* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download supporting the use of medication in care settings
Survey
Document related concepts
Transcript
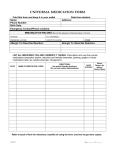
SUPPORTING THE USE OF MEDICATION IN CARE SETTINGS carer edition CONTENTS Chapter 1 medication law 04 04 04 05 05 05 The Medicines Act L egal classification of medicines Controlled Drugs Common Controlled Drugs Data Protection Act Best Practice Chapter 2 SERVICE USER PRESCRIPTIONS 06 06 06 07 07 07 Acute prescriptions Repeat prescriptions Ordering repeat prescriptions W ho orders the prescriptions? Medication Reviews Managed repeats Chapter 4 Administering Medication Safely 12 Safe working practice 13 Basics of administering medication 14 Pharmacy labels Chapter 5 When patients decline medication 18 Recording declined medication 18 Putting back medication in the pack 19 Covert administration Chapter 6 Information about medicines 21 Drug interactions Chapter 3 SAFE STORAGE & HANDLING OF MEDICATION 08 09 10 10 11 Temperature/light/moisture Fridge items Use of gloves ‘When required’ medicines Monitored Dose System Chapter 7 Administering solid oral medicines Chapter 10 Administering inhaled medicines Swallowing difficulties Crushing tablets and opening capsules Enteric coating What if patients chew medication? W hat if patients vomit after taking medication? 25 Lozenges and pastilles 25 Sublingual tablets 26 Buccal tablets 36 36 38 38 38 39 40 22 23 23 24 25 Chapter 8 Administering oral liquids 27 Medicines spoon 27 Measuring cups 28 Oral syringes Chapter 9 Applying topical medication 30 30 31 32 32 33 33 34 34 35 Creams/lotions/ointments/gels Medicated and non-medicated topicals W earing gloves Applying barrier creams Applying moisturisers Soap substitutes Applying non-medicated ointments Bath oils Applying medicated topicals Applying medicated patches Relievers Preventers Combination inhalers COPD Models of inhaler Spacer devices Administering an inhaler with a spacer device Chapter 11 Administering medication to the eye, ear & nose 42 Eye drops 43 Administering eye ointments 43 Patients who find it hard to keep their eye open 43 If a second drop is needed afterwards 44 Administering eye drops 44 Administering nasal drops 45 Administering ear drops Chapter 12 Important medications often taken by the elderly & how to administer 46 Alendronic Acid 46 Calcium supplements 47 references Chapter 1 MEDICATION LAW The Medicines Act 1988 Controlled drugs + Anyone can administer a prescribed + CDs are ordered on prescription in medicine to another person but must follow instructions from prescriber – i.e. what is on the label + Prescription medicines must only be administered to the person they are prescribed for, they remain the property of the patient and must not be shared with others the same way as all other medicines + Care professionals are allowed to collect CDs from the dispensary but you must provide some form of identification – you will be asked to provide your name and sign to say you’ve received the CDs. + If you are receiving a delivery of CDs from the dispensary then you are normally asked to sign something to say you have received them. + Generic name = Name of the drug e.g. ibuprofen + Brand name = Name each manufacturer gives that drug e.g. ibuprofen comes as Nurofen Legal classification of medicines GSL: General Sales List Can be bought without prescription from any shop/supermarket. P: Pharmacy Only Medicine Can only be bought in pharmacies under pharmacist supervision, often kept behind counter. CD: Controlled Drug Has the potential to be abused/stolen. Stored in a metal cabinet, recorded in CD register and with a witness present. POM: Prescription Only Medicine Can only be obtained with a prescription and only for the patient stated. 04 Common controlled drugs generic name uses brand names/formulations Temazepam Sleeping tablet Generic tablets, oral solution Morphine Pain killer Oramorph liquid, MST tablets, MXL capsules, Zomorph capsules Diamorphine Pain killer Generic tablets, syrup, injection Dipipanone Pain killer Diconal tablets Fentanyl Pain killer Abstral tablets, Effentora tablets, Instanyl nasal spray, Actiq lozenges, Durogesic DTrans patches Hydromorphone Pain killer Palladone capsules Methadone Pain killer Physeptone liquid and capsules Oxycodone Pain killer Oxynorm capsules, Oxycontin tablets Pethidine Pain killer Generic tablets and injections Buprenorphine Pain killer Temgesic tablets Pentazocin Pain killer Fortral tablets Methylphenidate ADHD Ritalin tablets, Concerta XL tablets Data Protection Act Best practice + Describes the information you can share + Means the current best way of working about patients e.g. medication details, health problems etc. + Ensures patient confidentiality and privacy. + The act states that you should only share sensitive information about patients with people who need to know if it’s in the patient’s best interest. For example with colleagues, doctors, nurses, pharmacists, social workers etc. + You should not disclose details about patients to friends, family or anyone else who doesn’t need to know. to get the best results + For medicines – guidance is issued by Royal Pharmaceutical Society of Great Britain who published ‘The Handling of Medicines in Social Care’ in 2007. 05 Chapter 2 SERVICE USER PRESCRIPTIONS Two types of prescription produced by the surgery: acute and repeat. Acute prescription + For acute illnesses that occur suddenly over a short period of time e.g. cough, cold, athletes foot, infection. An acute prescription is a one off prescription for a short course of medication – once it is finished there’s usually no need to order any more unless the illness hasn’t cleared up. In this case the doctor will need to be contacted and may want to see the patient again. Repeat prescription + Repeat prescriptions are for chronic illnesses which are long lasting and can’t normally be cured. Examples include: asthma, high blood pressure and arthritis. If a patient needs to take a particular medication for a long time the doctor can issue a repeat prescription. There is no need to make an appointment to see the doctor each time they need more of that particular medication. + Repeat prescriptions are usually for 28 days worth of medication, however the patient can ask the doctor for more than 28 days worth if need be. 06 Ordering repeat prescriptions + Each repeat prescription comes with a white tear-off repeat slip attached to it. This is a form used to order another prescription. Each item of medication that the person can have is listed on the repeat slip – to order more of an item the box needs to be ticked and the slip dropped into the box in the surgery + To order a repeat prescription, the dispensary needs a written request. + In person: simply drop your repeat slip into the practice. If you have lost this, ask and we will print you off another one. + By fax: fax your repeat slip to the practice + By email: go onto the practice website and follow the link on the front page that says ‘prescriptions’ + By post: send your repeat slip to the practice. Allow a minimum of two working days for a prescription to be sent to the chemist. Please note we do not take requests over the phone due to the risk of errors occurring and overloading an already busy phone line. Who orders the prescriptions? Medication reviews + It needs to be clear who is responsible for ordering the medication and should be recorded in the care plan. It may be a family member or a carer. If there are a number of different carers going in to see the patient everyone needs to be clear about who will be doing the ordering. + Don’t just re-order the same items each month – always check to see which items are needed. Medicines taken on a ‘when required’ basis are not always taken every day, therefore there may be enough left over from last month. + If the patient has run out of medication ask for ‘urgent’ to be written on the repeat slip and it will be put towards the top of the pile – the medication will possibly be ready for collection the same day. + Medication reviews are required to ensure the patient’s medication is correct and up to date. These may be at a clinic (LTMC), with a GP/nurse/pharmacist and may be conducted via a phone call appointment. Managed repeat medication for dispensary + We offer a managed repeat service where you can order what you need for next month when collecting your prescription. This makes ordering easier as it is one less trip to make and helps you to only order what you need. Please enquire at the Stowhealth complementary shop regarding this service. GUIDANCE Filling in a repeat prescription This half is your prescription to obtain your medication. This half is your repeat list which you should keep to enable you to order more. Tick the box if you need more of this item. If you don’t need any, leave it blank REVIEW DATE - your medication needs reviewing by this date. See “Review Dates”. 