* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download neuropath-for-psy-d-disorders
Survey
Document related concepts
Transcript
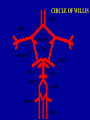
GCS 1. Best eye response - (max 4) 2. Best verbal response - (max 5) 3. Best motor response - (max 6) GCS- 13+ mild H I 9-12- moderate H I 8 or less – severe H I HI • May result in LOC • Longer unconscious and deeper coma > likelihood that pt has suffered severe HI • 60% good recovery • Based on US, UK and Netherland figures for every 100 HI, 5 VS, 15 severely disabled, 20 minor problems, 60 full recovery Nature of lesions in HI • Non - missile- RTA • Missile Distribution of lesions • Focal • Diffuse Primary damage TIME COURSE • scalp laceration • skull fracture • cerebral contusions • ICH • DAI Immediate Delayed Secondary damage • • • • ischemia hypoxia cerebral oedema infection Pattern of damage in non -missile HI Focal Scalp- contusion, laceration Skull - fracture Meninges - haemorrhage, infection Brain - contusions, laceration, infection Diffuse damage Brain, DAI, DVI, HIE, Cerebral oedema ICH is a complication of 66% of cases of nonmissile head injury Haemorrhage May be EXTRADURAL INTRADURAL - subdural, subarachnoid intracerebral EDH • Found in 2% HI • Usually associated with skull fracture • Arterial bleed usually meningeal vessels Subdural haemorrhage • Usually venous • Rupture of bridging veins Subdural haematoma: classification 48-72 hours – acute composed of clotted blood 3-20 dys – subacute – mixture of clotted and fluid blood 3 weeks + - chronic encapsulated haematoma Traumatic SAH • may result from severe contusions • Fracture of skull can rupture vessels • IVH may enter SAS • RULE OUT ANEURYSM Cerebral contusions • Superficial bruises of the brain • Frequent but not inevitable after head injury Various types of surface contusions and lacerations ~ Coup – at point of impact ~ Contrecoup- diametrically opposite point of impact ~ Herniation – at point of impact between hernia ~ Fracture related to # of skull Sites of cerebral contusions • Frontal poles • Orbital surfaces of the frontal poles • Temporal poles • lateral and inferior surfaces of occipital poles • cortex adjacent to sylvian fissure Uncommon types of focal brain damage • Ischaemic brain damage due to traumatic dissection and thrombosis of vertebral or carotid arteries by hyperextension of the neck • Infarction of pituitary - due to transection of pituitary stalk • pontomedullary rent Infection • complication of skull fracture • Open HI • Incidence is increased even after closed HI as devitalised tissue prone to infection Diffuse damage • DAI - widespread damage to axons in the CNS due to acceleration/deceleration of the head • Pts usually unconscious from moment of impact • Lesser degrees compatible with recovey of consciousness Brain swelling and raised ICP Results from: • cerebral vasodilation - inc cerebral blood vol • damage to BV - escape of fluid through BBB • inc water content of neurones and glia- cytotoxic cerebral oedema ICH herniation Subfalcine herniation Tentorial herniation Tonsillar herniation End result of herniation is compression and Duret haemorrhages as seen in the pons The pathologist and CNS neoplasms Clinical details of importance ~ ~ ~ ~ Age Sex F/X Site of neoplasm INCIDENCE; ~ Second commonest form of cancer in children Accounts for 3.5% of all deaths in the 1-14 year age group Sixth commonest cause of cancer deaths in adults 25% of all tumors in adults are in the brain and 35% are neurectodermal and 40% are metastatic ~ Most primary tumors are sporadic and of unknown aetiology ~ Secondary tumors vary greatly between 14-40% ~ Fewer than 5% are associated with hereditary syndromes that predispose to neoplasia CNS neoplasms present with: ~ epilepsy (focal or generalised) ~ focal neurologic deficits ~ symptoms and signs of raised ICP ~ symptoms and signs of hydrocephalus Sites of cerebral tumors SSites of cerebral tumors ADULTS Supratentorial tumors account for 90% Therefore increased incidence of epilepsy and decreased incidence of headache Posterior fossa tumours cause headache and vomiting as early features CHILDREN Cerebellum Pons Optic nerve/chiasm SUPRATENTORIAL TUMORS ARE RARE Therefore Headache, vomiting, visual disturbances common Epilepsy - unusual Diagnosis 1. Clinical picture 2. CT or MRI