* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 6 - gu365 cases 2009..
Survey
Document related concepts
Transcript
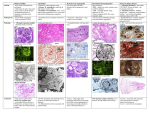
GUT CASE INVESTIGATION LECTURE 1 Nephrolithiasis(renal stones) Epidemiology Risk Factors Up to 10% by age 70, usu in 3rd to 4th decade 4:1 M to F ratio More prevalent in the South Hypercalcemic states, Crohn’s, stents, RTA, infection, gout, hypercalciuria, hyperuricosuria, cystinuria Symptoms Asymptomatic, flank pain, hematuria Composition OPAQUE contains calcium +/ phosphate Calcium calculi Ca oxalate, Ca phosphate Struvite calculi Magnesium ammonium phosphate= triple phosphate SEMI OPAQUE contains sulphur Cystine calculi LUCENT Uric acid stones;Xanthine Matrix (coagulated mucoid material) CT Imaging of Stones Essentially all renal and ureteral calculi have high attenuation on non-contrast CT (all but matrix stones have atten of > 100HU) CT has sensitivity of 97% and specificity of 96% Can also see hydronephrosis, hydroureter, renal enlargement, or perirenal stranding Must differentiate from phlebolith which is a calcified blood clot in a pelvic vein.(appearance: round/ovoid, smooth, central lucency, in true pelvis) Nephrolithiasis Radio opaque stone in calyx Images: BIDMC, Dept of Radiology, 2001. Hydronephrosis Dilated urine filled pelvis Stent Hydroureter Stent Images: BIDMC, Dept of Radiology, 2001. Obstructive Uropathy Radiologic Assessment Anatomy: Urinary Tract Renal Capsule Calyx Superior Operculum Cortex Medulla Papilla Pelvis Fornix Inferior Operculum http://www.urostonecenter.com/images/p1.gif Unequivocal Obstructive Uropathy = Urinary tract obstruction Unequivocal: clear etiology Obstruction may be at any site within GU tract Evidence of post-renal failure Variable presentation based on etiology Sign: Hydronephrosis = dilatation of renal pelvis and ureters Pathophysiology of Obstructive Uropathy Hydronephrosis Mechanical or functional obstruction Back up of urine flow = increased renal pressure Tubular dilatation Initial increase in renal blood flow Decrease in renal blood flow Increase in renal lymphatic flow Initial increase in ureteral peristalsis & pelvic muscle hypertrophy Muscle stretched & atonic Aperistalsis Dilatation of ureters and renal collecting duct system Parenchymal Atrophy Renal failure Pathogenesis of unilateral hydronephrosis. Smith’s Urology p.181 How Acute Obstruction leads to Dilatation and Decreased Tubular Function Pathology Dilated renal pelvis (arrow), external view http://www.smbs.buffalo.edu/pth600/IMCPath/y1case/y1ans21.htm#Obstructivelesionsintheurin arytract Dilated pelvis & calyces, renal atrophy, cut surface http://www.smbs.buffalo.edu/pth600/IMCPath/images/Year1/Hydronephrosis_Gross-_Robbins.jpg Clinical Presentation: Obstructive Uropathy Lower and Mid Tract (Urethra and Bladder) Hesitancy in starting urination Lessened force Weak stream Terminal dribbling Hematuria Burning on urination Cloudy urine (infection) Acute urinary retention Upper Tract (Ureter and Kidney) Flank pain radiating along ureter course (distension) Gross hematuria Nausea/Vomiting Fever/Chills Burning on urination Cloudy urine with infection Bilateral uremia N/V/weight loss Renal insufficiency Consider UTO in all patients with unexplained renal insufficiency Urine Output Changes Anuria = complete bilateral UTO Partial obstruction normal to elevated UO Hyperkalemic renal tubular acidosis Hypertension Lab Abnormalities: normal, microscopic/gross hematuria, pyuria, azotemia, uremia, anemia (2/2 chronic infection, ACD), leukocytosis Think Anatomically: Where is obstruction? Proximal etiology Series: 53 of 380 patients 52/53 in lower 1/3 of the ureter. Unilateral hydronephrosis Causes: Ureteral stones 64% Most Common in Distal Ureter Ureteral edema or lucent stones 30% Systemic or Neoplasms 4% Distal etiology Inflammatory disease 2% Chen et al., J Emerg Med, 1997: 15; 3. 