07 Chapter 3 Safe storage & handling of medication Medicines are affected by the environment in which they are kept and can be affected by: Temperature + Most medicines need to be stored at room temperature (below 25°C) + Too hot = the active ingredient can degrade (go off) or liquid medicines can grow microbes. Some medicines are so sensitive to heat that they need to be refrigerated + Too cold = medicines can also degrade especially if they are allowed to freeze or drop below a certain temperature Light + Light can also cause medicines to degrade. This is why bottles that pharmacies dispense into are made of brown plastic in order to reduce the amount of light that gets in. 08 Moisture + Moisture can reduce a tablet’s ability to dissolve or even break down the active ingredient. Sodium valproate tablets (an epilepsy drug) are sensitive to moisture. + Places to avoid storing medicines include the cupboard above a kettle – heat and steam could damage them, on a window sill – sunlight and heat could again damage them. Dressings, food supplements, urine bags and catheters should not be stored directly on the floor as any spillages can get them wet. + There are occasions when a selfmedicating patient may place themselves at risk by taking too much of their medication. If this happens often a risk assessment can be carried out to decide if it is safe for them to carry on selfmedicating. If not, it may be safer to store the medication directly away from the patient. + Medications should be ideally be kept in the patient’s locked medicine cabinet. + If there is a risk that the patient will still gain access to their medicines then it is acceptable to store them in the manager’s office or somewhere else away from the patient. However this must be an exception rather than the norm and a risk assessment must have concluded that this way is in the patient’s best interest. Staff must ensure that medicines are kept securely, at the correct temperature, with keys that are held securely and that fridges are monitored. Items that need to be stored in a fridge + You would know that a medicine needs to be stored in the fridge by the presence of a bag label saying ‘fridge’, on the label or in the patient information leaflet. + Some items which are normally kept in the fridge are stable at room temperature for short periods of time and can be kept out of the fridge for the time they’re being used. For example, some types of eye drops such as Xalatan and Xalacom (used for glaucoma) are usually stored in the fridge but can be stored at room temperature for four weeks. + Always write the date you first open the eye drops on the bottle and box. + Avoid placing medicines at the back of the fridge as they can get pushed against the back plate of the fridge and freeze which can damage medicines. 09 Use of gloves No need to wear gloves for the following: + Coated tablets and capsules: most tablets are coated in a film/sugar coating so you don’t touch the drug inside. Capsules are coated in plastic so there is no risk of absorbing any medication through your own skin. Wear gloves for the following: + Topical creams, ointments etc: Wear gloves or wash hands after application of medicated topical to prevent any medication absorbing through your own skin + Uncoated tablets (if you are allergic or pregnant): Unlikely that any medication would absorb through your own skin but a small theoretical risk – only problematic if you were allergic to that particular drug + Oral liquids (if you think spillage onto your own skin could occur): If you spilled liquid medication onto your skin and failed to wash it off you could get a small amount showing up in your blood stream. 10 + Drugs that cause rashes and cytotoxics: Chlorpromazine (used in mental health) can sometimes cause rashes in people who frequently handle the uncoated tablet or spill the liquid on them. It is a COSHH requirement to wear gloves in the handling of uncoated methotrexate (used in treatment of arthritis and psoriasis). Medicines prescribed as ‘when required’ + Also known as PRN and are medicines that are only taken when needed. Examples include pain killers, laxatives, indigestion treatments etc. + PRN medicines should be offered to the patient – if they do not want or need them then you do not have to let the doctor or supervisor know. They are not refusing them; they just don’t need any at that particular time. Monitored Dose System + Also known as MDS, blister packs or NOMAD trays and contain a whole week’s worth of medication + Always check you have the current week’s pack and check the patient’s name carefully + You cannot give medicines from MDS packs that have been filled by friends or family as there would be no pharmacy labels attached. As well as labels there should also be a written description of the tablets/capsules Examples of medication that is unsuitable for MDS packs: + Some types of tablet and capsule are not stable enough to be placed in MDS packs as moisture can enter and cause the active ingredient to degrade. Also the tops of the packs are clear – allowing light in which can damage certain medicines. Medicines in MDS packs are only stable for eight weeks. + Soluble tablets, dispersible tablets or sublingual tablets (under the tongue) or anything that cannot be swallowed whole. + PRN medicines – if they are placed in an MDS pack they tend to be given to patients regularly instead of only being given when they are needed. exampleS Medicines that need to be refrigerated MDS pack Dosette box 11 Chapter 4 Administering medication – safe working practices Safe working practices are to provide: The right medication to the right patient at the right dose in the right way at the right time right medication AT THE right TIME TO THE right PATIENT Safe working practice IN THE right WAY 12 AT THE right DOSE GUIDANCE Basics of Administering medication 1 If unfamiliar with the patient read the care plan to find out which tasks you need to carry out and any personal preferences they have 2 Check you have the current medicines chart and any other paperwork needed 3 Wash your hands or wear gloves if needed 4 C heck if the patient has already taken or been given any doses check the medicines chart or check with patient 5 F or PRN medication check any when required protocols or ask the patient if they need the item 6 If you are giving from MDS packs check that you have the correct weeks pack for the right patient. Check the medicines chart to see how many items are due. Check the MDS pack and make sure the blister you are about to pop out has the right number of items in. Check for any items listed on the medicine chart not in the MDS pack 7 If you are giving any medicines not in an MDS pack, compare the pharmacy label with the entry on the medicines chart. Make sure the following details agree: 1 Drug name 2 Drug strength 3 Form of the drug 4 Directions 5 Patient’s name 6 Expiry date 8 R ead any warning/cautionary and advisory labels on the pharmacy label e.g. take with food and act on them 9 Administer each item according to ‘best practice’ 10 Observe the patient take each item 11 E nter the correct code/your initials on the medicine chart only when you personally have seen the patient take or use the item or decline it 13 PHARMACY LABELS GUIDANCE Typical pharmacy label 1 Name 2 Strength 3 Form Asprin 75mg dispersible tablets 28 4 Direction 5 Patient’s name 6 Quantity Take ONE tablet Daily Dissolve or mix with water before taking Take with or after food Contains aspirin 7C autionary and advisory labels Mr John Greene 8D ate of dispensing 23 March 2012 1 Name of the drug 2 Strength The same drug can have two names the generic (e.g. diclofenac) and the brand name (e.g. Voltarol). Make sure the name on the label matches the name on the medicines chart. If the medicines chart has the brand name and the label has the generic name (or vice versa) it may still be okay to administer the medicine (you can check with a pharmacist for clarification). The same medicine can come in many different strengths, so check you’ve got the correct one. Strengths are written in various ways for example: 14 + Grams (g) + Milligrams (mg) there are 1000 milligrams in one gram + Micrograms (mcg) there are 1000 micrograms in one milligram For example: 4 Directions + Warfarin 0.5mg tablets + Warfarin 1mg tablets + Warfarin 3mg tablets + Warfarin 5g tablets + Digoxin 62.5mcg tablets + Digoxin 125mcg tablets + Digoxin 250mcg tablets Sometimes directions are written as ‘Take ONCE daily’ on the label, but state ‘Take ONCE in the morning’ on the medicines chart (or vice versa). This is okay as long as the two sets of directions don’t contradict each other. Directions such as ‘take as directed’ (or similar wording) are not acceptable for you to work from. The dispensary/pharmacy should be asked to seek directions from the prescriber and add them to the label. The strengths of liquids and creams are sometimes written as a percentage, for example: + Hydrocortisone 0.5% cream + Hydrocortisone 1% cream Some medicines are only available in one strength (e.g. lactulose) in which case the strength isn’t always written on the label or medicines chart. 