* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Cardiovascular System
Survey
Document related concepts
Transcript
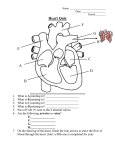
The Cardiovascular System Lindsey Bily Anatomy & Physiology Austin High School What is Blood? It is the delivery service for the body. Picks up food and oxygen from the respiratory and digestive system and delivers them to the cells. Picks up wastes from the cells and takes them to the excretory organs. Transports hormones, enzymes, buffers, and other substances vital to life. Heat regulating mechanism. It can absorb lots of heat without raising the fluid temperature. What is Blood? 8% of a person’s body weight is blood Male- 5-6 L, female- 4-5 L When you donate blood, they generally take 1 L from you. That is about 10% of your total blood volume. What is Blood? Composed of… Red blood cells (RBCs)- erythrocytes White blood cells (WBCs)- leukocytes Platelets- thrombocytes Plasma is the fluid portion and is mostly water A B A: red blood cells B. Blood smear with all components C. Platelets D. White blood cells C D Red Blood Cells Do not have ribosomes, mitochondria, or many other organelles. Contain lots of hemoglobin. That’s why they are red. They can change shape to fit through tiny blood capillaries. Testosterone may stimulate RBC production-males typically have more RBCs than women. (5,500,000 vs. 4,800,000 per/mm3 Red Blood Cells Transport oxygen and carbon dioxide. The total surface area of all the RBCs in an adult is equal to an area larger than a football field for exchanging gases! Each hemoglobin molecule can carry 4 oxygen or carbon dioxide molecules. Anemia: having a hemoglobin content of less than 10g per 100/mL of blood (normal~ 12-16 g per 100/mL) Red Blood Cells Erythropoiesis: RBC formation Occurs in the red bone marrow and the process takes about 4 days. Each minute of our life, we replace 200 billion RBCs that have been destroyed! If the blood oxygen level decreases (higher altitudes) we make more RBCs. The life span is 105-120 days. They usually break apart in the capillaries as they age. Macrophages lining the blood vessels phagocytose them. Sickle Cell Anemia Due to an abnormal type of hemoglobin. Causes the RBC to change shape and get stuck in capillaries. Inherit the gene from 1 parent and you have a less severe form called “sickle cell trait”. Inherit from both parents and you have a more severe case. Causes strokes, swelling, ulcers, etc. due to blockage in the blood vessels. Sickle Cell Anemia Spleen with sickle cell anemia White Blood Cells • • There are 5 types of WBCs that each have a different form of protection for the body. Some destroy bacteria, parasitic worms, ingesting inflammatory chemicals, contain histamine, eat viral infected cells and cancer cells. WBCs are formed in red bone marrow and in lymphatic tissue. White Blood Cells Platelets They stick together to form plugs or clots to stop blood flow. Usually form at the site of injury. We are always having microhemorrhages in our capillaries. Without platelets we could bleed to death. Formed in the red bone marrow, lungs, and spleen and “live” about 7 days. Platelets Blood Types Blood type refers to the antigens that are attached to the RBC membrane. (A, B or Rh) Type A: A antigens on the RBC Type B: B antigens on the RBC Type AB: both A & B on the RBC (universal recipient) Type O: neither antigens (universal donor) Blood plasma contains antibodies that are different from the antigens on the RBCs so that you don’t attack your own RBCs. Blood Types Blood Types The Rh System Rh + blood has the Rh antigen on the RBC. Rhdoesn’t. Plasma does not have antibodies against Rh naturally. Only if a (-) person has been in contact with Rh (+) blood may they make the antibodies. Sometimes a mother could be Rh- and her baby is Rh+. During delivery, the blood mixes, and the mom develops the antibodies. The first baby is born fine, but if the mother has another Rh+ baby in the future, the baby is at risk of dying. Plasma Liquid part of the blood. contains… 90 % water 10% solutes Proteins that regulate blood clotting and help with immunity Glucose, amino acids, lipids Urea, uric acid, creatinine and lactic acid Oxygen and carbon dioxide Hormones and enzymes Blood Clotting (Coagulation) We need our blood to clot to stop bleeding and prevent loss of body fluid. Clotting is a series of chemical reactions that