339 – 343. Bilateral hydronephrosis Acute Obstruction and Anuria Acute complete, bilateral obstruction = Medical Emergency Patients may die from acute renal failure with oliguria/anuria Requires prompt recognition and possible surgical intervention CT examination: Postcontrast axial scan: The retroperitoneal giant tumor mass compresses the right ureter and causes hydronephrosis (arrows). http://www.szote.u-szeged.hu/radio/panc/alep8c.htm Diagnosis Early diagnosis and decompression is critical to prevent renal failure Continue to Radiologic work-up Ultrasonography Test of Choice for Suspected Urinary Tract Obstruction Screening test Indications: Renal failure of unknown origin/Hematuria/Signs of UTO/Urolithiasis Sensitivity for detection of chronic obstruction: 90% Sensitivity for detection of acute obstruction: 60% Advantages: No allergic/toxic complications of radiocontrast media Fast, inexpensive Diagnose other causes of renal disease in patient with renal insufficiency of unknown origin Polycystic Kidney Disease Disadvantages Nonspecific Rarely identifies cause False positive rate: < 25% with minimal criteria (operator dependent) Any visualization of collecting systems False negative with acute obstruction, dehydration, sepsis Bowel Gas decreases sensitivity Ultrasound – Normal Kidney Normal renal parenchyma, hypoechoic, normal function Normal renal fat, no dilatation of collecting system, hyperechoic Ultrasound – Obstructive Uropathy Renal parenchyma, hypoechoic Dilated collecting duct, hypoechoic (fluid) Compressed renal fat, hyperechoic CT: normal renal parenchyma with proximal stone, no obstructive uropathy Noncontrast CT Enhancing calculus in interpolar portion of R Kidney Kawashima et al., RadioGraphics 2004;24:S35-S54 CT: Hydronephrosis due to retroperitoneal fibrosis (soft tissue) CT (postcontrast): Giant retroperitoneal tumor mass compressing the right ureter, causing hydronephrosis with compression of renal parenchyma (arrows). http://www.szote.u-szeged.hu/radio/panc/alep8c.htm CT: Obstructive Uropathy Dilated Renal Pelvis Proximal Stone CT (postcontrast): Obstructive left-sided uropathy with proximal ureteric stone PACS, Courtesy of Dr. D. Brennan IVU: Intravenous Urogram Intravenous Pyelogram = Excretory Urogram 1. Scout film calculi? 2. IV bolus of radiocontrast dye (ionic contrast) 3. Series of plain films demonstrate kidneys, ureters, urinary bladder 4. Upright film post-void to evaluate for obstruction Advantages Anatomy Pathology Location Rough indicator of function bilaterally Low false positive rate Detects associated conditions Papillary necrosis intralumenal filling defect Caliceal blunting from previous infection Disadvantages Cumbersome Requires radiocontrast Need bowel prep with conventional IVU Radiation dose Need cross-sectional imaging follow up CT Urography Evaluate urinary tract for flow defects Noncontrast Scout first: Urolithiasis Coronal reconstructions: visualize entire urinary tract Advantages over Conventional IVU Speed Sensitive to renal parenchyma abnormalities Simultaneous evaluation of both renal parenchyma and urinary tract Cross-sectional imaging Disadvantages Radiation dose Ionic Contrast reactions/cannot be used in patients in renal failure Kawashima et al., RadioGraphics 2004;24:S35-S54 Normal CT Urogram CT Urography Total Body Opacificantion Nephrogram Pyelogram Normal CT Urogram CT Urography Total Body Opacificantion Nephrogram Pyelogram Normal CT Urogram CT Urography Total Body Opacificantion Nephrogram Pyelogram Normal CT Urogram CT Urography Total Body Opacificantion Nephrogram Pyelogram Normal CT Urogram CT Urography Total Body Opacificantion Nephrogram Pyelogram Pt. JL, PACS, Courtesy of Dr. AC Kim Normal CT Urogram CT Urography Total Body Opacificantion Nephrogram Pyelogram Normal CT Urogram CT Urography Total Body Opacificantion Nephrogram Pyelogram Contraindications for IVU/CTU History of allergy to IV contrast Bronchospasm, laryngeal edema, anaphylactic shock May use with history of minor allergic reactions with preprocedural steroids, antihistamines (diphenhydramine) 12 hours prior to study Renal insufficiency Pregnancy = relative contraindication (radiation exposure) MR Urogram can be used Likewise: children minimize radiation doses Pts taking oral hypoglycemics (metformin) should stop taking meds prior to study May resume after renal function is confirmed normal Risk of lactic acidosis Must be Physician-Supervised - Contrast reactions - Minimize no. of images - Minimize radiation - May use Fluoroscopy MR Urography Sagittal contrast-enhanced excretory MR urography obstructing right sided papillary TCC A. Unenhanced MR urography Heavily T2 weighted B. Gadolinium-enhanced excretory MR urography C. Excretory MR urography + diuretic 