* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Malaria
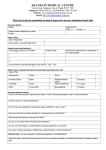
Survey
Document related concepts
Transcript
Travel Associated Infections Sunanda Gaur, MD Qtr 1st 0 100 Qtr 2nd Qtr 3rd Qtr 4th Travelers’ Health Risks Of 100,000 travelers to a developing country for 1 month: – 50,000 will develop some health problem – 8,000 will see a physician – 5,000 will be confined to bed – 1,100 will be incapacitated in their work – 300 will be admitted to hospital – 50 will be air evacuated – 1 will die Steffen R et al. J Infect Dis 1987; 156:84-91 (ISTM) Infectious Disease Risks to the Traveler • • • • • • • • • • • • • Malaria Diarrhea Leishmaniasis Rabies Dengue Meningococcal Meningitis • Hepatitis A ETC. Schistosomiasis Tuberculosis Leptospirosis Polio Yellow Fever Measles JEV Diseases in Returning Travelers • Fever : Malaria, Dengue ,Typhoid, nonspecific • Diarrhea : Giardiasis, Amebiasis, bacterial, non specific • Dermatologic : Insect bites, CLM, allergic rashes • Non diarrheal Intestinal disorders : Hepatitis, Strongyloidosis N Engl J Med 2006; 354:119-130 Fever in the Returned Traveler Geosentinal sites study CID 2007 44: 1560-8 ( n=6957) • • • • • • • Malaria 21% Acute Diarrheal Disease 15% Respiratory Illness 14% Dengue 6% Salmonella Infections 2% Tick borne Illness 2% 3% had vaccine preventable illness ( Hep A, Typhoid Fever, Influenza ) Causes of imported fever by region Africa Asia Americas Malaria 35% Unknown etiology 19% Unknown etiology 33% Unknown etiology 25% Respiratory 13% Respiratory 16% Respiratory 10% Dengue 12% Dengue 9% Bacterial enteritis 5% Malaria 11% Bacterial enteritis 9% Rickettsial 4% Bacterial Enteritis 9%, Typhoid 3% Malaria 4 % Bottieau et al Arch Int Med 166: 1642, 2005 Travel Health Resources • CDC Travelers’ Health Website – www.cdc.gov/travel • World Health Organization – www.who.int/int • State Department – travel.state.gov • International Society of Travel Medicine – www.istm.org • Health Information for International Travel – CDC “Yellow Book” • International Travel and Health – WHO “Green Book” Travelers’ Health Website www.cdc.gov/travel Traveler's Diarrhea • In general, up to 50% of travelers develop at least one episode of diarrhea during a two week stay • Onset usually within 2-3 days of arrival, > 90% occur within the first two weeks • A self limiting illness with significant morbidity Causes of Traveler’s Diarrhea Cause Bacteria Percent Isolation 50-75 Escherichia coli Enterotoxigenic Enteroadhesive Enteroinvasive 5-70 5-70 ? ? Campylobacter spp. 0-30 Salmonella spp. 0-15 Shigella 0-15 Aeromonas 0-10 Plesiomonas 0-5 Other 0-5 Causes of Traveler’s Diarrhea Cause Percent Isolation Protozao Giardia lamblia Entamoeba histolytica Cryptosporidium ssp. Cyclospora cayetanensis 0-5 0-5 0-5 ? ? Viruses Rotavirus Enterovirus 0-20 0-20 ? No pathogen isolated 10-40 Food and Beverage Precautions Boil it , peel it, cook it or FORGET IT !! Food and Water Precautions • Bottled water • Selection of foods – well-cooked and hot • Avoidance of – salads, raw vegetables – unpasteurized dairy products – street vendors – ice Traveler’s Diarrhea • Prevention : Antimicrobial prophylaxis is not recommended. • Early self therapy is recommended • • • • • • Oral rehydration Fluoroquinolones remain drug of choice Resistance is developing in some regions Azithromycin ( Mexico , Thailand, Morocco ), ? preferable Rifaximin ( non bloody stools, no fever) Non specific agents ( Bismuth subsalycilate, loperomide) Destination Specific Vaccines Vaccine Risk Region Yellow fever Parts of Africa and South America. (travel.state.gov) Hepatitis B SE Asia, parts of Africa, Middle East, Pacific Islands, parts of South America Hepatitis A All except Japan, Australia, New Zealand, north and west Europe, North America (except Mexico) Typhoid Developing countries Meningococcal Sub Saharan Africa Japanese Encephalitis Indian Subcontinent, SE Asia Cholera Outbreak setting Rabies South and SE Asia, Mexico, parts of South and Central America and Africa Plague Outbreak Setting The Meningococcal Meningitis Belt Don’t Forget the “Routine