* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Integumentary System – Catalase, Mannitol Salt Agar
Survey
Document related concepts
History of virology wikipedia , lookup
Marine microorganism wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Gastroenteritis wikipedia , lookup
Disinfectant wikipedia , lookup
Infection control wikipedia , lookup
Urinary tract infection wikipedia , lookup
Anaerobic infection wikipedia , lookup
Neonatal infection wikipedia , lookup
Triclocarban wikipedia , lookup
Human microbiota wikipedia , lookup
Transcript
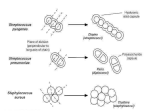
Lab 5: INTEGUMENTARY SYSTEM BACTERIOLOGY AND IDENTIFICATION THE INTEGUMENTARY SYSTEM: A PROTECTIVE BARRIER USUAL MICROBIOTA OF THE INTEGUMENTARY SYSTEM Trillions of bacteria live on our skin So then why aren’t we sick all of the time? Because the bacteria are mostly harmless and some even beneficial. INTEGUMENTARY SYSTEM WHEN THE LAYERS OF THE SKIN ARE INTACT, THE BACTERIA REMAIN ON THE OUTSIDE. INFECTIONS CAN ARISE WHEN THE SKIN IS DAMAGED BY: • EXTERNAL TRAUMA – SURGERY, BITES, BURNS, ABRASIONS, TRAUMATIC IMPLANTATION INTEGUMENTARY SYSTEM INFECTIONS CAN ALSO ARISE FROM SYSTEMIC DISEASES OR CHRONIC INFECTIONS SUCH AS: • DIABETES • VASCULAR • METABOLIC • IMMUNE (HIV) OR AUTOIMMUNE USUAL MICROBIOTA OF THE INTEGUMENTARY SYSTEM • Bacteria most commonly found on skin include: – Staphylococcus species (Gram-positive cocci in clusters) – Streptococcus species (Gram-positive cocci in pairs and chains – Corynebacterium species (Diphtheriods) (Grampositive rods) – Anaerobic bacteria – Fungi – Pathogens in low numbers PATHOGENS OF THE INTEGUMENTARY SYSTEM • Staphylococcus aureus • Gram-negative rods (Pseudomonas spp. or enteric) • Streptococcus spp. (S. pyrogenes (Group A strep or S. agglactica (Group B strep) • Enterococci (E. faecalis or E. faecium) • Fungi (yeast [Candida spp.] and filamentous) Staphylococcus aureus • Most pathogenic of the staphylococci – Produce and secrete several toxins and enzymes that act on host immune system to mediate cell destruction • Normal microbiota: Skin surface, upper respiratory tract, nares, axilla, groin, and perineum; can colonize various epithelial and mucosal membranes • Cause a wide range of infections: – Superficial skin infections; wound infections – Deep infections—can cause bacteremia and involve bones, joints, deep organs, lungs and respiratory – Scalded skin syndrome; toxic shock syndrome; food poisoning Staphylococcus epidermidis • Ubiquitous member of normal microbiota and often encountered in the laboratory as a contaminant • Normal microbiota: skin and mucous membranes; distributed widely over body surface • Can cause infections in immunocompromised patients. – Important nosocomial pathogen – Associated with indwelling prosthetic devices— intravascular catheters, cardiac valves, joints, cerebral shunts; bacteremia; UTIs; wounds Staphylococcus saprophyticus • Second most common cause of uncomplicated UTIs in women • Normal microbiota: skin and mucosa of the urogenital tract • Cause urinary tract infections: – Sexually active, young females – Prostatitis in men – Infections in sites outside of urinary tract are uncommon TYPES OF INFECTION Folliculitis Necrotizing fascitis Furuncle Cellulitis Surgical wounds Impetigo Bug bites THE INTEGUMENTARY SYSTEM: SPECIMEN COLLECTION FOR DIAGNOSIS • THE SAMPLE (TISSUE OR FLUID) IS COLLECTED WITH A SYRINGE OR SPECIAL SWAB USING ASEPTIC