10 mg furosemide IV Gadopentetate dimeglumine Advantages: Distinguishes adjacent soft tissue abnormalities With Gadolinium: functional information No ionic contrast OK in renal failure No radiation children, pregnancy women Drawbacks High cost Low sensitivity in detecting calcifications Time intensive Metallic implants/Foreign Body = Contraindications Blandino et al., AJR 2002; 179: 1307 -1314 Excretory Urogram/CTU/MRU Acute Obstruction Mild Moderate Marked Kidney minimally enlarged Dense Nephrogram • Preferential absorption of Na and water from diseased tubules = concentration of contrast Delayed appearance of contrast in collecting system = delayed function Poor concentration of contrast in the collecting tubules No ureteral dilatation acutely Ureters not tortuous http://asia.elsevierhealth.com/home/sample/pdf/314.pdf Excretory Urogram/CTU/MRU Chronic Obstruction Partial Complete Progressive dilation of collecting system and ureters/tortuous Urectasis = dilated ureter Decrease number of nephrons 6-12 weeks: irreversible loss of renal function “Shell nephrogram” parenchymal atrophy Collecting system: blunt calyces/forniceal angles Calyceal Clubbing Blandino et al., AJR 2002; 179: 1307 -1314 Patient JL – Bladder Mass Left Bladder mass surrounding UO Diagnosis: 57 yo M with known Bladder CA with left hydronephrosis secondary to left bladder cancer. Management Foley placement for immediate decompression. Pt urinated following catheter removal and was cleared for d/c Urology consult for possible stent placement Renal Cystic Disease Very common 50% of pts over age of 50 Assoc w/ many syndromes, etiology unknown, probably arise from obstructed tubules or ducts Most commonly asymptomatic Rarely, may have hematuria, HTN, cyst infection, or mass effect CT Characteristics of Simple Cysts Smooth, imperceptible cyst wall Sharp demarcation from surrounding renal parenchyma Water attenuation (<15 HU), homogenous throughout lesion Non-enhancing Simple cysts are w/o septations or calcification May have slight elevation of adjacent renal parenchyma Beak sign Type I Simple Cyst Bird Beak Sign Aortic aneurysm Simple Cyst Images: BIDMC, Dept of Radiology, 2001. Inferior vena cava with filters Type IV Cystic Neoplasm Complex renal mass infiltrating lvc Images: BIDMC, Dept of Radiology, 2001. Conditions Associated with Multiple Cysts Autosomal Dominant PCKD Autosomal Recessive PCKD Acquired Cystic Disease (hemodialysis pts) Von-Hippel-Lindau disease Tuberous Sclerosis Medullary Sponge Kidney Benign Masses Cysts Angiomyolipoma Oncocytoma (via epithelial cells of prox tubule) Renal Adenoma Mesoblastic Nephroma (hamartomatous tumor, usu present at birth) Hemangioma Various Renal Pelvic Tumors(papilloma, angioma, fibroma) Hematoma Angiomyolipoma Hamartomas containing fat, smooth muscle, and blood vessels Usually asymptomatic, but may spontaneously bleed Large AMLs resected or embolized Multiple AMLS usually Associated w/ tuberous sclerosis On CT *fat attenuation in mass*, strong contrast enhancement (RCCs rarely contain fat), no Ca2+ Angiomyolipoma Note fat content Images: BIDMC, Dept of Radiology, 2001. Malignant Masses Renal Cell Cancer Transitional Cell Cancer Wilm’s Tumor Nephroblastomatosis (multiple rests of embryologic metanephric blastoma) Lymphoma Metastases (lung, breast, colon, melanoma) Renal Cell Ca Most common primary renal malignancy (85% of primary renal tumors) Assoc w/ smoking, family hx, age, Von HippelLindau, Acquired Cystic Disease/chronic dialysis, phenacetin abuse Presentation: Hematuria, flank pain, wt loss, palp mass, fever, anemia, paraneoplastic syndromes liver enzymes w/o mets Stauffer syndrome CT characteristics Variablefrom complex cyst to large, heterogeneous renal mass Generally enhancing May have calcifications May have hemorrhage and central necrosis Usually no fat Renal Cell Ca Images: BIDMC, Dept of Radiology, 2001. RCC Images: BIDMC, Dept of Radiology, 2001. Renal Trauma Anatomy of the Kidney Renal blood supply IVC Ureter Renal arteries Renal veins Be suspicious of renal injury with broken ribs 2 Anatomy of the Kidney 3 Prevalence of Renal Trauma • 10-20% of trauma pts. have GU involvement • 45% of GU trauma is renal • 20-30% of renal trauma pts. have associated abdominal injury 4 Mechanisms of Renal Trauma • Blunt trauma (80%): MVA, falls, assaults • Penetrating trauma (20%): gunshot, stabbing, impalement • Predisposing factors: preexisting renal conditions (tumors, hydronephrosis), children, associated abdominal injuries 5 Clinical Presentation of Renal Trauma • Gross or microscopic hematuria (absent in 5%) • Flank pain/ecchymosis • Hemodynamic instability • Presence of other abdominal injuries 6 Patient 1: An illustration of imaging modalities • 18 yo male sustained stab wound to R flank • P=180, BP 130/80, Hct 36 • CXR nl. • Why image and with which modality? 