3 Form Form means formulation. Medicines come in various formulations, for example: + Diclofenac dispersible tablets + Diclofenac gel + Diclofenac suppositories + Diclofenac injection + Diclofenac tablets + Diclofenac slow release tablets + Diclofenac capsules There are exceptions for this rule: drugs whose doses vary frequently such as warfarin or insulin can be labelled ‘Take as directed’. However there should be a way of finding out what the dose is. With warfarin you should always check the laboratory test results (INR results) before you give the dose. These INR results will tell you how many milligrams of warfarin to give the patient. Don’t just give the same dose of warfarin as yesterday without checking the results first as the dose may have changed. 15 5 Patient’s name Make sure the patient’s name on the label matches the patient’s name on the medicines chart. 6 Quantity The amount of medication in the pack 7 Cautionary and advisory labels These warnings are put on the label automatically by the dispensary’s computer system. They contain important information such as whether the drug needs to be given with food or on an empty stomach, or whether the drug causes drowsiness as well as other important information. These warnings are not always printed on the medicines chart and so you’ll need to check these on the label before administering the item to the patient. 8 The date of dispensing Not the expiry date, the date when the item was dispensed, i.e. on the 23rd March 2012. 16 Expiry dates (medicines often have two) + The expiry date before the pack is opened: medicines supplied in the manufacturer’s original packaging will have an expiry date printed on the pack or on any foil strips. Unfortunately if the dispensary repacks the item into another container, then this expiry date is sometimes lost. When this happens the advice from the regulators is to assume medicines are still in date 6 months after the date of dispensing. + The expiry date once the product has been opened: most medicines contain preservatives but they don’t protect the product forever. Once you open a pack of medication it starts to ‘go off’ (the active ingredient degrades and becomes less effective. Bacteria can also start to contaminate liquid medicines.) The table below shows examples of the shelf life on some liquids. LIQUID SHELF LIFE OTHER ITEMS SHELF LIFE ITEM SHELF life once opened ITEM SHELF life once opened Chlorpromazine syrup 6 months Oral liquids 6 months Ditropan elixir 28 days Creams in tubes 3 months Folicare 4 weeks Creams in jars/pots 1 month Frusol liquid 3 months Ointments in tubes 6 months Gastrocote liquid 1 month Ointments in jars/ pots 3 months Largactil syrup 1 month Eye drops 28 days Neoral oral solution 2 months Oramorph oral solution 90 days Phenergan elixir 1 month Risperdal liquid 3 months Antibiotic liquids 7-10 days (needs to be refrigerated) 17 Chapter 5 When patients decline their medication + We all have the right to refuse medication Recording when medicines and you should never pressure a patient into taking their medicines but gentle encouragement is okay + If you have more time to spend with the patient you could leave their medicines chart blank, walk away and try again later. Patients with dementia often forget they declined medication so you may be able to offer them the item again + It would be helpful to spend some time talking with the patient to find out why they don’t want their medication e.g. they find tablets hard to swallow – a pharmacist could recommend another formulation. They also may not know why they take the item - in cases like this a MUR (medication usage review) may be helpful. If you have a patient who is hiding medication from you instead of taking it, remind them that they have the right to refuse medication. They don’t need to pretend that they’ve taken doses they don’t want. 18 are declined + There comes a point when you have to code the medicines chart that the dose was declined – check and see what code to use. Also check what your policy is on declined medication – some people contact the prescriber straight away, some contact them after the patient has refused for more than 24 hours, some wait longer. It also depends on the drug declined. The time period can be agreed with prescribers. Can I put a tablet or capsule back in the pack? + If a tablet/capsule has come from a blister strip or MDS then you won’t be able to put it back. Don’t be tempted to try and re-seal it with tape. However if it has come from a bottle it may be okay to put it back although take great care to check you are putting the same tablet/capsule back. + Check that the patient will take the item of medication before you remove it from the pack so you won’t have to deal with any doses you have taken out. Covert administration + If the patient has adequate mental capacity then they have the right to decline their medicines, but what about patients with limited mental capacity? Laws and guidance state that if a person’s mental capacity is under doubt than an assessment of their mental capacity may be needed. + In cases where patients lack the mental capacity to take and understand their medications there are certain situations when we can hide medicines in food and drink, i.e. give a person their medication without them realising it (covert administration). However one of the difficulties with this is that you need to ensure the patient swallows the entire drink or meal to get the full dose. If the patient shares the living space with others you need to think about how you’d prevent someone else finishing their meal or drink and inadvertently swallowing their medicine. + Don’t confuse covert administration with putting medicines in food/drink to help someone swallow. If the patient understands that their medication is mixed with a drink or food then this is not covert administration. + The doctor, a social work team, family members and a pharmacist would all have to be consulted before covert administration could take place. 19 Chapter 6 Information about medicines + The amount of knowledge you are expected to have about the medicines you administer depends on how many different types you encounter on a dayto day basis. + It’s very important you have the right forms in place e.g. care plans, medicines charts, PRN protocols etc. These forms should contain all the information you need to give medicines safely and appropriately. The latest and best information sources that are available to you include: + Patient information leaflets: pharmacies are required to supply a patient information leaflet with each medicine they dispense – it should contain all the information you and the patient need. Make sure the leaflet you are reading is up to date as information about medicines sometimes changes. Patient information leaflets should be made available for the patient to read – you may have to help patients with limited mental capacity understand the leaflets by reading them out and explaining them using more simple language. 20 + BNF: the British National Formulary is designed to be used by pharmacists/ nurses/doctors and therefore contains quite a lot of medical jargon and terminology. However it contains a lot of detailed information on medicines. + www.bnf.org the British National Formulary is also available online + New Guide to Medicines & Drugs book: The British Medical Association produces a useful book aimed at the general public and has advice about what to do if a particular medicine is given late. + www.medicines.org/guides the Electronic Medicines Compendium (EMC) provides up-to-date, reliable and understandable information about medicines. It also allows you to download patient information leaflets for many different drugs simple language. exampleS BNF New Guide to Medicine & Drugs Drug interactions + Multiple items of medication can interact in other ways to produce a range of side effects. Some examples are: some cough/cold treatments contain paracetamol which when given with co-codamol could cause a paracetamol overdose. Ibuprofen can interact with a number of medicines such as lithium with sometimes quite serious consequences. + It’s best to advise any patient where there’s a risk that medication bought over the counter can interact with their prescribed medications or hide symptoms that might need investigating. It’s best to check with a pharmacist or the patient’s GP to see if they can be taken together safely. + Some policies state that you are only to assist with medication that has been prescribed. This is because prescribed items will already have been checked by a doctor and pharmacist and so shouldn’t interact with each other. If you are giving patients items of over the counter medication then these should be added to their medicines chart. 