Vaccines” • • • • • MMR dT ( New dTaP ) Varicella IPV Hepatitis B Malaria Malaria MALARIA • • • • Plasmodium vivax* Plasmodium falciparum* Plasmodium ovale Plasmodium malariae * most common Malaria Risk • Oceania 1: 5 ( chloroquin res Vivax) • Sub-Saharan Africa 1:50 ( falciparum) • South Asia 1:250 ( mainly vivax) • SE Asia 1:2500 ( multi res falciparum) • Mexico/Central Am 1:10,000 ( Chloroquin sens) Malaria life cycle Malaria • All febrile returning travelers should be considered to have malaria until proven otherwise • Serial blood smears (thick and thin) every 8-12 hours in the first 24 – 48 hours • Thick smears are 10 – 40 times more sensitive than thin smears. Thin smears important for quantitation of parastemia • Important to identify the species Fatal Malaria • • • • 45 fatal cases between 1980 – 1992 98% caused by P. falciparum 82% acquired in Sub-Saharan Africa Most cases were associated with lack of chemoprophylaxis, suboptimal chemoprophylaxis, delay in seeking medical attention, and delay in diagnosis “ABCD” of malaria reduction –A –B –C –D Awareness of risk Bite prevention Chemoprophylaxis Diagnosis Mosquito Bite Prevention Vector Precautions • • • • • • • • • Covering exposed skin Insect repellent containing DEET 30 – 50% Treatment of outer clothing with permethrin Use of permethrin-impregnated bed net Use of insect screens over open windows Air conditioned rooms Use of aerosol insecticide indoors Use of pyrethroid coils outdoors Inspection for ticks Malaria Prophylaxis Drug Mefloquine Usage In areas with chloroquine resistant Plasmodium falciparum and vivax. Highly effective Adult Dose 22mg base (250 mg salt) orally, once/week, continue for 1 week after return Side effects 25% mild headache, GI upset, malaise, anxiety 1/250-1/500 nightmares, irritability, depression Comments Contraindicated in persons allergic to mefloquine. Not recommended for persons with epilepsy and other seizure disorders; with severe psychiatric disorders; or with cardiac conduction abnormalities. Malaria Prophylaxis Drug Doxycycline Usage An alternative to mefloquine Adult Dose 100 mg orally, once/day Pediatric Dose >8 years of age: 2mg/kg of body weight orally/day up to adult dose of 100 mg/day Comments Contraindicated in children < 8 years of age, pregnant women, and lactating women. Malaria Prophylaxis Drug Chloroquine phosphate Usage In areas with chloroquine sensitive Plasmodium flaciparum Adult Dose 300 mg base (500 mg salt) orally, once/week Pediatric Dose 5 mg/kg base (8.3 mg/kg (salt)) orally once/week up to maximum adult dose of 300 mg base Comments Malarone (Atovaquone and Proguanil Hydrochloride) • Atovaquone - a broad spectrum antiprotozoal inhibits the parasites mitochondrial electron transport. • Treatment with Atovaquone alone results in rapid development of resistance. • Atovoquone and Proguanil are synergistic against multi drug resistant P. falciparum • Several studies have demonstrated the efficacy of this combination in treatment and prophylaxis of multidrug resistant P. falciparum • Daily dosing ( 2-3 days prior, 7 days after), high cost • Occasional headache, GI upset Typhoid Fever • Caused by S.typhi or S. paratyphi • In US 445 cases/year between 1967 – 1994 • 72% of cases in the recent years (1985-1994) occurred in returning travelers • Travel to Mexico and India account for >50% of cases • Fever, chills, headache, malaise, abdominal pain, and constipation are common symptoms. • Blood cultures positive in 40-66%, bone marrow culture positive in 90% • Increasing antibiotic resistance – particularly in India – consider Ceftriaxone or Ciprofloxacin as first line therapy Commercially Available Typhoid Vaccines Available in the United States Drug Ty21a ViCPS Type Live Attenuated Polysaccharide Route Oral IM Min Age of Receipt 6 2 No. Doses 4 1 Booster frequency,y 5 2 <5% <7% Side Effects(incidence) Oral Ty21a Vaccine • • • • • • Live attenuated vaccine Enteri coated capsule – 1 cap every other day x 4 doses Efficacy – 65% Minimal to no side effects Contraindicated in immune compromised individuals Mefloquine can inhibit growth of Ty21a in vitro; delay vaccine at