7 Indications for Imaging • Gross hematuria • Microscopic hematuria with hemodynamic instability • Persistent microscopic hematuria • Significant MOI 8 Radiologic Imaging of Renal Trauma CT with IV contrast • Gold standard, high sensitivity • Immediate and delayed post-contrast images to view collecting system • Allows diagnosis and staging • Images abdomen and retroperitoneum • Not for hemodynamically unstable pts. 9 Patient 1: CT with IV contrast Normal attenuating kidney Peri-renal hemorrhage 10 Patient 1: CT with IV contrast Contrast extravasation 11 Patient 1: CT with IV contrast Renal laceration with extravasation of contrast Retroperitoneal hematoma 12 Radiologic Imaging of Renal Trauma Cont. Intravenous pyelography • Unable to evaluate abdomen and retroperitoneum • Inadequate for grading renal injury Image from Trauma.org • Used in unstable pts prior to surgery to identify functioning contralateral kidney Extravasation of contrast from R kidney 13 Radiologic Imaging of Renal Trauma Cont. Renal Angiography • Delineates vascular injury (intimal tears, pseudoaneurysm, AV fistula) • Use when CT equivocal and continued hemorrhage • Use for endovascular repair (embolization, stenting) Image fromTrauma.org Devascularization of L kidney 14 Radiologic Imaging of Renal Trauma Cont. Renal ultrasound • Bedside US in ED allows evaluation of abd/pelvic injury/fluid accumulation Subcapsular hematoma • High false neg. rate for renal injury • Used in areas without CT, or for follow up kidney 15 Patient 2: An Illustration of Injury Staging • 17 yo unrestrained driver MVA c/o RLQ pain • VSS • Hct 45.7, BUN 15, Cr 1.2 • CXR, cervical, lumbar, pelvic plain films nl. • CT demonstrates renal laceration • How severe? How manage? 16 AAST Organ Injury Scale - Renal Injury Grade I Contusion: Microscopic or gross hematuria, urological studies normal Hematoma: Subcapsular, nonexpanding without parenchymal laceration Grade II Hematoma: Nonexpanding perirenal hematoma confined to renal retroperitoneum Laceration: <1cm parenchymal depth of renal cortex without urinary extravasation Grade I and II injuries managed conservatively (observation, serial Hct) 17 AAST Renal Injury Scale Cont. Grade III Laceration: >1cm depth of renal cortex, without collecting system rupture or urinary extravasation Grade IV Laceration: Parenchymal laceration extending through the renal cortex, medulla and collecting system Vascular: Main renal artery or vein injury with contained hemorrhage Grade III and IV injuries are now managed conservatively 18 AAST Renal Injury Scale Cont. Grade V Laceration: Completely shattered kidney Vascular: Avulsion of renal hilum which devascularizes kidney Image from www.trauma.org Surgery! Salvage vs. nephrectomy 19 Renal Trauma Conclusions • Look for renal trauma in pts with abdominal trauma and significant MOI • CT with contrast • Grade severity of injury • Injuries requiring surgery: vascular injury, shattered kidney, expanding hematoma • 80-90% renal injuries treated conservatively with • remarkable resolution! 23 Imaging in the Evaluation of Female Infertility Infertility Inability to conceive after one year of intercourse without contraception Epidemiology Affects 1 in 7 American couples Rate has been stable over the past 50 years Advances in assisted reproductive technologies (ART) has increased interest in infertility treatment Infertility - Causes Male Factor – 40% Azoospermia Sperm defect or dysfunction Chronic Illness Combined Factors – 10% Female Factor – 40% Advanced age Anovulatory cycles Congenital anomalies Acquired structural defects Endocrine abnormalities Unexplained – 10% Infertility – Radiologic Evaluation Largely focuses on female factor infertility Several congenital and acquired conditions affect female reproductive function Complete evaluation