21 Chapter 7 Administering solid oral medicines Swallowing difficulties + Many people find swallowing tablets and capsules difficult + The wider the cup the better as the patient won’t need to tip their head back to get to the liquid - makes swallowing more difficult + Make sure you have filled the cup to the top with liquid otherwise they’ll need to tip their head back + Some people find it easier to swallow if they suck the liquid up with a straw + Swallowing problems can also occur if patients suffer from a dry mouth – you could give them a drink to wet their mouth with before they put the tablets in their mouth. + Many people find it easier to swallow capsules, sugar coated tablets, or a liquid formulation. Talk to the dispensary to see if they can change the formulation if necessary. + Most people need a drink in order to swallow tablets/capsules. You can always add some cordial if the patient prefers. + Milk can affect certain types of medication by reducing the amount of drug that gets absorbed. Check the cautionary and advisory warnings on the label if it says ‘do not take with milk’ then you’ll need to advise the patient about this. 22 + Most types of fruit juice are okay however grapefruit juice can interact with nifedipine, simvastatin and carbamazepine. Cranberry juice can also be a problem in some patients taking warfarin – there should be a warning on the label or within the patient information leaflet. + The caffeine in tea and coffee can interact with theophylline. Another problem with hot drinks is that patients cannot take a big enough ‘gulp’ to make sure the tablet is swallowed properly. There have also been cases where soft gelatine capsules have melted in the mouth when taken with a hot drink, releasing the drug into the mouth which can taste quite bitter. If the patient has milk with their tea or coffee check the label to see if it says ‘do not take with milk’. + Alendronic acid should only be given with water (no cordial and not mineral water). There are multiple warnings such as ‘take on an empty stomach’ surrounding alendronic acid which can be found in the patient information leaflet Crushing tablets and opening capsules + Some tablets are designed to be chewed e.g. Natecal + Some tablets are designed to be crushed e.g. Epilim crushable tablets + You could find this information by reading the patient information leaflet. However if the tablets you are administering have not been designed to be crushed/chewed then don’t crush them unless you’ve had permission from the pharmacist and doctor. Permission should be recorded in care notes. + Some capsules are designed to be opened up e.g. Zomorph. However unless it states in the patient information leaflet that you can do this, don’t open up any capsules unless you’ve had permission from a pharmacist and doctor. You have to be cautious when determining whether tablets can be crushed/chewed for the following reasons: + Some tablets are coated as there are + With enteric coated tablets and capsules there is always a warning on the label saying ‘swallow whole, do not crush or chew’. + Some tablets have a sugar (or film) coating which is not the same as an enteric coat. The sugar (or film) coating is just there to make the tablet easier to swallow. These coatings will dissolve in the stomach along with the tablet. The pharmacist might give you permission for you to crush sugar or film coated tablets. + Some tablets and capsules are slow release which is a mechanism designed to release the drug inside slowly throughout the day (or night). This means that instead of having to give the medicine a number of times throughout the day, the tablet or capsule can be given less frequently, i.e. only once or twice a day. By crushing slow release tablets/capsules you may end up giving the person an overdose as the entire day’s dose is released in one go. some drugs that can be damaged by acid in the stomach. To protect them they are coated in a film that doesn’t dissolve in acid known as an enteric coating. This coat will dissolve to release the drug in a more neutral or alkaline environment once it passes through the stomach into the intestines. Some drugs also have an enteric coat to stop the drug in them irritating the stomach lining. 23 + With slow release tablets and capsules there is always a warning on the label saying ‘swallow whole, do not crush or chew’. + You cannot crush tablets or open up capsules that are not coated or slow release unless you have had permission from a pharmacist and the doctor. Giving medicines in a way that the manufacturer didn’t intend them to be given is called a drug ‘off licence’ or giving it as an unlicensed drug. The prescriber has to be asked permission if any drug is to be given in an unlicensed way. + It is okay to break tablets in half if they have a ‘score line’ on them. You don’t need permission from the pharmacist/ doctor because the manufacturer has designed scored tablets to be broken in half if need be. GUIDANCE Breaking scored tablets 24 What if the patient chews their tablets or capsules? + Can sometimes occur in patients with dementia where swallowing difficulties can occur. It’s only enteric coated or slow release tablets/capsules that you need to worry about. This is important because if a patient chews a slow release tablet, they could end up having an entire day’s dose in one go which could be dangerous. Chewing enteric coated tablets might stop them working or cause stomach irritation. + If any of the medicines patients are chewing have these warnings on them (swallow whole, do not crush or chew) you’d need to warn the patient of the risks and let the pharmacist/doctor or another health professional know as soon as possible. + If the tablets that they are chewing are not slow release/enteric coated then there will be no warning on the label, however you could still contact the pharmacist as they may be able to change the item to a liquid or something that is easier to swallow. The patient would not be putting themselves in immediate harm by chewing tablets that are not slow release though. What if the patient vomits after taking any oral medication? Unlikely but if this does happen then contact a health professional (such as a pharmacist) they may advise you to give another dose if you can see the intact tablet/capsule in the vomit but do not do this unless you have checked with a health professional. Lozenges and pastilles + Occasionally prescribed by doctors, lozenges and pastilles are designed to be sucked and should be held in the mouth for as long as possible and allowed to slowly dissolve. + Patients taking any medication that needs to be sucked or chewed should avoid eating or drinking anything until the pastille or lozenge has fully dissolved. Sublingual tablets + Sublingual tablets are designed to be placed under the tongue instead of swallowed. From there the drug absorbs directly into the bloodstream and so it is able to work more quickly. One example of a sublingual tablet is glyceryl trinitrate (GTN) used to treat angina. + Once used, GTN should ease chest pain within 1-5 minutes. If needed, the patient can have another GTN tablet after 5 minutes. If they have taken 3 doses within 15 minutes and the chest pain is either no better or worse then you should call a doctor, or dial 999 as the patient may be having a heart attack. GTN can sometimes cause a headache – a recognised side effect and although uncomfortable is nothing to worry about. + GTN tablets expire 8 weeks after opening the bottle so it’s important to keep them in their original container, as a metal seal in the lid and the glass bottle is designed to protect the tablets. Any tablets remaining after 8 weeks need discarding and a fresh supply is required. 25 + GTN also comes as a spray for under the tongue. The spray does not expire after 8 weeks and may be used until its empty or has reached its expiry date. When patients feel chest pain, they should spray one or two puffs under their tongue. It’s important that the canister is held upright when spraying. After spraying, the patient should close their mouth; otherwise the spray can evaporate out of the mouth. GTN tablets and spray can tingle or burn under the tongue, which is normal. exampleS Sublingual tablets Buccal tablets + Designed to be placed between the upper cheek (or lip) and the top gum where they sit and dissolve. The drug then gets absorbed directly into the bloodstream and therefore works very quickly. + If the patient has a dry mouth, you can moisten the inside of it with some wet cotton wool. If you have a patient who needs this type of tablet regularly, it’s best to vary the place where the tablet goes a little (to stop irritation). Some types of GTN tablet come as buccal tablets. Some tablets used to treat nausea and sickness are also available in this form. GUIDANCE Administering buccal tablets 26 Chapter 8 Administering oral liquids When measuring out oral liquids, you have three choices of what to use: medicines spOON Only a 5ml medicines spoon is designed to accurately hold 5mls of liquid – not a metal teaspoon or any other type of spoon. However, most people tend to pour out less than 5ml – only 3 or 4ml. Whilst this may be less important if measuring out items such as cough medicines or treatments for indigestion, this could lead to more serious under-dosing if you are measuring out items such as antiepileptics, treatments for the heart, or antibiotics etc. To pour out 5ml you need to pour a heaped spoonful of liquid. Although spoons are not good for measuring out liquids, they can be easy to administer from. If the patient finds it hard to swallow from a measuring cup or oral syringe, you can always transfer the medicine to a spoon after measuring it out accurately using another device. Measuring cupS Many care professionals use graduated medicines cups to measure out liquids. If you are using these, it’s important to place them on a level surface to check you have the right dose. If you hold the cup up to eye level, you can end up holding it at an angle resulting in you measuring out the wrong dose. Medicines cups are more accurate than spoons, but many people tend to pour too much into them (sometimes 6 or 7ml when aiming for 5ml). Also, thick medicines can be left behind in the measuring cup. Measuring cups are better for larger volumes of liquid, e.g. 15 or 20ml. This is because over measuring by 1ml when aiming for 20ml gives you a 5% error, whereas over measuring by 1ml when aiming for 5ml gives you a 20% error. Generally speaking, most people manage to swallow liquids okay from measuring cups. However, you often have to tip your head back to get the last of the medicine from the cup. Tipping your head back and looking up can make swallowing difficult. This might be a problem if the patient has a swallowing difficulty, in which case spoons might be easier (after using a syringe to measure out the dose accurately). 