least 24 hours before or after Mefloquine • Concommitant or antimicrobials may effect vaccine efficacy GEOGRAPHIC DISTRIBUTION OF HEPATITIS A VIRUS INFECTION Hepatitis A Vaccine • Inactivated Vaccine • Approved for children 2-18 years old and adults • Highly Immunogenic – 88 – 90% seroconversion in 2 weeks – 99% seroconversion after 2nd dose • Duration of protection – under evaluation • Indicated for: – – – – – – Foreign travel Residence in communities with high endemicity Patients with chronic liver disease Homosexual/bisexual men IVDU Occupational risk Yellow fever Endemic Zones Yellow Fever Vaccine • Live vaccine • Required if entering endemic area or going from an endemic region to non-endemic region • Approved for children > 9 months old • Do not administer simultaneously with cholera vaccine • Under 4 months – unsafe (high incidence of post vaccination encephalitis) • Adverse effect ( viscerotropic disease) : 1 in 2-3 million World Distribution of Dengue 1999 Areas infested with Aedes aegypti Areas with Aedes aegypti and recent epidemic dengue Travel related Tick-Borne Diseases Tick Borne Relapsing Fever Israel, Africa, South Asia Every 3-5 days fever episodes African TBF Southern Africa Fever, h/a ,eschars Mediterranean Spotted fever Mediterranean , South Asia, E&S Africa Similar to African TBF, more severe TBE Central and E Europe Fever, Meningoencephalitis Lyme Borreliosis Europe Rash, 7th nerve palsy, aseptic meningitis Bloodborne and STD Precautions • Prevalence of – – – – • • • • • • STDs Hepatitis B Hepatitis C HIV Unprotected sexual activity Commercial sex workers Tattooing and body piercing Auto accidents Blood products Dental and surgical procedures Post Exposure HIV prophylaxis • • • • Assess likelihood of exposure Assess degree of exposure Begin ARV prophylaxis within 12-24 hrs. 2-3 drug combinations recommended depending on exposure risk . To be continued for 4 weeks. • http://www.cdc.gov/mmwr/PDF/rr/rr5409.pdf or http://www.ucsf.edu/hivcntr/hotlines/PEPline Pre Travel Check List Routine immunization Hepatitis A Immune Dose 1 Polio Immune One dose IPV Meningococcal One dose Booster Typhoid Oral 4 doses One dose IM Booster Malaria Chloroquin Mefloquin Malarone Doxy Diarrhea Loperamide Ciprofloxacin Azithromycin Oral rehydration Allergy Antihistamine Epi Pen Soft tissue infection Cefalexin bacitracin Motion sickness/GERD Dramamine/H2 blocker Food and water precautions Instruction Adventure/long stay Rabies Yellow fever JE Special problems Asthma Diabetes Mantoux status Dose 2 Travel Emergency Kit • Copy of medical records and extra pair of glasses • Prescription medications • Over-the counter medicines and supplies – Analgesics – Decongestant, cold medicine, cough suppressant – Antibiotic/antifungal/hydrocortisone creams – Pepto-Bismol tablets, antacid – Band-Aids, gauze bandages, tape, Ace wraps – Insect repellant, sunscreen, lip balm – Tweezers, scissors, thermometer Kibera, Nairobi Post-Travel Care • Post-travel checkup – Long term travelers – Adventure travelers – Expatriates in developing world • Post-travel care – Fever, chills, sweats – Persistent diarrhea – Weight loss Rabies • Rabies in travelers – an underestimated risk • 1980 – 1997 12/36 (33%) of human rabies deaths in US have been related to rabid animals outside the US • Canine rabies in endemic in the Indian Subcontinent, China, SE Asia, Philippines, Latin America, Africa and the former Soviet Union • In many rabies endemic countries, only Equine RIG and older Semple rabies vaccines are available • Equine RIG – significant risk of serum sickness • Semple type rabies vaccine is not as effective, and theoretical danger of allergic myeloencephalitis exists • Pre-exposure prophylaxis should be considered in selected cases Japanese Encephalitis Vaccine • • • • • Inactivated vaccine Efficacy = 91% Booster every 3 years Not approved for children under 3 years Side effects – Local reaction (10-25%) – Fever (10-25%) – Hypersensitivity reaction (0.6%) • Indications – Expatriates living in Asia – Travel to endemic regions for >30 days during transmission season, especially travel to rural areas