happen really fast that causes a net of fibers to be built which traps RBCs. Blood Clotting Proteins involved… Prothrombin Thrombin Fibrinogen Fibrin Blood Clotting You need calcium in order for some of the chemical reactions to occur. If you have a low blood calcium level, you may have trouble clotting. The pale yellowish liquid left over after the clot has formed is blood serum. It is the blood, minus the blood cells and clotting elements. You need Vitamin K for the liver to make the clotting proteins. You get this from foods (broccoli, cabbage, asparagus, okra, beans, etc..) and also bacteria in your gut make it. Opposing Clotting We only want our blood to clot under certain conditions. Normal blood vessels are very smooth, so platelets can’t attach. That makes sure clotting is not activated. Heparin is an anti-thrombin in blood that keeps it from clotting. Promoting Clotting A rough spot in the blood vessel lining will cause clotting as will an abnormally slow blood flow. Atherosclerosis causes rough spots due to the cholesterol-lipid plaques that have built up. People who are immobile can get clots (thrombosis) since blood flow decreases. Once started, a clot continues to grow unless medicine is taken to stop it. Blood Disorders Most blood disorders are due to the tissues not forming blood cells properly. If a blood disorder is suspected, bone marrow is taken from the pelvis and tested. A bone marrow transplant may be required. RBC Disorders Anemia: inability to carry sufficient oxygen to the body’s cells. Polycythemia: too many RBCs and it becomes too thick to flow properly. Aplastic anemia: too few RBCs. Causes by destruction of bone marrow by drugs, toxic chemicals, radiation, or cancer. Pernicious anemia: low # of RBCs. Deficiency of Vitamin B12. Usually due to a problem with the stomach that doesn’t allow you to absorb it. Folate-deficiency anemia: low # of RBCs due to a deficiency in folic acid (Vitamin B9). Common in alcoholics and other malnourished individuals. Hemoglobin Problems Iron-deficiency anemia: too little iron means that you can’t make hemoglobin. Sickle Cell Anemia Thalassemia: Similar to sickle cell anemia. Abnormal hemoglobin causes changes in RBC shape. WBC Disorders Leukopenia: too few WBCs (HIV/AIDS). Leukocytosis: too many WBCs (usually caused by bacterial infection). Leukemia: a group of malignant disorders where adult stem cells replace normal cells. They can eventually leave the bone marrow and travel to other parts of the body. Clotting Disorders Thrombus: clot that stays in the place where it was formed. The condition is called thrombosis. Embolus: When the clot dislodges and circulates through the bloodstream. Called an embolism. Drugs that can prevent clotting are Heparin (prevents prothrombin from turning into thrombin) and Coumadin (prevents Vitamin K from stimulating the liver to produce clotting proteins). Clotting Disorders Hemophilia: X-linked disorder and affects 1 in 10,000 males. Failure to produce 1 or more of the clotting proteins. Thrombocytopenia: low levels of platelets. Caused by destruction of bone marrow due to drugs, immune system diseases, chemicals, radiation or cancer. Bleeding from many small blood vessels in the body. The Heart 4 chambered pump the size of a fist. Weighs 310g (males) and 225g (female) Heart Coverings Pericardium-sac that surrounds the heart. Contains pericardial fluid that protects the heart from friction while pumping. Myocardium- the bulk of the heart wall made up of cardiac muscle . Endocardium- inner layer of the heart. Very delicate layer. Chambers of the Heart 4 Chambers 2 upper: right and left atria They receive the blood from the body 2 lower: right and left ventricles They receive blood from the atria and pump it out to the lungs and the rest of the body Valves of the Heart The valves permit blood flow in one direction only. 2 Atrioventricular Valves: Also called “cuspid” valves Right AV Valve (tricuspid)-right atrium to right ventricle Left AV Valve (bicuspid)-left atrium to left ventricle 2 Semilunar Valves Pulmonary Semilunar valve: right ventricle to pulmonary artery Aortic Semilunar Valve: left ventricle to aorta Valves of the Heart Blood Flow Blood Supply to Heart Tissue The heart muscle cells (myocardium) receive blood via the coronary arteries that branch off of the aorta. The left ventricle cells receive the most blood because it does the