27 Oral syringES Oral syringes are the most accurate method of measuring out liquids. They come with a plastic adaptor which you push into the bottle. You then push the syringe into the adaptor and turn the bottle upside down. You need to get rid of the air gap that you get when you first draw the liquid up. Push this air gap back into the bottle. A few small air bubbles are okay, but not an air gap. If you are holding the syringe pointing upwards, make sure it’s the top edge of the black ring that’s just touching the underside of the correct mark. If possible, it’s best to let the patient use the oral syringe themselves. This way they have control over how quickly they push the liquid into their mouth and it’s also more dignified. If the patient can’t do this on their own, then you may have to do it for them. Take care, as choking incidents have occurred when staff have pushed liquid in too quickly. It’s good if you have found a technique that works for you and the patient. As long as medication does not dribble out of their mouth and they find the technique comfortable, then you can use whichever technique suits you both. However the technique does need to minimise the risk of choking. 28 Rather than pushing the whole of the syringe into the mouth, place just the tip of the syringe between the front lips (which remain closed) in front of the teeth. If you push the syringe in between their teeth, the patient won’t be able to clench their teeth to swallow. Some people place the whole syringe in the side of the cheek, between the teeth and the inside cheek. Although the patient can clench their teeth to swallow, they can’t form a seal around the syringe, and liquid can leak out. Also, you can’t see how much liquid you are squirting in at a time. This is also not the most dignified way to treat the patient – hence just place the tip between the front lips. Not all patients can take 5ml in one go. If this is the case, squirt about 2.5ml in at a time then allow them to swallow this. Once they have swallowed it, push another 2.5ml in. In time, you may find that the patient is able to take a whole syringe-worth of medication in one go, however just be cautious to begin with. If you find that the patient doesn’t get on with syringes, you can always squirt the medicine bit-by-bit from the syringe onto the spoon and give it that way. Cleaning oral syringes Clean the syringe after each use with fresh, warm soapy water. Draw the plunger in and out several times until the inside of the syringe is clean. Separate the barrel and plunger and wash both in soapy water. Do the same to the adapter. Rinse under cold water and leave un-assembled to dry. You can use a dishwasher, but that doesn’t clean the medicine out of the tip. If you use a dishwasher, flush the medicine out first with fresh water. If you are administering into the mouth, oral syringes need to be clean, but not necessarily sterile. exampleS Medicines spoon Measuring cups Oral syringes Carry on using the oral syringes until the markings fade. 29 Chapter 9 Applying topical medication Topical products are products applied to the skin. In general terms this means creams, lotions, ointments and gels. + Creams are a combination of oil and water. They also contain extra ingredients such as emulsifying agents which allow the oil and water to mix, and preservatives to stop microbes growing in the water that creams contain. Medical creams don’t tend to contain colours or perfumes as these can sometimes irritate the skin. + Lotions are like creams but are designed to be applied over larger areas of skin. For this reason they are often thinner and contain more water. + Ointments are mostly made of oil or grease. They contain either no water, or just very small amounts. Since most ointments contain no water, they do not need emulsifying agents added or even much in the way of preservatives. Therefore they contain fewer ingredients, which means they are much less likely to cause skin irritation. Because they contain more oil, they moisturise the skin for longer, This is because the oil seals the water in the skin, preventing the skin from drying out. Some patients don’t like the greasy feel of them although they do make excellent moisturisers. + Gels are a much more recent invention and can be made of almost 99% water or any combination of oil and water. They remain fairly solid whilst they are in their container, but become softer when applied to the skin. 30 All of the above can have drugs added to them which would make them ‘medicated’ or they can be used as they are i.e. left as ‘unmedicated’ in which case they are often used as moisturisers. + Non-medicated creams, ointments, gels and lotions are most often used as moisturisers. An example is aqueous cream. Moisturising creams are normally applied quite thickly. With moisturising ointments, less is needed as they contain more oil. + Barrier creams and ointments are in a class of their own. Examples include Sudocrem, Conotrane and Cavilon cream. They contain a type of silicon which sits on the skin and acts as a repellent, keeping irritants such as sweat, saliva, urine and faeces off the skin. The silicon doesn’t get absorbed, so they aren’t really ‘medicated’ topicals, but because some of them also contain mild antiseptics they aren’t really non-medicated either. Wear gloves when applying topical medicines exampleS Non-medicated cream Medicated cream It’s best to wear gloves when applying any medicated cream/ointment/lotion/gel. This prevents the drug absorbing through your own skin. There is only a small risk of this happening, especially as you’d wash your hands afterwards, but it is possible. It’s best to spread topical products (medicated, non-medicated and barriers) onto the skin, rather than trying to rub them in. Spread them down the limb using a sweeping motion in the direction of hair growth (always down, away from the body). This is important if the patient has hairy skin as otherwise you end up brushing the hairs the wrong way which can be uncomfortable for them. Barrier cream Don’t try and rub topical products in vigorously, as this can irritate the skin and will take a long time. Skin is a barrier and it can take a while for things to soak through (depending on what is applied). As far as creams are concerned, they are mostly made of water. Most of this water dries into the air, rather than soaking through the skin. The active ingredient is then left behind on the skin to soak in. Rubbing creams around the skin just heats up the skin and causes the water to evaporate more quickly. 31 Therefore the advice is to stroke topical products across the skin and leave them there to soak in. However, although it is usually pointless trying to rub the cream in, some patients enjoy the massaging action when creams are applied. If massaging the skin is not causing any irritation and the patient enjoys it then carry on. It won’t cause the product to soak in more quickly but it might help the patient to relax. Applying barrier creams Many people apply barrier creams too thickly. You should stroke a small amount thinly across the skin, but still be able to see the skin through the cream. If the skin is very white, then you’ve applied too much. This can be difficult to wash off and the patient can end up with layer upon layer of barrier cream building up. The result is that their skin never gets cleaned underneath which can cause skin irritation. Therefore the advice is to stroke topical products across the skin and leave them there to soak in. However, although it is usually pointless trying to rub the cream in, some patients enjoy the massaging action when creams are applied. If massaging the skin is not causing any irritation and the patient enjoys it then carry on. It won’t cause the product to soak in more quickly but it might help the patient to relax. 