TECHNIQUE. • UPON RECEIPT, THE MICROBIOLOGY LABORATORY WILL PERFORM A: – GRAM STAIN • LOOKING FOR WHITE BLOOD CELLS AND PRESENCE OF MICROORGANISMS – CULTURE • TO ISOLATE, IDENTIFY AND PERFORM SUSCEPTIBILITY TESTING ON PATHOGENIC MICROORGANISMS. LABORATORY TESTING So how do we identify any staphylococci that is growing and whether or not it could be causing an infection? To Rule Out Staphylococci: – GRAM STAIN – BIOCHEMICAL TESTS: • CATALASE • MANNITOL SALT AGAR • COAGULASE TEST GRAM STAIN Staphylococci are: • Gram positive • Cocci • Arrangement in pairs or clusters CATALASE TEST • Hydrogen peroxide is toxic to cells • The catalase test detects the presence of the enzyme catalase • Catalase breaks down hydrogen peroxide into water and oxygen • Used on the bench-top to differentiate two common groups of microorganisms that can cause skin infections – Staphylococci produce catalase – Streptococci do not produce catalase CATALASE TEST PROCEDURE SPECIALIZED MEDIA REVIEW Selective Differential MANNITOL SALT AGAR (MSA) • Mannitol Salt Agar is a growth medium containing the sugar mannitol and high concentrations of salt. • Mannitol salt agar is both a selective and differential medium used to detect and differentiate Staphylococcus species • Selective because it contains a high concentration of salt (7.5% NaCl) which allows for growth of only salt-tolerant (halophiles) staphylococci to grow. • Differential because it contains mannitol and the pH indicator phenol red. Fermentation of mannitol by pathogenic staphylococci produces acid, which decreases the pH and causes the agar to change from red to yellow. Mannitol Salt Agar Lab Procedure COAGULASE TEST Bacteria that produce coagulase use it as a defense mechanism by clotting the areas of plasma around them, thereby enabling themselves to resist phagocytosis by the host's immune system 1.Mix a drop of plasma and the catalase positive organism on a glass slide 2. Look for the presence or absence of agglutination CATALASE TEST Streptococci are Gram-positive, catalase negative (no bubbles) Staphylococci are Gram-positive, catalase positive (bubbles) Mannitol Salt Agar Results MANNITOL SALT AGAR NEGATIVE MSA TEST POSITIVE MSA TEST POSITIVE TEST IS GROWTH AND FERMENTATION OF MANNITOL (YELLOW) Mannitol Salt Agar Lab: RESULTS COAGULASE TEST NEGATIVE (Coagulase - negative staphylococci) POSITIVE (Coagulase - positive staphylococci) (Staphylococcus aureus) THE USE OF MSA / COAGULASE TEST IN DIAGNOSIS • Staphylococcus aureus – COAGUALASE POSITIVE STAPHYLOCOCCI • The most pathogenic of the staphylococci • Produce toxins and enzymes that lead to harmful effects on the body • Cause of a variety of skin, respiratory, and blood infections (MRSA and VRSA) • COAGULASE NEGATIVE STAPHYLOCOCCI (Staphylococcus epidermidis and other species) • Staphylococci that are not as pathogenic as S. aureus, but can cause infection in compromised hosts, BSI (catheterrelated) DICHOTOMOUS KEY FOR IDENTIFICATION OF STAPHYLOCOCCI GRAM POSITIVE COCCI IN PAIRS OR CLUSTERS STREPTOCOCCI CATALASE NEGATIVE Staphylococcus aureus CATALASE TEST MSA PLATE POSITIVE Staphylococci, not S. aureus CATALASE POSITIVE= Staphylococci MSA PLATE MSA PLATE NEGATIVE DICHOTOMOUS KEY FOR IDENTIFICATION OF STAPHYLOCOCCI GRAM POSITIVE COCCI IN PAIRS OR CLUSTERS STREPTOCOCCI CATALASE NEGATIVE Staphylococcus aureus CATALASE TEST POSITIVE Coagulase – negative Staphylococci CATALASE POSITIVE= Staphylococci COAGULASE TEST NEGATIVE