most work. The atria receive blood from a small branch off the coronary arteries. The right coronary artery is dominant in about 50% of all hearts, left 20% and in 30% neither is dominant. Blood Supply to the Heart There are few connections between the coronary arteries. If the main route is blocked, there are few detours. Myocardial Infarction (MI): Death of oxygen deprived heart muscle cells. This is a heart attack. Blood Supply of the Heart Cardiac Veins surround the heart and once blood has supplied the cells with oxygen, they enter the vein and go back to the right atrium. Heart Conduction System Sinoatrial Node (SA node): “pacemaker” of the heart. Sets up the action potential and causes atria to contract. Atrioventricular Node (AV Node): small mass of special cardiac muscle tissue that lies at the lower part of the right atrium. Atrioventricular Bundle (AV Bundle): Action potential passes to the ventricles and then down the Purkinje Fibers to cause the ventricles to contract. Heart Conduction Blood Vessels Carry blood to and from the heart. Arteries-carry blood away from the heart. All arteries EXCEPT the pulmonary artery carry oxygenated blood. Veins-carry blood to the heart. All veins EXCEPT the pulmonary vein carry deoxygenated blood. Blood Circulation Blood leaves the heart Arteriesarteriolescapillariesvenulesveins back to the heart Functions of the Blood Vessels Capillaries: microcirculation to every cell Arteries: “distributors”. Arterioles regulate blood pressure by acting as resistance vessels for the capillaries. Veins: “collectors and reservoir vessels”. They can stretch called capacitance. Major Blood Vessels Aorta: serves as the main trunk of the entire systemic arterial system. Blood Vessels The main arteries and veins lie deep in the body alongside bone- deep veins and arteries Superficial veins and arteries are the ones that are closer to the skin and you can see. Hepatic Portal System Veins from the spleen, stomach, pancreas, gallbladder and intestines send their blood to the liver for filtering via the Hepatic Portal Vein. Purpose: Liver removes excess glucose from the digestive system blood after a meal. Liver puts glucose back into the blood when levels are low. Toxic molecules such as alcohol are partially removed or detoxified before blood goes to the rest of the body. Hepatic portal circulation. In this unusual circulatory route, a vein is located between two capillary beds. The hepatic portal vein collects blood from capillaries in visceral structures located in the abdomen and empties it into the liver. Hepatic veins return blood to the inferior vena cava. (Organs are not drawn to scale.) Fetal Circulation Fetal blood gets oxygen and food from the mom’s blood as opposed to its own lungs and digestive organs. Fetuses have additional blood vessels to do this. Umbilical arteries (2) Umbilical vein Ductus Venosus Fetal Circulation Umbilical arteries: carry fetal blood to the placenta. Placenta: Attached to the uterine wall and exchanges oxygen and nutrients between the mom and baby. No mixing of the blood! Umbilical vein: returns oxygenated blood from the placenta to the baby. Ductus Venosus: blood from the umbilical vein goes here and bypasses the liver. Foramen ovale: opening in the septum between the right and left atria so that blood bypasses the fetal lungs. Ductus arteriosus: Connects the pulmonary artery to the descending aortic tract. Another way to bypass the lungs. Fetal Circulation: Most fetal blood is a mixture of oxy and deoxy blood so it is shown as purple. Changes After Birth Once the umbilical cord is cut, none of the fetal structures are needed. The placenta is shed with the mother’s afterbirth. The blood vessels become fibrous cords in the liver. The foramen ovale begins to close once the baby takes its first breath and takes 9 months to fully close. Disorders Pericarditis: inflamed pericardium. Caused by trauma, virus, bacteria, tumor and causes severe chest pain because the layers rub together every time the heart beats. Pus, pericardial fluid, or blood can accumulate interfering with the heart to pump and begins to compress it called cardiac tamponade. Disorders Stenosed valves: valves that are narrower than normal so they slow blood flow from the chamber. Rheumatic heart disease: caused by a delayed inflammatory response to a Strep infection. Occurs mostly in children. The valves become