* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Approach to the Wheezing Child - West Virginia Association
Survey
Document related concepts
Transcript
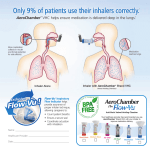
Approach to the Wheezing Child Maple Landvoigt, MD 11/7/14 Disclosures • I have no actual or potential conflict of interest in relation to this program/presentation. • I have no financial relationships to disclose. Objectives • Summarize the current scientific understanding of asthma. • Recognize when to treat and when to refer the child for further evaluation. • Recall current treatments for asthma. • Review best practice aerosol drug delivery devices and methods. • Identify other causes of wheezing including vocal cord dysfunction, malacia, and other underlying immunologic diseases. • Enumerate clinical pearls for the care of children with respiratory disease. Wheezing • Very common – 25-30% of infants, at least 1 in 3 children by 3 years. • Asthma – Also common… Scope of the Problem – – – – – – – – Over 25 million Americans have asthma. Nearly 3,500 annual deaths attributed to asthma and over 150 in children under the age of 15. The annual health care costs of asthma is over 50 billion dollars. It is one of the most common chronic disorders in childhood, affecting over 7 million children or 1 in every 11 kids in the US. More common in WV with a overall childhood lifetime asthma prevalence of nearly 15%. Asthma is the third leading cause of hospitalizations among children under the age of 15. It is one of the leading causes of school absenteeism accounting for approximately 10.5 million lost school days. The proportion of people with asthma in the United States has grown by nearly 15% in the last decade. From CDC National Asthma Control Program What is Asthma? “Asthma is a complex disorder characterized by variable and recurring symptoms, airflow obstruction, bronchial hyperresponsiveness, and an underlying inflammation.” – National Asthma Education and Prevention Program Expert Panel Report 3 (2007) http://www.nlm.nih.gov/medlineplus/magazine/issues/fall11/images/asthma-airways_lg.jpg The Trouble with Being Small Poiseuille's law R = 8nl/πr4 Overall Approach Follow Up National Asthma Education and Prevention Program Expert Panel Report 3 Diagnosis National Asthma Education and Prevention Program Expert Panel Report 3 (2007): 1. Episodic symptoms (history, physical exam) 2. Airflow obstruction that is at least partially reversible (spirometry: ≥ 12% change in FEV1 from baseline following short-acting beta agonist) 3. Alternative diagnoses are excluded Common Asthma Symptoms • Cough – Particularly with activity • • • • Wheezing Dyspnea Chest tightness Exercise limitation Goals of Treatment • Reduce Impairment – Prevent chronic symptoms. – Decrease frequent need for short-acting beta2-agonist (SABA). – Maintain near normal lung function and normal activity levels. • Reduce Risk – Prevent exacerbations. – Minimize need for emergency care, hospitalization. – Prevent loss of lung function (and for young children prevent reduced lung growth). – Minimize adverse effects of therapy. No treatments proven to change the disease progression (long term outcomes) Treatment 2007 (NHLBI) Reliever Medications • Short acting, used for acute symptoms. • Albuterol sulfate: – Relaxes the smooth muscles of the bronchi – Beta2-adrenergic agonist • Proventil HFA • Ventolin HFA • ProAir HFA • Levalbuterol: – R isomer of albuterol – Reportedly less tachycardia • Xopenex http://allergy.peds.arizona.edu/southwest/devices/inhalers-asthma/images/proventil1.jpg http://www.proairhfa.com/healthcare-professionals/images/section-1/Proair-inhaler-difference.png http://www.drug3k.com/img2/xopenex_11960_4_(big)_.jpg Other Relievers • Anticholinergic Agents • Ipratropium bromide: – Relaxes the smooth muscles of the bronchi – Inhibits secretions from serous/mucous glands – Typically used second line in Asthma – Sometimes used for tracheomalacia, bronchomalacia. • Atrovent http://www.atrovent.com/images/dosing-inhaler-mobile.png Controller Medications • Leukotriene receptor antagonists: – Non-steroid immunomodulator – Inhibits leukotrienes – Mild potency – Significant behavioral side effects have been noted • Montelukast (Singulair) • Zafirlukast (Accolate) Controller Medications • Inhaled corticosteroids: – Steroids are the most effective drugs for asthma control – Inhaled forms are topically active, poorly absorbed, and least likely to cause adverse effects – Reduce asthma mortality, hospital visits, and exacerbations – Higher doses may lead to steroid side effects – Cochrane review on growth effects: • Daily treatment lead to an approximately 0.5 centimeter decrease in linear growth during the first year of treatment • Effect is less pronounced in subsequent years • “This effect seems minor compared with the known benefit of these medications for asthma control” Cochrane Database Syst Rev. 2014 Jul 17. Inhaled corticosteroids in children with persistent asthma: effects on growth. Zhang, L. Controller Medications • Inhaled corticosteroids: • Fluticasone (Flovent) • beclomethasone dipropionate (QVAR) • Combination long acting beta agonist and inhaled corticosteroids: – Long acting beta agonists carry a black box warning • Fluticasone/salmeterol (Advair) • Budesonide/formoterol (Symbicort) • Mometasone/formoterol (Dulera) http://www.asthmasymptoms86.com/images/Flovent-inhaler1.jpg http://allergy.peds.arizona.edu/southwest/devices/inhalers-asthma/images/qvar.h4.jpg http://allergy.peds.arizona.edu/southwest/devices/inhalers-asthma/advair3.jpg http://www.multivu.com/assets/60910/photos/60910-457-Inhaler-F-4C-HR-original.jpg?1366812083 Devices and Drug Delivery • Nebulizers: – Commonly available – Slow – typically 15-20 minutes – Young children need to wear mask, blow-by decreases drug delivery to lower airways • MDIs without spacers: – Fast 1-2 minutes, portable – May improve adherence – Most of the medication is