32 Applying moisturisers A good moisturiser doesn’t just add water to dry skin, it adds plenty of oil to it in order to fill all the gaps between skin cells and restore the skin’s natural barrier function. With moisturising creams, the oil they contain has been diluted with water. This is why you need to apply so much, as shown below: Most patients will probably not want you to put this much on. You could ask them to try it for a week to see what difference it makes. Depending on how dry the skin is, it takes about 10-30 minutes for the water to dry off (some of the water soaks into the skin, most of it evaporates into the air). After the water has gone, you are left with a thin layer of oil on the skin. The oil then soaks into the skin over the next few hours. It fills the gaps between the skin cells, which seals in the water already present in the skin. Once you have applied all of this moisturising cream, the patient can get dressed over the top of it with an old dressing gown or clothes which they don’t mind getting a little greasy. It doesn’t stain most clothing (apart from silk) as the oil normally remains in the skin rather than soaking into the fabric. Any product will come off the fabric in the wash. Moisturisers work even better when applied to wet skin as they lock the moisture in. It’s best to pat the skin dry a little first to avoid diluting the cream too much with water. Some patients may have a limited understanding of why you have to apply this much (e.g. patients with a learning disability or dementia). It might be easier to use moisturising ointments with these people as they are less visible on the skin and less likely to get rubbed off. GUIDANCE Moisturising creams can be used as soap substitutes The water, oil and emulsifying agents in creams means they can act as a kind of soap. They can be kinder to the skin than normal soaps which often strip the skin of its natural oils. People with dry skin or eczema tend to use moisturising creams (such as aqueous creams) as soap substitutes. Applying moisturisers Applying non-medicated ointments Examples include Vaseline, Epaderm ointment, Emollient 50, Diprobase ointment etc. Moisturising ointments don’t need to be applied as thickly as moisturising creams, as they are made almost entirely of oil, so a thin layer is fine. It wouldn’t do any harm to apply them too thickly; you just don’t need that much. Unfortunately, people don’t always like the greasy feel of ointments on their skin, so although ointments are fantastic moisturisers, people often prefer water based (and often less effective) creams and lotions. Because ointments contain less water, they don’t need as many preservatives in them. Therefore with ointments, there’s less chance that people will experience the stinging sensations they can get with creams. 33 exampleS Moisturising ointment Bath oil Medicated topical Bath oils Examples include Oilatum and Balneum bath oils. These are oil based products added in small quantities to the bath water. They float on the surface of the water and coat the skin in oil. They don’t dry the skin like traditional bath soaps can. People often use bath oils and moisturising soap substitutes together. Take care when using bath oils as they can make the bath slippery which could lead to a fall. A rubber bath can help prevent this. Applying medicated topicals Medicated topicals contain drugs such as antibiotics, anti-fungals, and steroids etc. They come as creams, ointments, lotions and gels. They need to be applied thinly. If you apply too much, the patient could get an overdose of the drug which could cause side effects. Medicated topicals are often applied to a small patch of skin – wherever the problem is. The information leaflet inside should tell you exactly how much to apply. You’ll usually find a warning on the label that states ‘to be spread thinly’. A fingertip’s worth of medicated topical covers two hand’s worth of skin. 34 Fingertip units are there as a guide and are probably most useful for applying steroids (as they are often applied over larger areas of skin). When we say apply thinly, this means you should be able to see the skin through the topical product. There should be hardly any topical product visible on the surface of the skin. If you need to apply a nonmedicated topical and a medicated topical to the same patch of skin, which would you apply first? The most sensible advice is to apply the non-medicated topical first, then apply the medicated topical on top. This is because if you applied a lot of non-medicated topical on top of a little patch of medicated topical, you could end up washing the medicated topical off. Do I need to add topicals to the medicines chart? The care regulators recommend that all topicals (whether medicated or nonmedicated) should be added to the medicines chart (including moisturisers and bath oils). This is to show that they have been applied or used regularly. The only exception to this is moisturising creams used as soap substitutes. GUIDANCE Applying medicated patches Applying medicated patches Examples include nicotine, Fentanyl and glyceryl trinitrate patches. Some medicines can be given as a skin patch. These patches are like large sticking plasters, with the drug contained inside them. The drug absorbs through the skin straight into the bloodstream. Patches can be applied to various parts of the body. Exactly where depends on the type of drug contained in the patch (this will be explained on the leaflet inside the box). Usual places include: 4 4 4 4 Back Stomach Top of the arms Thighs Places to avoid sticking patches include: 6 Very hairy skin 6 Oily skin 6 Sunburned skin 6 Scarred skin 6 Rough skin 6 Damaged skin 6 Areas that get sweaty – e.g. underarms 6 Places where the patch could get rubbed off – e.g. under bra strap, on the waist 6 Bony areas – e.g. shoulders or hips The area of the skin where the patch will be applied needs to be clean and dry. You may need to wash off any moisturiser or body lotion that the patient has used, and pat the area dry first of all. Peel off the backing paper and stick the patch onto the skin. Press the patch on firmly so it sticks well, especially around the edges. So long as you are careful and avoid touching the sticky side, you wouldn’t necessarily need to wear gloves when applying patches. Some patches are only worn during the day; some are also worn at night. Some patches are kept on for as long as three days. Check to see what the instructions say. Some people write the date when the patch was applied onto the actual patch itself to remind them when a new one is needed. Remove the previous patch before applying a new one. Fold the old patch in half, sticking it to itself before discarding it. When applying a new patch, stick it near to where the last one was, but not directly over the same patch of skin. This prevents the same patch of skin getting irritated. 35 chapter 10 Administering inhaled medicines Inhalers are given to patients suffering from lung diseases – the two most common ones you’ll see are asthma and COPD (chronic obstructive pulmonary disease). Asthma is called a variable and reversible condition which means the symptoms can come and go; it is often caused by allergies. COPD is called a ‘fixed’ disease which means it doesn’t tend to get better. Relievers Everyone with asthma should have a reliever inhaler (usually blue). The most common reliever drug is salbutamol. Relievers don’t reduce the inflammation and mucus, they just open the narrowed bronchioles quickly (within a few minutes) making it easier to breathe. Salbutamol inhalers normally last about four hours. With asthma, relievers should be used when the patient either gets symptoms or expects them to come (i.e. before exercise or being exposed to anything that triggers their asthma). Side-effects include a slight tremor in the hands – this isn’t normally anything to worry about. It’s important patients are able to self medicate with their relievers, as you might not be around when they get symptoms. Assuming the patient has a good technique with their reliever inhaler but still 36 needs it frequently, the next step is to add a preventer inhaler. If a patient needs to use their reliever inhaler more than three times a week, they may need an asthma review. Preventers Preventer inhalers contain steroids (the most common being beclometasone). Steroids reduce inflammation and mucus, and makes the lungs less sensitive to triggers so the patient is less likely to suffer an asthma attack. Preventers are brown, orange or burgundy. Light brown inhalers contain less steroid; darker brown, orange and burgundy inhalers contain higher doses. In asthma, preventers are added when patients: + Cough, or have chest tightness or breathing difficulties more than three times a week + Need to use their reliever inhaler more than three times a week + Get breathless because of a chest infection or smoky atmosphere It is important patients use their preventers regularly, once or twice a day. Preventers take up to 14 days to work fully, hence they are taken every day even if the patient feels well. Forgetting