inflamed and can result in permanent damage in the valve, the myocardium, or chordae tendinae (heart strings). Disorders Mitral Valve Prolapse: The mitral (bicuspid) valve’s flaps extend back up into the left atrium. You get backflow of blood or leaking of the valve. Most people don’t develop any symptoms, but some have chest pain and fatigue. Aortic regurgitation: Leaky aortic semilunar valve. Blood flows back from the aorta to the left ventricle. You have too much blood in the left ventricle now, so it gets bigger to compensate as well as increases its contraction strength. This can stress the heart and cause some cells to die. Mitral Valve Prolapse (above) Aortic Regurgitation (right) Disorders Coronary Artery Disease (CAD): a condition where blood flow to the heart is reduced. Can be caused by… Coronary embolism or thrombus blocking blood flow. Atherosclerosis: “hardening of the arteries” due to lipids building up on the sides. Disorders Angina pectoris: severe chest pain that is felt when the coronary artery is not delivering enough blood to the heart. Coronary Bypass Surgery: Veins are harvested from other parts of the body to create “detours” to bypass the clogged coronary arteries. Disorders Congestive Heart Failure: Inability of the left ventricle to pump blood well. Usually due to myocardial infarction (MI) caused by CAD. Causes the body to retain fluids. Pulmonary edema: fluid buildup around the lungs Patients may be candidates for a heart transplant or heart implant. Heart transplants are not very successful because the body’s immune system tends to reject the new heart. Heart implants are machines that don’t have any external pumps. External battery packs recharge the small internal battery. Disorders Arteriosclerosis: “hardening of the arteries” by calcium deposits which reduces blood flow to tissues. The tissues may die (necrosis) and gangrene may develop. Develops with advanced age, diabetes, high blood pressure, and smoking. Angioplasty: procedure to open up the narrowed arteries. A balloon can be inserted and inflated opening up the artery. Disorders Aneurysm: section of an artery has become abnormally wide due to weakening of the arterial wall. Promotes the formation of a thrombus. The artery can burst and cause internal bleeding Disorders Varicose veins: enlarged veins where blood tends to pool. The valves in the veins then get leaky and have a hard time getting blood back to the heart. Disorders Hemorrhoids: varicose veins in the anal canal. Caused by excessive straining during defecation. Hemodynamics How we achieve blood flow and vary the volume and distribution of the blood circulated. Active cells-more blood Inactive cells-less blood Conduction Remember the 4 structures… Sinoatrial node (SA node): The Pacemaker Atrioventricular node (AV node) Atrioventricular Bundle (AV Bundle or Bundle of His) Purkinje fibers (Bundle branches) These structures are specialized cardiac cells that don’t contract. They are there to propagate action potentials through the heart. Conduction The SA node’s normal intrinsic heart rate is 70-75 beats per minute (bpm) at rest. If the SA node cannot create an impulse, one of the other structures will assume the duty. However, they beat more slowly at 40-60 bpm Electrocardiogram (ECG or EKG) The impulses created in the heart cause tiny electrical currents to spread to the surface of the body. We can take a graphic record of the heart’s electrical activity with an electrocardiogram. ECG Waves Composed of the P wave, QRS complex, and T wave P wave: The depolarization of the atria (becoming more -). Showing the impulse traveling from the SA node through the atria. QRS complex: ventricular depolarization and atrial repolarization T wave: repolarization of the ventricles Cardiac Dysrhythmia Dysrhythmia: abnormal heart rhythm. AV Node Heart block: impulses can’t get to the ventricles. The ventricles contract much slower than normal. Usually a pacemaker is needed. Bradycardia Slow heart beat– below 60 bpm. We reach bradycardia during sleep and athletes can reach it while awake, but resting. Other than that, you could have a damaged SA node or there may be abnormal autonomic control. Tachycardia Very rapid heart beat– more than 100 bpm Normal during and after exercise and during stress response. Abnormal tachycardia is due to improper autonomic control, blood loss or shock, drugs and toxins, and fever. Fibrillation-cardiac cells contract out of step with each other. Atrial fibrillation: Abnormal atrial contraction and so it does not pump blood well. Can be controlled by drugs. Ventricular fibrillation is deadly because the ventricles stop pumping blood to organs. Defibrillation: application of an electric shock to force the fibers to contract together. Atrial fibrillation Ventricular fibrillation Cardiac Cycle A complete heartbeat is 1 cardiac cycle. 