* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download What is pain?
Survey
Document related concepts
Transcript
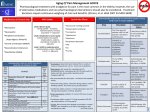
OVERVIEW and UPDATE Analgesia Dr Rebekah Moles Outline • What are the different types of pain? • How should opioids be used in the treatment of pain? • New opioid related drugs 2 What is pain? • Pain has been defined formally as: “an unpleasant sensory and emotional process which we primarily associate with tissue damage or describe in terms of such damage.” • Note: The inability to communicate, in no way negates the possibility that an individual is experiencing pain and is need of appropriate pain relieving treatment Pain Classification – Acute pain: short duration, cause often identifiable eg myocardial infarction, burn, appendicitis and kidney stones – Chronic pain: persists after healing is expected to be complete; caused by chronic disease; acute exacerbations can occur; management often difficult • Cancer • Non-cancer (eg. arthritis, low back pain) Classification of Pain • Physical causes – Nociceptive: activation of afferent fibres due to tissue injury or inflammation • Somatic eg skin & superficial structures • Visceral eg deeper structures – liver, pancreas – Neuropathic: nerve damage or nerve compression • Peripheral eg sciatica • Central eg post herpetic neuralgia – Mixed nociceptive/neuropathic • Brachial plexus lesion (deep somatic pain and neuropathic components Factors contributing to suffering Neural pain pathways Nociceptors in skin Sensory afferent fibres http://www.georgiapainphysicians.com/downloads/m1_slides/4.%20Spinal%20cord%20junctions.jpg Detection in the CNS http://www.georgiapainphysicians.com/downloads/m1_slides/4.%20Spinal%20cord%20junctions.jpg World Health Organization (WHO) Analgesic Ladder Step 1- Mild Pain • Non-narcotic medication Paracetamol NSAID Step 2- Moderate Pain • Add an opioid for moderate pain Paracetamol/Codeine World Health Organization (WHO) Analgesic Ladder Step 3- Severe Pain • Strong opioid Morphine Long-acting opioid such as MS Contin Note: All residents on around the clock opioids should be started on prophylactic bowel medications to prevent constipation Pain types & typical response (Adapted from AMH) Nociceptive Neuropathic Inflammatory Paracetamol Effective, regular use at max doses Less effective Opiods Effective NSAIDs Effective Often less effective when used alone May be effective in short term Effective analgesia; no antiinflamm effect May be effective initially; dose dependent Effective antidepressants & anticonvulsants ? – sedative – useful nocte Most effective May be effective as adjunct Opioids - Mechanism of action • Activation of peripheral nociceptive fibers causes release of substance P and other pain-signaling neurotransmitters from nerve terminals in the dorsal horn of the spinal cord • Release of pain-signaling neurotransmitters is regulated by endogenous endorphins or by exogenous opioid agonists by acting presynaptically to inhibit substance P release, causing analgesia Opioids – Mode of Action • Opioid receptors are classified into: – Mu: analgesia, respiratory depression and constipation (All) – Kappa: analgesia (mainly in the spinal cord), miosis, dysphoria and respiratory depression (Heroin, Pethidine. Buprenorphine = Kappa antag) – All these receptor sites antagonised by naloxone The family of opioids Similarities - mainly m receptor agonists 1. analgesia sleep 2. respiratory depression 3. nausea and vomiting 4. gastrokinesis 5. reversed by naloxone Differences 1. potency 2. pharmacokinetics 3. cost - availability 4. applications (?) 5. drug interactions (?) Equianalgesic Table PO/PR (mg) Analgesic SC/IV/IM (mg) 30 Morphine 10 6–8 Hydromorphone 1.5 15 Oxycodone 20 Methadone 10 100-150 Tramadol 180-240 Codeine Dosing Information Norspan 5 10 20 Morphine (oral / day) 20 40 80 Oxycodone (oral / day) 15 30 60 • No more than 2 patches (MAX 2x20) to be used at once • May require other SA drugs for 72hrs on initiation • No other analgesics for 24hr when discontinued Dosing information - Durogesic Codeine • 7-10% population lack CYP2D6 liver enzyme: – Codeine cannot be metabolized and therefore will not be effective • Doses less than 30mg are most likely sub therapeutic. • Doses more than 60mg will not provide further benefit at 2D6 will be saturated at that dose Opioid Therapy in Pain Related to Medical Illness Opioid therapy is the mainstay approach for • • • • Acute pain Cancer pain AIDS pain Pain in advanced illnesses But under treatment is a major problem Opioid Responsiveness • Opioid dose titration over time is critical to successful opioid therapy • Goal: Increase dose until pain relief is adequate or intolerable and unmanageable side effects occur • No maximal or “correct” dose • Responsiveness of an individual patient to a specific drug cannot be determined unless dose was increased to treatment-limiting toxicity Addiction • Rare when opioids given for pain control – Less than 1% – A study of 11,882 patients, no episode of addiction Porter and Jick, NEJM 302: 123, 1980 Breakthrough Pain • Incident pain – which occurs with or following physical activity, • End-of-dose failure – which occurs in the time before you are supposed to take your next dose of medication • Spontaneous breakthrough pain – which occurs without predictable cause or frequency Advances in opioid treatment Medication Safety As the Director of Pharmacy at the Royal Parade Hospital you have been asked to undertake a root cause analysis for a medication error that occurred on Ward 6W MS Contin 60 mg was administered to a patient instead of Oxycontin 60 mg ©Pharmaceutical Society of Australia 26 Oxycodone Sustained Release Oxycodone (Oxycontin) • New strengths: 15 mg and 30 mg • Potential for confusing with MS Contin (morphine) which also has 15 mg and 30 mg strengths • Oxycontin 15 mg: grey • MS Contin 15 mg: light green • Oxycontin 30 mg: brown • MS Contin 30 mg: purple ©Pharmaceutical Society of Australia 27 Oxycontin vs MS Contin * 5 mg 5mg 10 mg 15 mg 30 mg 60 mg 100 mg 200 mg ©Pharmaceutical Society of Australia 28 Hydromorphone sustained release (Jurnista) • Sustained release hydromorphone tablets in 8 mg, 16 mg, 32 mg & 64 mg strengths • Palladone XL withdrawn because of dose dumping when taken with alcohol • Immediate release (Dilaudid) in 2 mg, 4 mg and 8mg available • For disabling pain not responding to non-narcotic analgesics ©Pharmaceutical Society of Australia 29 Hydromorphone Dose: • Opioid naïve patients should be commenced on an immediate release product • Oral hydromorphone is estimated to be around 5 times as potent as morphine • 32 mg hydromorphone extended release = 160 mg oral morphine • If switching to hydromorphone from another opioid, switch between 1/3 and ½ of the equianalgesic total daily dose to allow for incomplete cross tolerance ©Pharmaceutical Society of Australia 30 Hydromorphone Role in therapy: • Allows doctors more options when managing moderate to severe chronic pain • Reduce frequency of medication administration • High risk of dependence and potential for abuse ©Pharmaceutical Society of Australia 31 Hydromorphone Practice points: • Jurnista should only be taken ONCE a day at the same time • Sustained release formulation should be swallowed whole • Ensure patients do not double up on chronic narcotic analgesics if switching over to new drug • Breakthrough analgesia may be required • Food has minimal effect on medication ©Pharmaceutical Society of Australia 32 Methylnaltrexone bromide (Relistor 12mg/0.6mL) Class: • selective μ opioid receptor antagonist Indication: • opiate induced constipation in advanced illness Mechanism of action: • blockage of μ receptors leading to reversal of peripheral effects from opiate analgesics ©Pharmaceutical Society of Australia 33 Methylnaltrexone bromide Dose: • Injected subcutaneously every SECOND day • Dosage based on weight – – – 0.15 mg/kg if under 38 kg or over 114 kg 0.4 ml (8 mg) if between 38 – 62 kg 0.6 ml (12mg) if between 62 –114 kg • Halve dose if CrCl < 30 mL/min Contraindication and precautions: • GI obstruction • Severe renal or liver impairment ©Pharmaceutical Society of Australia 34 Methylnaltrexone bromide Adverse effects: • Abdominal pain • Diarrhoea • Nausea • Flatulence • Dizziness ©Pharmaceutical Society of Australia 35 Methylnaltrexone bromide Clinical evidence – pivotal studies to date: Portenoy (2008) • Dose ranging study • 4 groups: 1 mg, 5 mg, 12.5 mg and 20 mg methylnaltrexone given on days 1, 3 and 5 • Primary endpoint: laxation within 4 hours of first dose • 5 mg, 12.5 mg and 20 mg group: 11/23 responded commercial dose • Followed by open label phase where 18 out of 33 continued similar results 36 Methylnaltrexone bromide Thomas(2008) • 2 groups: placebo and methylnaltrexone (0.15 mg/kg) • Outcomes were: – laxation within 4 hours of first dose – laxation within 4 hours after four subsequent doses • 48% of treatment group compared to 15% in placebo group had laxation response within 4 hours of 1st dose (p < 0.001) • Half of treatment group who had laxation response had it within 30 minutes of dose 37 