deposited in the mouth and GI tract • MDIs with spacers: – – – – • Significantly increases drug delivery to the lower airways Proper technique requires slow deep breaths Younger children or children with cognitive delay should use a spacer with mask Equally effective as nebulized medication when used properly Dry powder inhalers: – Fast, portable – Proper technique requires fast deep breaths – Not appropriate for pre-school and younger children. http://www.healthcare.philips.com/pwc_hc/main/shared/Assets/Images/Homehealthcare/Respironics/275s/optichamberDiamondInUse_275.jpg http://www.frx.com/pi/AeroChamberPlusFlow-VuSmall-Medium_PI.pdf http://images.rxlist.com/images/rxlist/flovent-diskus6.gif http://www.asmanex.com/static/images/bottle220_tcm682-19861.png How much is too much? • When do children need to see a specialist? Stepwise Approach for managing asthma in children 5-11 years of age Intermittent Asthma Persistent Asthma: Daily Medication Consult asthma specialist if step 4 care or higher is required. Consider consultation at step 3 Step 5 Step 2 Preferred Step 1 Low dose ICS Preferred Alternative SABA PRN LTRA, Cromolyn Nedocromil or Theophylline Step 4 Preferred Step 3 Preferred Preferred Medium Dose ICS + LABA High Dose ICS + LABA Either Low Dose ICS + LABA, LTRA, or Theophylline OR Medium Dose ICS Alternative Medium dose ICS + either LTRA, or Theophylline Step 6 Preferred High Dose ICS + LABA + oral corticosteroid Alternative Alternative High dose ICS + either LTRA, or Theophylline High dose ICS + either LTRA, or Theophylline + oral corticosteroid Patient Education and Environmental Control at Each Step Quick-relief medication for ALL patients SABA as needed for symptoms. Short course of oral corticosteroids maybe needed. Step up if needed (first check adherence, environmen tal control, and comorbid conditions) Assess control Step down if possible (and asthma is well controlled at least 3 months) Not All That Wheezes Is Asthma http://1.bp.blogspot.com/_-Uzu0xg5lh0/R6XkBDkhs6I/AAAAAAAAAIc/BbMW0MemCLM/s1600/DDX_of_Asthma-Children.jpg Types of Wheezing Polyphonic: • Multiple tones • Sounds musical • Associated with more distal airway disease • Classic asthma wheezing Types of Wheezing Monophonic: • Single tone • Repeated same sound • Associated with central airway disease • Concerning for underlying structural airway disease Structural Airway Disease • Tracheobronchomalacia: – Associated with coarse, monophonic wheezing. – Symptoms may persist past age 2, but typically do not persist past school age. – Causes impairment of mucous clearance and can lead to recurrent pneumonias. – Beta-agonists may worsen. – Can be associated with other anatomic anomalies. Structural Airway Disease • Stenosis can be either congenital or acquired in nature. – Associated with monophonic wheezing. – Risk factors: • • • • prolonged intubation aspiration prolonged or severe infections previous airway surgery • Compression is typically vascular in nature. – Consider vascular rings or slings. • Both stenosis/compression impair mucous clearance (can lead to recurrent pneumonias). Foreign Body Aspiration • Classically occurs in mobile toddlers, but can occur at any age including infants (particularly with toddler sibs) and older patients (especially those with developmental delays). • Concerning historical points include: – – – – Any witnessed choking event Persistent cough or wheeze Poor response to beta-agonist Persistent respiratory infections • Key respiratory findings include: – Focal monophonic wheeze • X ray or direct airway endoscopy may be need to confirm the diagnosis. Chronic Aspiration Syndromes • Unrecognized or untreated can lead to bronchiectasis and severe lung disease. • Risk factors include: – – – – – Neurologic disease or developmental delay Vocal paralysis or paresis Swallowing dysfunction Reflux or upper GI anatomic abnormalities Increased work of breathing. • Concerning historical points include: – Coughing, choking, or gagging with oral intake – Recurrent respiratory infections – Pooling of oral secretions Occult Immunodeficiency • Can lead to bronchiectasis and severe lung disease. • Concerning historical points include: – Persistent cough or wheeze – Productive cough – Recurrent respiratory and unusual non-respiratory infections. • Key respiratory findings include: – Coarse crackles – Monophonic and/or polyphonic wheezing – Associated findings of chronic inflammation (i.e. digital clubbing). Digital Clubbing http://medlibes.com/uploads/Screen%20shot%202010-07-19%20at%205.51.24%20PM.png Vocal Cord Dysfunction • Partial closure of the vocal cords during inspiration. • Can occur in combination with other pulmonary processes. • In children, often can persist after an initial triggering irritant (reflux, post-nasal drip) or can be related to anxiety. • Concerning historical points include: – – – – – Difficulty getting air “in” vs. “out” Throat tightness or pain Extreme sensitivity to smells (perfume, etc) Inspiratory stridor in the older child, particularly during exercise Poor response to controller medications • Spirometry can be diagnostic when showing intermittent inspiratory obstruction. Summary • Asthma is characterized by respiratory symptoms and airflow obstruction that is reversible or variable in nature. • The diagnosis is typically confirmed by thorough history and physical as well as spirometry. • Current standard of care treatment involves initiation of inhaled corticosteroid controller for frequent symptoms as well as beta-agonist rescue therapy with frequent monitoring to step up or step down therapy as needed. • Common barriers to optimal asthma control include incorrect inhaler technique and poor adherence. • Use of a spacer device improves drug delivery to the lower airways. • Proper evaluation of uncontrolled or severe asthma often requires detailed examination by an asthma specialist and testing to rule out other underlying respiratory disease. The End