1. 2. 3. 4. 5. Contraction: systole Relaxation: diastole Atrial systole: contraction of the atria (P wave) Isovolumetric Ventricular Contraction: The ventricles fill with the same volume of blood and then they contract Ejection: semilunar valves open and blood is ejected from the heart. There is always a volume of residual blood left in the ventricles after this. Isovolumetric Ventricular Relaxation: the semilunar valves close and the AV valves open. Passive Ventricular Filling: AV valves open and ventricles fill Heart Sounds “Lub dub” Lub: contraction of the ventricles and closing of AV valves Dub: closing of the semilunar valves If you have a heart murmur, the heart sounds differently and you could have incomplete closing of the valves or stenosis of the valves. Factors that Affect Heart Rate Parasympathetic nervous system releases Acetylcholine to inhibit the heart beat through the vagus nerve. Sympathetic nervous system releases Norepinephrine to stimulate the heart beat through the cardiac nerve. There are pressure receptors (baroreceptors) located in the aorta and carotid arteries that detect changes in blood pressure, and adjust the heart rate to get it back to normal. Factors that Affect Heart Rate Emotions: Anxiety, fear and anger: increase heart rate Grief and depression: decrease heart rate Exercise: you release epinephrine and that stimulates the heart High blood temp and stimulation of skin heat receptors- fast heart rate Low blood temp and stimulation of skin cold receptors- slow heart rate Pain: sudden intense pain from the visceral organs slow the heart rate and can cause fainting. Blood Pressure Measured with a sphygmomanometer and is measured in mmHg. The cuff is wrapped around the brachial artery in the upper arm. The air is pumped into the cuff until it compresses the artery and no pulse can be heard through a stethoscope. Air is then released until the artery opens up a little and you hear a tapping sound. This is the systolic pressure (ventricles contracting) The tapping sound changes to very muffled sounds until they disappear and this is the diastolic pressure (ventricles relaxing) Blood Pressure Normal adult BP is 120mmHg systolic and 80mmHg diastolic (120 over 80 or 120/80). Pulse Pulse is the expansion and then recoil of the arteries as blood is pumped. You can feel your pulse several places in the body. Radial artery-wrist Temporal artery- temples Facial artery-jawbone Popliteal artery- behind the knee Posterior tibial artery- inner ankle bone Dorsalis pedis artery- upper surface of the foot Pressure Points There are 6 points where you can stop arterial bleeding. Temporal artery Facial artery Common carotid artery Subclavian artery Brachial artery Femoral artery Disorders Hypertension (HTN): high blood pressure (over 140/90 mmHg) 90% of patients have an unknown cause 10% of patients have HTN due to kidney disease, hormonal problems, or birth control pills, or pregnancy. Genetics play a large role. Seen in males more than females and in older people. Risk factors: high stress, smoking, obesity, high alcohol and caffeine intake, and lack of exercise. Disorders HTN is usually a “silent killer” because it doesn’t have any major symptoms. Heart disease Heart failure Kidney failure stroke Heart Failure Inability of the heart to pump enough blood to sustain life. Due to… Congestive heart failure (left ventricle failure) Cardiomyopathy (disease of the myocardium) Valve disorders Shock Failure of the circulatory system to deliver enough oxygen to cells. Cardiogenic: due to heart failure Hypovolemic: loss of blood volume in the vessels (blood loss, burns, chronic diarrhea or vomiting, dehydration) Neurogenic: dilation of the blood vessels, so blood pressure gets too low. The parasympathetic nervous system does not balance out the sympathetic. Anaphylactic: allergic reaction that causes blood vessels to dilate Septic: toxins in the blood dilate the blood vessels.