scan 3. Biopsy ~ smear ~ Frozen section ~ paraffin section Epidemiological aspects of stroke ~ In the USA stroke is the third commonest cause of death ~ Incidence increases with age ~ Major risk factors for stroke are hypertension, cardiac disease, smoking, hyperlipidemia, and diabetes ~ Other causes OCP, sickle cell, coagulation disorders ~ In USA - brain infarction 10 times commoner than haemorrhage Blood supply to the brain ~ Human brain approx 2% of body weight ~ Receives 15% of total cardiac output O2 consumption approximately 20% of whole body (i.e high metabolic rate) ~ How long would the brain survive if blood flow interrupted Terminology ~ Ischaemia - arterial stenosis or occlusion Infarction - perfusion territory of the affected vessel ~ Global brain ischaemia - < CPP below the threshold for autoregulation i.e when systemic blood pressure falls very low e.g cardiac tamponade, heroin overdose, or ICP rises to a level that compromises cerebral perfusion Resultant brain damage or infarction is accentuated in the WATERSHED REGIONS CPP= SAP - ICP CPP > 40 mmHg - necessary for autoregulation If CPP < 40 mmHg CBF falls dramatically Selectively vulnerable zones ~ Hippocampus - CA1 ~ Laminae 3 and 5 of cortex ~ Purkinje cells cerebellum HYPOXIA - blood flow to the CNS may be normal or increased Damage occurs in selectively vulnerable neurones CIRCLE OF WILLIS Berry aneurysms Congenital Risk of bleeding inc; • Hypertension • AVM • systemic vascular disease • defects collagen • polcystic renal disease ICH causes • • • • • • • • • • Hypertension Trauma CAA Berry aneurysm AVM Bleeding diathesis Vasculitides Drugs Neoplasm Infective CNS INFECTION Development and outcome depends on Organism Host nature route of entry dose Anatomical defenses - skull, meninges Physiological - immune defense mechanisms Bacteria Entry into the cranial cavity Haematogenous - distant foci e.g lung Local spread - Skull - middle ear, nasal sinus, osteomyelitis Abnormal routes - Trauma -fractures Surgery - shunts Congenital sinus BACTERIAL INFECTIONS Depending on their virulence/pathogenicity bacteria can induce: 1. Purulent lesions 2. Cellular inflammatory reactions with giant cells 3. Inflammatory oedema caused by toxins and other inflammatory substances released by bacterial secretions or lysis, in the absence of bacterial replication PYOGENIC INFECTION 1. BONE – EPIDURAL – usually spinal sec to osteomyelitis 2. DURA MATER - SUB DURAL - sec to sinusitis, otitis etc. 3. ARACHNOID – SUBARACHNOID – sec to haematogenous spread of bacteria 4. PIA - INTRAPARENCHYMAL - abscess SUBDURAL Three organisms responsible for acute meningitis in childhood or adult life • Meningococcus • Haemophilus influenza • Pneumococcus Bacterial meningitis Complications of acute meningitis in the neonate • Obstructive hydrocephalus • Cavitating lesions in the white matter CSF Bacterial Viral TB low low v. high N glucose Slightly Raised protein increased neutrophil lymphocyt lymphocyt cells s es es Complications of bacterial meningitis • Acute inflammation of adjacent structures • Organisation of inflammatory structures Organisation of inflammatory exudate Impedes flow of CSF into venous sinuses Obstructs CSF outflow from IV ventricle Cerebral abscess ~ Mean age – 35.2 ~ P/C – headaches, pyrexia, altered mental state (depends on site, number, and +/- secondary cerebral lesion) ~ Site – frontal lobe commonest ~ Majority – associated with sinusitis, mastoiditis 20% no source ~ Bacteria isolated from 73%. Polymicrobial – 17.7% ~ Anaerobes – 13.6% ~ 9.8% died ~ 11% developed epilepsy Cerebral abscess Predisposing conditions Local – otitis media, sinusitis, trauma Systemic ~ chronic lung disease ~ cyanotic congenital heart disease ~ transplants ~ immunosupression Parenchymal abscess formation ~ Early cerebritis (days 1-3) ~ Late cerebritis (days 4-9) ~ Early capsule formation (days 10-13) ~ Late capsule formation (days 14 onward) AIMS OF TREATMENT ~ Eliminate infectious process ~ Reduce mass effect within cranial cavity – thus reduce secondary injury ~ Treat infections Tuberculous meningitis Usually M Tuberculosis More commonly associated with documented history of tuberculosis exposure in children than adults CSF Bacterial Viral TB glucose low N low protein v. high cells Slightly Raised increased neutrophil lymphocyt lymphocy s es tes