous volume-expansion prior to establishing circulation to transplant • Replace all urine output (cc for cc) for initial 48-72 hours • Maintain: CVP 8-12 BP 90th-95th% tile for age HR within normal range • “Third-space” fluid losses are common in first 24-72 hours after intraperitoneal transplant (bowel manipulation results in bowel wall edema) • Colloid (albumin) is often necessary to maintain adequate BP and CVP Adult kidney into small infant > 900 Pediatric Kidney Transplants Comparison of Pediatric Renal Txs 1984-2006 Age (yrs) <1 1-5 6-10 11-17 Total Nation 105 2618 2806 8589 14,118 U of MN 36 146 94 179 450 % U of MN 34 6 3 2 3 The Good Trends in Pediatric Kidney Transplantation 1996-2006 Impact of ESRD on Growth Younger subjects have greater height deficits at transplantation »0-1 years: -2.21 »2-5 years: -2.26 »6-12 years: -2.00 »13-17 years: -1.41 2008 NAPRTCS Annual Report Trends in Height Z Scores after Kidney Transplant 2004 NAPRTCS Annual Data Report The Good: Conclusions • Compared to chronic dialysis, kidney transplantation leads to improved patient survival • Children aged 0-5 years have the best long-term (5 year) graft survival rates of all kidney transplant recipients • Improvement in linear growth after transplant is associated with age < 6 years The Bad Infection Rates are Up in Young Pediatric Kidney Transplant Recipients Infectious hospitalization rates in pediatric vs. adult ESRD patients, by modality: any infection Figure 8.23, 2004 USRDS ADR Incident dialysis patients & first-time, kidney-only transplant patients, with Medicare as primary payor; unadjusted. Infectious hospitalizations represent inpatient claims with a principal diagnosis code for infection. Admissions per 100 patient years at risk Admissions for infection (overall), by age, gender, and time on ESRD: transplant 80 Age Gender 70 < 1 year 1 to < 2 years 2 to <5 years 5+ years 60 50 40 30 20 10 0 0-4 5-9 10-14 15-19 Male Female Figure 6.17, incident & prevalent transplant patients, 1997–1999 combined, 2001 USRDS ADR Cause-specific hospitalization rates in months 6-24 by selected characteristics at month 6 posttransplant (%) Viral Bacterial 0-1 years 27.1 25.3 2-5 years 24.5 23.0 6-12 years 14.6 13.3 > 12 years 10.0 11.6 Age at transplant Dharnidharka et al, AJT 4:384, 2004 Prevention of infection after transplant – Screening of donor and recipient for infections before transplant » CMV, EBV, HIV, Hepatitis A/B/C – Pretransplant serology – Ensuring up-to-date immunizations including influenza – Prophylaxis » Antiviral: ganciclovir, valganciclovir » Antibacterial » Antifungal The Bad: Conclusions Infection after kidney transplantation • Largest cause of death in pediatric first kidney transplant recipients -Infection 28.9% (NAPRTCS 2008 ADR) • The smallest children have the greatest number of infections after kidney transplantation • Immunizations help prevent vaccine preventable infection posttransplant • Co-infection is common The Ugly PTLD Rates are Unacceptable in Young Pediatric Kidney Transplant Recipients Posttransplant Lymphoproliferative Disorder (PTLD) • 4 -5 x more common in children after kidney transplant than adults • Usually caused by proliferation of Epstein Barr virus (EBV) infected B cells • Symptoms – Infectious mononucleosis – Lymphoid hyperplasia – Invasive malignant lymphoma QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Posttransplant lymphoproliferative disorders after renal transplantation in the United States in era of modern immunosuppression • Patient characteristics – Data obtained from the USRDS – 25,127 Medicare patients aged 1-98 years, transplanted between 1996 and 2000, 80% with grafts from deceased donors – 344 (1.4%) developed PTLD (non Hodgkin lymphoma) within the first 3 years of transplant. Mean time to onset was 12 months. 27% mortality – The incidence in pediatric patients (< 20 years) was 5.8% Caillard, et al Transplantation 80:1233, 2005 Posttransplant lymphoproliferative disorders after renal transplantation 3 Caillard, et al Transplantation 80:1233, 2005 Posttransplant lymphoproliferative disorders after renal transplantation Caillard, et al Transplantation 80:1233, 2005 Incidence of PTLD in Pediatric Renal Transplant Recipients Receiving Basiliximab, Calcineurin Inhibitor, Sirolimus and Steroids • 7% incidence in 274 recipients • Rate varied by age – 12% in 0-5 years – 7% in 6-10 years – 3% in 11-17 years – 0% in > 17 years McDonald, et al AJT 8:984, 2008 Malignancy Prevention in Pediatric Kidney Transplant Recipients • Pretransplant serology on donor and recipient • Viral load monitoring in high risk patients – EBV seronegative recipient – Children < 1 year at transplant – Children tested after receiving blood products that might transiently confer EBV positivity • Reduce immunosuppression if positive • Monitor uric acid, LDH, CT scans The Ugly: Conclusions Malignancy in Pediatric Kidney Transplant Recipients • Third largest cause of death in first kidney transplant recipients – Malignancy 10.6% • Highest rates are seen in the young • Mean 3-year posttransplant malignancy rates have increased – – – – 1987-1990 1.05% 1991-1994 1.4% 1995-1998 2.93% ≥ 1999 3.0% 2008 NAPRTCS ADR Conclusions: Pediatric Kidney Transplantation in Infants and Small Children • Young children have excellent long-term outcomes after kidney transplantation • Improvement in linear growth after transplant is associated with age < 6 years • Infectious complications of immunosuppression are highest in young children • Highest rates of PTLD are seen in young kidney transplant recipients age ≤ 5 years Acknowledgements Katherine Tabaka Jerry Vincent Jensina Ericksen