of the female reproductive tract must include cervical, uterine, endometrial, tubal, peritoneal, and ovarian factors Menu of Tests Hysterosalpingogram (HSG) Ultrasound (US) Sonohysterogram (SHG) Magnetic Resonance Imaging (MRI) HSG Hysterosalpingogram Historically the mainstay in infertility imaging Indications: evaluation of uterine cavity and patency of tubes Limitations: does not aid in characterization of uterine wall or ovarian pathology Ultrasound Test of choice for imaging the female pelvis No radiation exposure Indications: evaluation of ovarian, uterine wall, and adnexal pathology Limitations: additional imaging may be needed for pre-surgical characterization and localization of pathology MRI Excellent soft tissue characterization Indications: guides interventional radiology and surgical management of infertility by identifying size, number, and location of pathology Female Reproductive Tract www.ethal.org.my/.../ 181rmgUterus.html Cervix Cervical Stenosis Fallopian Tube vary Narrowing of the cervix due to adhesions or scarring Patients complain of painful or absent periods Complication of cone biopsy Blocks entry of sperm Ovary Uterus Adhesions Cervix Vagina www.drkline.com/ risks.html Cervical Stenosis HSG Findings: •Internal os < 1mm •Inability to advance catheter Normal HSG •Non-opacified uterine cavity Vagina Cervical Stenosis BIDMC, PACS Uterus Synechiae Fibroids Polyps Congenital Anomalies Synechiae Asherman Syndrome Intrauterine adhesions caused by trauma, infection, or instrumentation Healing granulation tissue forms bridges across the cavity Infertility may result from obliteration of the cavity or obstruction to implantation Synechia HSG findings: Filling Defect Linear Irregular Synechia BIDMC, PACS Synechia US Findings: Echoic Linear Extends from one wall to opposite wall Synechia Fibroids Benign, smooth muscle tumors of the uterus Found in 20-30% of reproductive aged women Affects fertility by interfering with implantation Fibroids HSG Findings Scalloped endometrial lining Fibroids Ultrasound aids in characterization of fibroids. US Findings: Hypoechoic mass May be submucosal, intramural, or subserosal Uterine enlargement or distortion may be seen 12 Fibroid Fibroids MRI aids in: • characterization and localization of uterine wall pathology •pre-surgical planning Fibroids BIDMC, PACS Uterine Anomalies A defect in the embryologic development of the Mullerian system can cause congenital uterine anomalies There are 7 classifications of anomalies All can be identified by imaging Uterine Anomalies Class II - Unicornuate Normal Class III - Didelphys Class V - Septate Class IV - Bicornuate Class VI - Arcuate http://www.emedicine.com/radio/topic738.htm Class VII - DES Uterine Anomalies Two classes must be differentiated in the infertility work-up: Bicornuate: Septate: • Indented fundus but otherwise normal uterine wall • No affect on fertility • No infertility treatment necessary • Fibrous band projecting from fundus into uterine cavity • Interferes with implantation • Surgical removal increases fertility http://www.emedicine.com/radio/topic738.htm Uterine Anomalies Irregularly shaped uterine cavity on HSG MRI BIDMC, PACS Uterine Anomalies The irregularly shaped uterus seen on HSG and MRI in the previous slides was determined to be an arcuate (class VI) uterus. It is on the spectrum of bicornuate and is believed to be a normal variant with no affects on fertility. Fallopian Tubes Obstruction Pelvic Inflammatory Disease Fibroids Endometriosis Adhesions Tubal spasm Fallopian Tubes Isthmus Ampulla Infundibula Fimbria Fallopian Tubes Left Proximal Obstruction Right Proximal Obstruction Peritoneal Cavity Adhesion Endometriosis Post surgical Post infection Difficult to image directly but an irregular pattern of dye overflow on HSG may raise suspicion. Ovaries Endometriosis Polycystic Ovary Syndrome (PCOS) Endometriosis C6 US Findings: •Round Bilateral Endometriomas •Symmetric •Hypoechoic cysts •Low-level echoes Ovarian stroma •Persistent PCOS US Findings of PCO: Bilateral Round, echogenic ovaries 10-12 small follicles PCOS is a clinical diagnosis. US findings of polycystic ovaries is neither necessary nor sufficient, but in the right clinical setting may be indicative of the diagnosis. EW is 9 weeks pregnant today. Early OB Ultrasound at 7 weeks 4 days.