the occasional dose won’t usually bring symptoms back straight away, but forgetting doses for several days can cause symptoms to return and make their asthma more unstable. Many people rely on their relievers too much and don’t use their preventers regularly. This is often because they feel an immediate effect from their reliever, whilst their preventer takes longer to work. However, this isn’t good for their asthma. Relievers don’t treat the underlying symptoms, so their asthma can become unstable and worsen. If patients have frequent symptoms and aren’t getting the right treatment, they can end up in hospital with a serious asthma attack. exampleS Relievers Preventers People worry about side effects with steroids. However, preventers only have small amounts of steroid in them and if they are used properly, it’s unlikely patients will suffer serious side effects. One side effect with steroids is thrush (a yeast infection) in the mouth. If a patient using steroid preventer inhalers has a sore mouth or throat, the doctor can prescribe something to treat it. To reduce the risk of thrush, patients must rinse their mouth out with water (and spit the water out) after using their preventer inhaler. Alternatively, they can brush their teeth after using their preventer inhaler. A spacer device can also reduce the build-up of steroid in the mouth to prevent thrush and other side effects. 37 exampleS Protectors Combination inhaler Protectors If reliever and preventer inhalers are still not controlling the asthma, the next step is to add a third inhaler called a protector. Protector inhalers are usually green or turquoise. These are basically long-acting reliever drugs. They act for around 12 hours so are usually prescribed twice a day. In asthma, it is very important that patients continue to use their steroid inhalers even if they have also been prescribed a protector. If they stop using their preventer and just rely on the protector inhaler, it can make their asthma very unstable and lead to a lifethreatening asthma attack. Combination inhalers Combination inhalers contain a protector and a preventer. Combination inhalers should be taken regularly: once or twice daily. They are usually purple, red or white. How do the treatments for COPD differ from asthma? Just like with asthma, everyone with COPD needs a short-acting reliever inhaler. However, the relievers are often prescribed on a regular basis rather than ‘when required’. Instead of adding a preventer next, prescribers tend to add a protector instead. If the relievers and protectors aren’t enough, then preventers are added. Preventers are used last because they are less effective in COPD (as there is less inflammation present than with asthma). Patients with COPD can have another type of inhaler called an ‘anticholinergic’. Examples include Atrovent (contains ipratropium) and Spiriva (contains tiotropium). The various different models of inhaler There are many different inhaler devices used to deliver the drugs we’ve looked at. Asthma UK has produced an animated guide showing how to use these at www. asthma.org.uk. The patient information leaflet should also show the patient how to use their inhaler device. If the patient self administers inhalers, check that they are using them correctly. If you see mist coming from the top of the inhaler or their mouth, they won’t be getting much benefit from it. You could always suggest they see a health care professional who can review their treatment. 38 exampleS Spacer Aerochamber Spacer with face mask Spacer devices Taking care of spacer devices A spacer is a plastic container that is added to a standard inhaler. There are many different designs, including smaller ones such as the Aerochamber Plus or larger spacers such as the Volumatic. Aerochambers have a soft rubber end so they can fit different types of inhaler, whereas Volumatics can only fit inhalers with a square mouthpiece. Spacer devices should be cleaned regularly by washing them in soapy water. After you have given the spacer a good clean, rinse the soap off the outside of the spacer, but leave the soap bubbles on the inside. When the spacer is dry, the bubbles will have burst leaving an invisible coating of soap on the inside of the spacer. This reduces static build up so less of the drug mist sticks to the sides of the spacer and more of the drug reaches the lungs. Don’t dry the spacer with a towel or tissue, as the rubbing action adds static. Volumatics need to be washed once a month and Aerochambers every 1-2 weeks. If used regularly, spacer devices should be replaced every 6-12 months. Aerochambers also have a whistle on them to let you know if the patient is breathing in too fast. It’s okay to hear a quiet whistle, not a loud one. If the whistle is loud, ask the patient to try again with a gentler in-breath. It’s not a good idea to change the type of spacer without checking with the prescriber. Most spacer devices also have a version with a soft silicon face mask. Patients who are unable to form a good seal around the mouthpiece (which can sometimes happen after a stroke) might benefit from a face mask. Patients who keep breathing through their nose might also benefit from a mask. With spacers, there are two techniques: 1 Taking in one long breath from the spacer device and holding it for 10 seconds or 2 Taking 5 breaths in and out from the spacer device (called tidal breathing) Both techniques are effective but patients often prefer the second technique as some find it difficult holding their breath. 39 GUIDANCE Administering an inhaler with a spacer deviCE 1 Remove the lid. Check there are no foreign objects inside the mouthpiece 2 T est the inhaler. If it hasn’t been used for 7 days shake it and then spray two puffs into the air; this ensures the patient gets a full dose of the drug 3 Insert the inhaler into the spacer. If you are using an Aerochamber, you might need to twist the rubber end around (where the inhaler fits into the spacer) so that the inhaler is pointing upwards at 12 o’clock 4 Shake the inhaler whilst it is in the spacer, 4 or 5 times 5 T he patient should be sat up straight or standing. Where possible, their chin should be lifted up to open the airways. This is the ideal position, but might not be possible with some patients with a physical disability 6 E stablish which technique the patient prefers: taking in one breath and holding it for 10 seconds or taking 5 breaths in and out. It’s a good idea to record which technique they prefer on the medicines chart 7 P ut the spacer in their mouth and check their lips form a tight seal. Check that they are breathing through the spacer device correctly before you fire a puff in (if you are using an Aerochamber, you shouldn’t hear a loud whistle). Make sure they are breathing through their mouth rather than their nose 40 8 If the patient cannot form a good seal with their lips around the spacer, they may need to use a spacer with a mask attached instead. Make sure that the spacer is level (horizontal) otherwise they might not receive a full dose 9 H olding breath technique: get the patient to blow out into the spacer device which empties their lungs. Tell them to take a slow, deep breath in. As they breathe in, fire a puff into the spacer. Encourage them to carry on breathing in. Keep the spacer in their mouth as they breathe in. Once they have breathed in fully, take the spacer out and ask them to hold their breath for as long as is comfortable (10 seconds if possible) 9 Breaths in and out technique: as the patient is breathing in and out, fire in one puff. Keep the spacer in their mouth for 5 breaths in and out. You can always help the patient by breathing in and out 5 times with them. This can help some patients with dementia or learning disabilities understand what to do. When you do this, the patient often copies your own breathing pattern. This also means that you can count your own breaths rather than trying to see if the patient is breathing in and out 5 times 10 If a second puff is needed, wait 30 seconds then repeat the whole procedure. Don’t put more than one puff into the spacer at a time, as the droplets can end up joining together to form larger droplets which cannot get deep into the lungs, and so reduces the amount of drug you are helping to administer 11 R eplace the mouthpiece and record on the medicines chart. If using a preventer, ensure the patient rinses their mouth out with water (rinse, gargle and spit) or cleans their teeth afterwards 41 Chapter 11 Administering medication to the eye, ear & nose Medicines can be applied to the eye, ear and nose in the form of drops, creams, gels, ointments and sprays. According to the care regulators, care professionals can administer these types of medicines after their ‘basic medicines training’ (i.e. you don’t need to have a registered health professional provide personalised training). However having said this, some employers have stricter policies than this. Check your medication policy to see if your employer lets you administer medications to the eye, ear or nose. If patients have had a recent eye operation (such as having cataracts