Methylnaltrexone bromide Role in therapy: • Useful if not responding to traditional laxatives • Targeted therapy: does not induce withdrawal or interfere with pain management • No severe side effects • Quick action • Studies in specific patient groups only 38 Methylnaltrexone bromide Practice Points: • Administered subcutaneously • Dose is based on patient weight-check calculations • It is injected into the upper arm, thigh or abdomen • Site should be rotated, and areas with scars should be avoided • Bowel motion expected in ~ 30 minutes • Most common side effect is abdominal pain • No effect on analgesia expected 39 Rodney Rodney presents a script for Durotram XR 200 mg for dispensing His history shows that he was previously taking Zydol SR 100 mg twice daily for several months It has been six days since the last dispensing of his Zydol SR 100 mg Rodney tells you he was told to start the Durotram XR He has had his morning Zydol SR tablet 40 Tramadol Once Daily (Durotram) • Tramadol hydrochloride now available in once daily dosing (Durotram XR) • 100 mg, 200 mg & 300 mg tablets • PBS listing and indication- pain where aspirin and/or paracetamol alone are inappropriate or have failed • Releases 25% of dose within 2 hours of consumption • Remainder is released from the core at a constant rate over 24 hours. ©Pharmaceutical Society of Australia 41 Tramadol Once Daily Role in Therapy? • Similar efficacy to twice daily tramadol • Not useful for acute/breakthrough pain • Most common side effects: • • – dizziness or vertigo (10% to 26%) – drowsiness (7% to 30%) – constipation (10% to 34%) – nausea (11% to 33%) Dizziness and vertigo less common with the extended release product than sustained release (26% v 37% p = 0.017) Drowsiness is more common with extended release product than sustained release (30% v 21% p = 0.047) 42 Tramadol Once Daily Dose: • 200mg daily is recommended ‘starting dose’ when switching from regular immediate release tramadol 43 Tramadol Once Daily Dose: 44 Tramadol Once Daily Practice points: • Ensure patient is not confused with change of formulation • Remind patient that it is only ONCE daily (at the same time each day) • Sustained release formulation should not be broken, crushed or chewed • They may be more drowsy on this formulation • Be aware of drug interactions 45 Tapentadol Class: • A novel μ opioid receptor agonist and noradrenaline reuptake inhibitor Indication*: • For relief of moderate to severe acute pain in patients > 18 years (approval in US) Mechanism of action: • Opioid receptor effects combined with noradrenaline reuptake inhibition activates descending pain inhibitory pathways 46 Tapentadol Dose: • 50 mg –100 mg every 4 – 6 hours • Maximum daily dose: 600 mg/day • Daily dose on the first day may be increased up to 700 mg Contraindications & precautions: • Impaired pulmonary function • Paralytic ileus • Concomitant use with MAOI • CNS effects • Abuse potential • Use in epilepsy 47 Tapentadol Adverse effects: • Nausea • Dizziness • Vomiting • Somnolence • Itch • Constipation • Euphoria • ‘Feeling drunk’ 48 Tapentadol Clinical evidence - pivotal studies to date: Stegmann (2008) • Tapentadol 50 mg or 100 mg, oxycodone 10 mg (immediate release) or placebo every four to six hours • Primary outcome was to measure pain intensity, pain relief and time course of analgesia (SPI-24) • Both tapentadol and oxycodone provided greater analgesia over placebo • 100 mg tapentadol more effective than 10 mg oxycodone (p = 0.0455) but greater dizziness & somnolence 49 Tapentadol Hartrick (2009) • Trial of tapentadol in joint replacement • Tapentadol 50 mg, tapentadol 75 mg, oxycodone 10 mg and placebo every four to six hours • Outcomes measured were sum of pain intensity difference (SPID) over five days • All treatment groups reported improved pain relief compared to placebo (p < 0.001) • Nausea/vomiting and constipation lower in the tapentadol group 50 Tapentadol Role in therapy: • Acute pain relief • Much lower potential for serotonin syndrome compared with tramadol • Equivalence with opioids unknown • Role in severe pain or chronic pain yet to be established • ?Better side effect profile than oxycodone 51 Key Steps to Improving Treatment in Chronic Pain • Step 1: Administer medications routinely, not prn • Step 2: Use the least invasive route of administration first • Step 3: Begin with low dose-Titrate up • Step 4: Monitor & document effectiveness of medication daily • Step 5: Reassess and adjust dose frequently to optimize pain relief while monitoring and managing side effects Questions? 53