* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Urinary System - North Seattle College
Survey
Document related concepts
Transcript
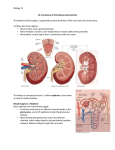
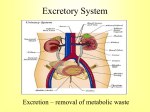
Urinary System Introduction 1. 2. 3. 4. Consists of Two kidneys Two ureters One urinary bladder One urethra Introduction Urine is excreted from each kidney through its ureter and is stored in the urinary bladder Introduction Urine is expelled from the body through the urethra Anatomy of Kidneys Retroperitoneal organs External Anatomy of Kidneys Hilus – A vertical fissure near the center of the concave medial border External Anatomy of Kidneys Ureters leave and blood vessels, lymphatic vessels, and nerves enter and exit at the hilus Internal Anatomy of Kidneys 1. 2. 3. 4. 5. 6. 7. Consists of Cortex Medulla Pyramids Papillae Columns Minor and Major calyces Renal pelvis Internal Anatomy of Kidneys Nephron – functional unit of the kidney Blood and Nerve Supply of the Kidneys Blood enters the kidney through the renal artery Blood and Nerve Supply of the Kidneys Blood exits via the renal vein Nephrons 1. 2. Consists of Renal corpuscle Renal tubule Renal Corpuscle Where fluid is filtered Renal Corpuscle Consists of 1. Glomerulus 2. Glomerular Capsule Renal Corpuscle Glomerulus – capillary knot Renal Corpuscle 1. 2. 3. The glomerular capsule consists of Visceral layer Parietal layer Capsular Space Renal Corpuscle The visceral layer consists of modified simple squamous epithelial cells called podocytes Renal Corpuscle The parietal layer consists of simple squamous epithelium and forms the outer wall of the capsule Renal Corpuscle Fluid filtered from the glomerular capillaries enters the capsular space Renal Corpuscle Capsular space – the space between the two layers of the glomerular capsule Renal Tubule Filtered fluid passes through here Nephron 1. 2. 3. Renal tubule Proximal convoluted tubule Loop of Henle Distal convoluted tubule Nephron Distal convoluted tubules of several nephrons drain into to a single collecting duct Nephron Many collecting ducts drain into a small number of papillary ducts Nephron These empty urine into the minor calyces Nephron 1. 2. 3. Loop of henle consists of Descending limb Thin ascending limb Thick ascending limb Nephron 1. 2. Two types of nephrons Cortical nephron Juxtamedullary nephron Cortical Nephron Has its glomerulus in the outer portion of the cortex Cortical Nephron And a short loop of Henle that penetrates only into the outer region of the medulla Juxtamedullary Nephron Has its glomerulus deep in the cortex close to the medulla Juxtamedullary Nephron Its long loop of Henle stretches through the medulla and almost reaches the papilla Renal Tubule and Collecting Duct Most of the cells of the distal convoluted tubule have receptors for ADH and aldosterone Juxtaglomerular Apparatus (JGA) Helps regulate blood pressure and the rate of blood filtration by the kidneys Juxtaglomerular Apparatus (JGA) 1. 2. Consists of Juxtaglomerular cells Macula Densa Juxtaglomerular Cells Located on an afferent arteriole Macula Densa Located on the distal convoluted abutting the JG cells Renal Physiology Nephrons and collecting ducts perform three basic processes while producing urine Renal Physiology 1. 2. 3. Glomerular filtration Tubular secretion Tubular reabsorption Glomerular Filtration Glomerular filtrate - the fluid that enters the capsular space Glomerular Filtration The principle of filtration – to force fluids and solutes through a membrane by pressure Glomerular Filtration Glomerular Filtration rate (GFR) – the amount of filtrate formed by both kidney per minute Glomerular Filtration GFR – 125ml/minute Glomerular Filtration This amounts of 180 liters of filtrate per day Glomerular Filtration Because of further processing we only excrete 1-2 liters of urine per day Glomerular Filtration Only call it urine after it drips out of the collecting ducts into the calyceal system Neural Autoregulation Through the ANS Neural Autoregulation During extreme emergencies such as shock, sympathetics to afferent arterioles cause them to constrict Neural Regulation Blood flow into glomerular capillaries is greatly decreased and GFR drops Neural Regulation Lowering of renal blood flow has two consequences Neural Regulation 1. Reduces urine output, which conserves blood volume Neural Regulation 2. It permits greater blood flow to other body tissues Neural Regulation Severe hypotension can cause death of part of the tubules, decreases urine output, and kidney failure Hormonal Regulation With mild drops of BP sympathetics stimulate renin secretion on JG cell by targeting B1 receptors Hormonal Regulation Renin converts angiotensinogen to angiotensin I Hormonal Regulation Angiotensin I is converted by angiotensin