removed) some employers will not allow care workers to administer eye drops, insisting instead that nurses do this. This is because there is a higher risk of getting eye infections after surgery and nurses are trained to pick up the signs and symptoms of eye infections. Eye drops There are many different ways of administering eye drops, the most important thing is to get a drop into the patient’s eye in a way that doesn’t cause them discomfort. Some patients will sit patiently and let you administer eye drops and are usually patients who have had them before. They may have had conditions like glaucoma or dry eyes. There will also be those patients who have not had eye drops before and may find it harder to keep their eyes open as you put drops in. 42 Many people stand above the patient and let the drop fall onto the eyeball. If this technique works for you and the patient, carry on. However this can be uncomfortable for patients. It also makes them more likely to blink, as they see the drop hanging above their eye. Older patients and those in highbacked wheelchairs may also find it difficult tipping their head back. An alternative used by many opticians, is to place the drop onto the lower eyelid whilst the patient looks away. By touching the drop against the lower lid, it gets ‘sucked’ into the eye. You only need to touch the drop on the lower lid, not the bottle tip. Some people worry that bacteria will be transferred onto the tip of the bottle it touches the lower lid. However, the drops are only used for 28 days; they contain preservative and are not swapped between patients so this shouldn’t be a problem. GUIDANCE Lower eyelid application Administering eye ointments With eye ointments you can use the same technique. You need to squeeze about 1cm of ointment inside the lower eyelid. The ointments can make the vision blurred as they can be quite greasy. Administering eye drops to patients who find it hard to keep their eyes open Despite your best efforts, some patients might find it hard to keep their eyes open as you administer drops. There is another technique you can use. Have the patient lie on their back and close their eyes. Gently place a few drops (3 or 4) into the eye socket near the side of the nose. Make sure the drops run along the eyelashes. Next, ask the patient to open their eye(s), you might need to help them do this. The drops will then enter their eye(s). Wipe away any excess drops with a clean tissue. Remember, the eye will only retain what it needs (about one drop). The patient will need to then close their eyes for about 30 seconds for the drop to absorb. exampleS Eye drops Eye ointments If a second type of eye drop or ointment is needed afterwards Some patients have more than one type of medication administered to the same eye. Wait 3 or 4 minutes for the first drop to absorb before administering another eye drop. If you have to administer an eye ointment and a drop to the same eye, it’s best to administer the drop first, wait 3 or 4 minutes, then administer the ointment afterwards. If you try administering an eye drop after an eye ointment, the drop will find it hard to absorb through the greasy ointment. Some eye preparations can sting (e.g.pilocarpine). If these are needed with other drops, then administer the pilocarpine afterwards, because the patient will find it hard to keep their eyes open if they sting. If an ointment is then needed, wait for the stinging to stop before administering the ointment last of all. 43 GUIDANCE The technique of administering eye drops Get ready: Check the drops haven’t passed their expiry date. When breaking the seal on new drops, write the expiry date on the bottle (28 days) Prepare the patient: The patient can be sat upright in a chair. They do not necessarily need to tip their head back with this technique Prepare the right dose of medication: Wash your hands, shake the bottle, unscrew the lid and put it somewhere clean. Gloves are not always needed when administering drops Administer the medication: Push out a drop and leave it hanging from the tip of the dropper bottle. With your free hand, pull the lower lid down gently away from the eyeball to make a pocket in which you can place the drop. Tell the patient to look towards the bridge of their nose and then upwards. Looking up takes the upper eyelid and lashes out of the way and gives you more room to put the drop in. Gently touch the drop onto the lower lid to release it. Don’t worry if you accidently put more than one drop in the eye – the eye can only hold onto one drop, so any others will flow away harmlessly down the cheek Give the patient a clean tissue to wipe away any excess. Once you’ve put in the drops, tell the patient to close their eyes for about 30 seconds. This spreads the drops over the eyeball. Check for any redness, pain, itching or swelling in the eye – a little stinging and itching is okay as long as it’s not too uncomfortable administering nasal drops Get ready: Check the drops haven’t passed their expiry date. When breaking the seal on new drops, write the expiry date on the bottle (28 days) Prepare the patient: The patient can either lie, or sit down with their head tilted backwards. If the patient lies down, put a pillow under their shoulders. This way their head tilts back a little, over the edge of the pillow 44 Prepare the right dose of medication: Wash your hands, shake the bottle and unscrew the lid Administer the medication: Hold the dropper just above the patient’s nostril and gently squeeze a drop down the centre of the nostril (you can make the nostril a little wider by pressing your thumb against the tip of the nose, which opens them up) Ask the patient to inhale slowly and deeply through the nose, hold their breath for several seconds, then breathe out slowly. All the while they should stay with their head back, or lying down for one minute. This lets the drops soak in. If you’ve used a dropper, squirt out any medication left in the dropper into a clean tissue before putting the dropper back in the bottle. Administering ear drops Get ready: Check the drops haven’t passed their expiry date. When breaking the seal on new drops, write the expiry date on the bottle (28 days) Prepare the patient: Help the patient lie down on the bed, with the ear being treated uppermost. Alternatively, they can sit with their head tilted so that the treated ear is upright Prepare the right dose of medication: Wash your hands, shake the bottle and unscrew the lid Administer the medication: Pull the ear upward (away from the neck) and backwards a little (away from the face). This straightens the ear canal so that the drops flow right down into the ear where they need to work. Gently squeeze the correct number of drops down the side of the ear canal, not straight down the centre as they’ll hit the ear drum (which is loud and sometimes painful). Try not to let the dropper touch any part of the ear or ear canal. Ask the patient to stay lying or sitting, with their head tilted for about 5 minutes after you have instilled the medication (this allows the drops to soak in). Wipe away any drops that have dribbled down the neck with a clean tissue. If both ears need drops, wait for about 5 minutes for the first drop to absorb and then get the patient to turn over and repeat the procedure. 45 Chapter 12 Important medicines often taken by the elderly & how to administer Alendronic acid: used in treatment of osteoporosis Calcium supplements + This drug is usually taken only once a & keep bones strong. It is often taken in conjunction with Alendronic acid. + If on Alendronic acid do not take calcium on the same day as taking this. + Take calcium carbonate supplements with meals to assure high stomach acid for maximum absorption. + Taking calcium supplements in divided doses throughout the day is important if the total daily dose of calcium is 500g or more. + Avoid carbonated soft drinks and antacids containing aluminium as they can interfere with the absorption of calcium. week on the same day. + Taken about 30 minutes before breakfast (8am) + Swallow whole do not chew + Take with a full glass of water + Stand or sit upright for at least 30 minutes after swallowing the tablet and do not lie down until after you have eaten breakfast. + If a weekly dose is missed take the next morning and continue as normal. 46 + Calcium is an important element to build References The Royal Pharmaceutical Society of Great Britain ‘The Handling of Medicines in Social Care’ 2007 Care Quality Commission Outcome: Management of Medicines Commission for Social Care Inspection ‘Professional Advice: The Administration of Medicines in Care Homes’ Commission for Social Care Inspection ‘Professional Advice: Safe Management of CD’s in Care Homes’ Jan 2008 Peterborough Primary Care Trust oral administration guidelines for good practice and NOMAD system operating Patient.co.uk: How to use eye drops Asthma.org.uk: Using your inhaler British National Formulary MIMS Designed by cobalt id |cobaltid.co.uk Cover image by Andrzej Tokarski (fotoila.com) stowhealth.co.uk stowhealth Violet Hill House Violet Hill Road Stowmarket Suffolk IP14 1NL