* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download MINOR
Survey
Document related concepts
Transcript
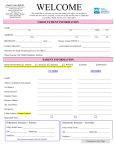
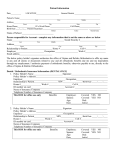
MINOR MEDICAL AND DENTAL HISTORY Please answer ALL questions to the best of your knowledge. The information requested below is very important. Please make it as complete and accurate as possible, as it will help us to provide the best possible health service. This information form becomes part of our permanent records and will be held in strict confidence. For patients of parents, complete this information for your child. Please update your medical history every 6 months. Name: ________________________________________________ Date of Birth: _________________ Age: _______ DENTAL 1. *Please describe the problem you would like to see corrected with orthodontics: ________________________ _________________________________________________________________________________________________________ YES NO 2. Does anyone in the family have a similar dental or facial condition? 3. Who referred you to our office? ______________________________________________________________________ 4. Name of family dentist: __________________________________________ Phone #: _____________________ Address: _____________________________________________________________ 5. Date of last dental appointment: __________________ 6. How frequently does patient brush? ____________ Floss? _________________ YES NO 7. Have the patient’s teeth ever been injured in the past? If YES, describe: __________________________________________________________________________________ 8. Has the patient ever had any of the following habits: Grinding / Clenching Lip biting/sucking Nail biting Tongue thrusting Thumb/ finger sucking Mouth breathing YES NO 9. Rate parent’s concern for correction of the orthodontic problem: Very concerned Concerned Indifferent Opposed Uncertain Very concerned Concerned Indifferent Opposed Uncertain Excellent Good Fair Poor Uncertain 10. Rate patient’s concern for correction of the orthodontic problem: 11. How do you think the patient will react to orthodontic treatment? 12. Has the patient ever had a consultation for orthodontic treatment before? YES NO YES NO 13. Has the patient ever had braces or any other orthodontic appliances? If YES, describe: __________________________________________________________________________________ MEDICAL 1. Name of physician: ____________________________________________________ Phone #: _______________________________ Address: ___________________________________________________ 2. Date of patient’s last physical exam: ______________________ 3. Please check if the patient is currently taking any of the following medications: Antibiotics Anticoagulants Anticonvulsants Antipsychotics YES NO YES NO Cortisone, Other steroids Aspirin Insulin Other: _____________________________________ 4. Is there a past history of the patient taking any of the above medications? YES NO If yes, please describe:________________________________________________________________________________ CONTINUED ON BACK PAGE → 5. Is the patient allergic to any of the following: 6. YES NO YES NO Local anesthetics Codeine Penicillin Latex Does the patient have a history of: YES NO YES NO Aspirin Barbiturates/sedatives Sulfa drugs Other allergies: _____________________________ Anemia Heart problems Asthma / emphysema Hepatitis/liver disease Arthritis High blood pressure Autism Kidney disease Bone / joint problems Mitral valve prolapse Brain injury Persistent cough Cancer: Coughing up blood _______________________________ Psychiatric problems Cerebral palsy Rheumatic fever Diabetes STD: _________________ Emotional difficulties Sickle cell anemia Epilepsy / seizures Speech difficulties Fainting or dizziness Stomach ulcer Headaches Thyroid disease Hearing difficulties Tuberculosis HIV+ / AIDS Other: _______________________________________ 7. Does the patient require antibiotics prior to certain dental treatments? YES NO CONSENT STATEMENT Elaine V. Sunga, DDS, Inc. and staff are hereby authorized to perform such dental and related surgical or medical treatments as deemed necessary to adequately provide such treatment for the above named patient. The undersigned understands and agrees that each patient’s records and materials pertinent to his/her treatment become property of Elaine V. Sunga, DDS, Inc. Dr. Elaine V. Sunga and staff are authorized to furnish, from the patient’s record, requested information of pertinent nature or excerpts thereof, to any approximate insurance company for the purpose of obtaining payment of the account of the patient. By signing, I also give my permission for the use of orthodontic records made in the process of examinations, treatment, and retention for purposes of professional consultations, research, education, or publication in professional journals by Dr. Elaine V. Sunga. I have read the preceding information fully, and understand it, and agree to comply with all rules and regulations for patient processing and treatment. To the best of my knowledge, the preceding answers are complete and accurate. _________________________________________________________ Signature of Parent / Guardian or Person Authorized to Consent for Patient _________________________________ Date ________________________________________________________ Witness Signature _________________________________ Date OFFICE USE ONLY: Date: _________________________ Health history reviewed by: _______________________________________ COMMENTS: ___________________________________________________________________________________________ _________________________________________________________________________________________________________ Health History Updates: (every 6 months while in active treatment) Any changes in the patient’s health or medications? Y N Any changes in the patient’s health or medications? Y N Comments: ________________________________________ Comments: ________________________________________ ___________________________________________________ ___________________________________________________ Signature: _______________________ Date: ____________ Signature: _______________________ Date: ____________ Doctor Signature: __________________ Date: ____________ Doctor Signature: __________________ Date: ____________ Any changes in the patient’s health or medications? Y N Any changes in the patient’s health or medications? Y N Comments: ________________________________________ Comments: ________________________________________ ___________________________________________________ ___________________________________________________ Signature: _______________________ Date: ____________ Signature: _______________________ Date: ____________ Doctor Signature: __________________ Date: ____________ Doctor Signature: __________________ Date: ____________