* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Alterations in Nutrition
Gluten-free diet wikipedia , lookup
Dietary fiber wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Food choice wikipedia , lookup
Calorie restriction wikipedia , lookup
Hadrosaur diet wikipedia , lookup
Ketogenic diet wikipedia , lookup
Vegetarianism wikipedia , lookup
Academy of Nutrition and Dietetics wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Raw feeding wikipedia , lookup
Low-carbohydrate diet wikipedia , lookup
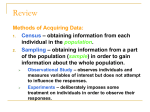
ALTERATIONS IN NUTRITION Jennifer B. Cowley, RN, MSN Objectives: * Who’s at risk? * Labs? Diagnostic tests? * Assessment - What do they look like? * Nursing Diagnoses - What’s the problem? * Therapeutic diets - What should they eat? * Nursing interventions - What should you do? * Enteral & parenteral nutrition - What are the nursing implications? Clients with Nutritional Problems: Who’s at Risk? Dietary history Medical history Lab Values Serum hemoglobin & hematocrit – “H&H” Serum albumin Serum pre-albumin Hemoglobin & Hematocrit Hgb - iron-containing pigment of the RBC’s – Normal lab values: • female - 12-16 g/100 ml • male - 14-18 g/100 ml Hct - % of whole blood occupied by RBC’s – Normal lab values: • female - 37-47% • male - 40-54% Albumin Synthesized in the liver from amino acids Accounts for > 50% total serum proteins Indicator of prolonged protein depletion Normal lab value: – 3.5-5 g/dl Pre-albumin A precursor to albumin Determines protein depletion in acute conditions Normal lab values: – 15-36 mg/kl Diagnostic Tests Gastroscopy – direct visualization Upper Gastrointestinal Series (UGI) – indirect x-ray exam Manifestations of Major Nutritional Deficiencies… Harkreader, p.703, Table 30-1 The nursing assessment enables the nurse to determine whether actual or potential nutritional problems exist. NANDA Nursing Diagnoses Altered Nutrition: Less than Body Requirements Altered Nutrition: More than Body Requirements Risk for Altered Nutrition: More than Body Requirements Examples of Secondary Nursing Diagnosis for Clients with Nutritional Problems Activity Intolerance r/t insufficient energy from protein depletion Altered Oral Mucous Membranes r/t oral intake Constipation r/t inadequate dietary intake and fiber Self-Esteem Disturbance r/t obesity Risk for Impaired Skin Integrity r/t intake of proteins, vitamins, and minerals Commonly Prescribed Therapeutic Diets Regular Diet – Who? • Clients who do not have special needs – What? • 2500 cal/day, variety of food groups Diets: NPO Nothing by Mouth (NPO) – Who? • Prior to surgery/certain diagnostic test • To rest the GI tract • When problem has not been identified – What? • NPO Diets: Clear Liquid Clear Liquid Diet – Who? • Surgical clients – What? • Only liquids that keep the GI tract empty (no residue) - i.e., apple juice, broth, carbonated beverages, gelatin. No dairy products Diets: Full Liquid Full Liquid Diet – Who? • Primarily postoperative clients – What? • Consists of liquids or foods that turn to liquid at body temperature Diets: Soft Soft Diet – Who? • For clients experiencing difficulty in chewing and swallowing; also for those with impaired digestion/absorption – What? • Avoid nuts, sees, raw fruits/vegetables, fried foods, whole grain. Diets: Mechanical Soft Mechanical Soft Diet – Who? • For clients experiencing difficulty chewing - i.e., poorly fitting dentures – What? • Similar to soft; however, allows clients variation permitting foods with different tastes, such as chili beans Diets: Pureed Pureed Diet – Who? • For clients with dysphagia – What? • Food that has been blenderized to a smooth consistency Diets: Low-Residue Low-residue Diet – Who? • Clients that need minimal GI irritation (diverticulitis, ulcerative colitis, Crohn’s disease) – What? • Has reduced fiber and cellulose. Avoid raw fruits (except bananas), vegetables, seeds, plant fiber, and whole grains. Limited dairy products (2 servings/day) Diets: High-Fiber High-fiber Diet – Who? • To increase elimination – What? • Opposite of low-residue Diets: Bland I don’t think so! Bland Diet – Who? • Clients with gastritis and ulcers – What? • Eliminates chemical and mechanical food irritants, such as fried and spicy foods, alcohol and caffeine Diets:Fat-Controlled Uh-oh! Low-Fat Diet – Who? • Clients with heart disease, atherosclerosis, and obesity – What? • Decreased saturated fats (replace with mono/polyunsaturated fats) and restricting cholesterol Diets: Sodium-Controlled Low-Sodium Diet – Who? • Clients with hypertension, heart failure, myocardial infarction/MI (heart attack), renal failure – What? • Mild - 2-3 g • Moderate - 1000 mg • Strict - 500 mg • Severe - 250 mg Diets: American Diabetic Association (ADA) Diabetic Diet A no-no! – Who? • Diabetics (of course!) – What? • Specified number of calories, amount of fat, carbohydrates, and protein at each meal, with snacks included. No concentrated sweets (NCS). Any diet is only as good as the client’s willingness to follow it. Meal plans should be individualized and developed in collaboration with the client. Monitoring Intake & Output/ “I&O” Purpose: To monitor client’s fluid status over a 24 hour period Who should be on I&O? Medical vs. nursing decision? Check clinical agency policy Inaccuracies of I&O I&O: Intake Oral fluids Ice chips Foods that become liquid at room temperature Tube feedings Intravenous fluids/medications Catheter/tube irrigants I&O: Output Urine Diarrhea Vomitus (emesis) Tube drainage I&O: Nursing Responsibilities Client/family teaching Documentation Relay to others that client is on I&O Look for trends over 48-72 hours The Malnourished Client: Nursing Interventions Stimulate the appetite Assist the client with eating Initiate client/family counseling Assisting the Client with Feeding ENTERAL NUTRITION If the client will not, should not, or cannot eat, enteral nutrition may be provided with nasogastric, gastric or jejunal tubes. Feeding tubes: Placement Nasoenterally Surgically – Gastrostomy – Jejunostomy Endoscopically – Percutaneous endoscopic gastrostomy (PEG) Placement of Enteral Nutrition Tubes Nasoenteral Feeding Tubes: Types Large-bore Small-bore – 90-95% of clients in hospital have small bore – more flexible, comfortable – stylet inserted into lumen Nasoenteral: Small-bore Feeding Tube Short term RN performs blindly at the bedside X-ray the only reliable method of placement verification Nasogastric, nasoduodenal, or nasojejunal Small bowel usually preferred over stomach in acutely ill clients Feeding Tube: Who does what? MD orders: – Type of tube – Rate and type of formula RN: – Inserts feeding tube – Administers/monitors tube feeding Enteral Feeding Tube: Confirmation of Tube Placement Radiologic confirmation Bedside methods: – Auscultatory method – Aspiration of gastric contents – pH method Gastrostomy/Jejunostomy: “G-tube/J-tube” Long term MD performs in OR Incision through abdominal wall creating an artificial fistula More cosmetically appealing/more comfortable Larger lumen allows more flexibility for feeding/medication administration Percutaneous endocscopic gastrostomy: “PEG” tube Long term MD performs at bedside or in endoscopy room Does not require surgery, therefore less risky and expensive than G/J tube insertion Percutaneous Endoscopic Gastrostomy Tube PARENTERAL NUTRITION Total Parenteral Nutrition “TPN” Total Parenteral Nutrition Candidates for What’s in Tonicity of Complications r/t Lipids given with TPN That’s All, Folks!