converting enzyme to angiotensin II Hormonal Regulation Angiotensin II causes efferent arteriole to constrict more than afferent arterioles, maintaining filtration Hormonal Regulation Angiotensin II also leads to the formation of aldosterone Hormonal Regulation Aldosterone causes sodium and water retention and potassium excretion Principles of Renal Transport Reabsorption – returns most of the filtered water and many of the filtered solutes (such as glucose, sodium, etc.) to the bloodstream Principles of Renal Transport Tubular secretion – the transfer of materials from the blood and tubule cells into tubular fluid Principles of Renal Transport Tubular secretion helps control blood pH and helps eliminate other substances from the body Principles of Renal Transport Solute reabsorption drives water reabsorption Reabsorption in the Proximal Convoluted Tubule The majority of the solute and water reabsorption from filtered fluid occurs in the proximal convoluted tubules Reabsorption in the Proximal Convoluted Tubule Reabsorption of Na and other solutes creates an osmotic gradient that promotes reabsorption of water by osmosis Reabsorption in the Proximal Convoluted Tubule 1. 2. 3. 4. 5. 6. 7. 8. Proximal convoluted Na transporters promote reabsorption of organic solutes such as Glucose Amino acids Bicarbonate ions Water Na K Cl Other ions and vitamins Secretion of NH3 and NH4 in the Proximal Convoluted Tubule The deamination of the amino acid glutamine by PCT cells generates NH3 and new HCO3- Secretion of NH3 and NH4 in the Proximal Convoluted Tubule Most NH3 quickly binds to H+ and becomes NH4+ Secretion of NH3 and NH4 in the Proximal Convoluted Tubule NH4+ can substitute H+ aboard the Na+/H+ antiporters and be secreted into tubular fluid Reabsorption in the Loop of Henle Water reabsorption is not directly coupled with sodium reabsorption Reabsorption in the Loop of Henle In the descending limb, water is reabsorbed via osmosis Reabsorption in the Loop of Henle As water is reabsorbed from the descending limb, the osmolality of the filtrate increases Reabsorption in the Loop of Henle In the ascending limb, Na+, K+, Clsymporters reclaim Na+, Cl-, and K+ ions from the tubular lumen fluid. Reabsorption in the Loop of Henle As sodium and chloride are reabsorbed from the ascending limb, the osmolality of the filtrate decreases Reabsorption in the DCT As fluid flows along the DCT, reabsorption of Na+ and Clcontinues due to Na+ - Clsymporters Reabsorption in the DCT The DCT serves as the major site where parathyroid hormone stimulates reabsorption of Ca2+ and excretion of phosphate Reabsorption and Secretion in the Collecting Duct Aldosterone increases Na+ and water reabsorption as well as K+ secretion by the collecting ducts and late distal convoluted tubules Reabsorption and Secretion in the Collecting Duct Some cells secrete H+ into the filtrate and reabsorb HCO3- into the bloodstream Reabsorption and Secretion in the Collecting Duct These cells help maintain body fluid pH by excreting excess H+ when the pH is too low or by reabsorbing less HCO3- when the pH is too high. Reabsorption and Secretion in the Collecting Duct ADH regulates water reabsorption by increasing permeability in the Collecting Duct and DCT Production of Dilute and Concentrated Urine The rate at which water is lost from the body depends mainly on ADH Production of Dilute and Concentrated Urine When ADH level is very low, the kidneys produce dilute urine and excrete excess water Production of Dilute and Concentrated Urine When ADH level is high, the kidneys secrete concentrated urine and conserve water Ureters Each of the two ureters connects the renal pelvis of one kidney to the urinary bladder Urinary Bladder Located in the pelvic cavity posterior to the pubic symphysis Urinary Bladder In the floor of the urinary bladder is a small, smooth triangular area, the trigone. Urinary Bladder The ureters enter the urinary bladder near two posterior points in the triangle Urinary Bladder The urethra drains the urinary bladder from the anterior point of the triangle Urinary Bladder In the area around the opening to the urethra, the circular fibers of the muscularis form the internal urethral sphincter Urinary Bladder The internal urethral sphincter contracts in response to sympathetics, and relaxes in response to parasympathetic stimulation Urinary Bladder Below the internal sphincter is the external urethral sphincter, which is composed of skeletal muscle Urethra A tube leading from the floor of the urinary bladder to the exterior Urethra Functions to discharge urine from the body Urethra The male urethra also serves as the duct for ejaculation of semen Incontinence A lack of voluntary control over urination Retention Failure to void urine completely or normally