* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download pediatric manual
Survey
Document related concepts
Transcript
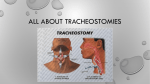
PEDIATRIC MANUAL © 2009 Breath of Life Home Medical Equipment and Respiratory Services GUIDELINES FOR CAREGIVER TRAINING Caregiver training will be divided into sections that will require successful completion of a section of training; the caregiver will continue to be involved, on a weekly basis, with the care of the child. The caregiver will complete each individual section of the training record with instruction from Breath of Life staff and then will return demonstrate each task without assistance and/or verbal cues from staff. The staff will be present at the bedside to observe. Section One: Caregiver will begin learning care Staff will be teaching trach care, trach changes, suctioning and manual resuscitation Caregiver will demonstrate 2 independent trach changes Caregiver will demonstrate 5 independent suctioning Caregiver will be required to do trach changes and suctioning on a weekly basis Child will have a cardiac apnea monitor and/or pulse oximeter on at all times Caregiver will be independent in use of manual resuscitator Section Two: Completion of section one CPR module Education will be started on the ventilator and the circuit Caregiver will be able to recognize signs and symptoms of respiratory distress after a discussion with the attending physician and/or staff member Caregiver will complete ventilator and/or CPAP training. Child will have a cardiac apnea monitor and/or pulse oximeter on at all times Section Three: Completion of section two Caregiver will review CPR Caregiver will independently change 2 circuits on ventilator. (No Cues) Caregiver will demonstrate getting the child and the equipment in and out of the car independently a minimum of one (1) time Caregiver will have completed all training records and have records signed Section Four: Caregiver will complete total independent care of their child as ordered by the attending physician Section Five: Completion of section four Caregiver will have a cardiac apnea monitor and/or a pulse oximeter on at all times I have read the above guidelines for the caregiver and understand that I will be required to participate with the Breath of Life staff to have training completed. Caregiver Signature:___________________________________ BOL Staff Signature:__________________________________ Date:______________________________ WHAT TO TAKE ON AN OUTING WITH A TRACHED CHILD YOUR TRAVEL BAG SHOULD INCLUDE: Trachs (Same size and emergency, ready to go) Syringe (if trach is cuffed) Scissors Water-based lubricant Normal saline Humidivents 2xs2 and 4x4 gauze sponges Suction catheters Ambu bag Portable suction List of emergency numbers Change for phone call/cell phone Gloves CHILDPROOFING YOUR HOME One of the most important steps you can take to protect the health and life of your child is to “childproof” your home. Perhaps the best way to do this is to take a “baby’s eye view”; crawling from room to room will help you spot the sharp corners, uncovered electrical wall outlets and extension cords, hanging cords to lamps and other appliances, and loose objects which might easily fall. The following is a quick checklist for childproofing each room in your house. Remember, however, that every child and home is different. Check your home carefully. NEVER LEAVE YOUR BABY UNATTENDED!!! Childproofing Baby’s Room 1. 2. 3. 4. 5. Hang mobiles and dangling toys out of reach so that baby can’t strangle on the string. The string should be no more than 12 inches long. Diaper pails can be dangerous to curious babies: many have drowned in the soaking pails. Keep the cover on the pail. The various baby powders and talcs can be dangerous. Never use them near a fan or allow the baby to play with the container-he/she could choke on the dust. Do not put plants in baby’s room if there is any chance the baby could reach them. Store ointments, creams, safety pins and other baby paraphernalia out of reach. Childproofing the Kitchen 1. Turn handles of all pots and pans to the back of the stove so that the baby can’t reach them. (The best way to avoid accidents is to keep your baby in his/her playpen or high chair while you cook) 2. Avoid using tablecloths that can be pulled down. 3. Keep all appliances and their cords away from the edges of counters or table tops. All cords should be coiled up and tied. 4. Place safety latches on kitchen cupboards. If you have room, you can let your baby have one cupboard of his own filled with pots, pans and large plastic bowls. 5. Cleaning products and all other toxic substances should be stored in a high cupboard with a lock or safety latch. You can begin to teach a 1 year-old the dangers of toxic substances by using “Mr. Yuck” stickers. For information on obtaining these stickers write the Institute of Education Communications, Children’s Hospital of Pittsburgh, Desoto Street, Pittsburgh, PA 15213. Note: Some groups have expressed concern that children do not get dependent on the Mr. Yuk stickers because it is impossible to put them on every toxic substance a child might find. Many parents take both approaches: they teach their child NOT to play with any bottles in cupboards and also use Mr. Yuk stickers. 6. Keep knives and all cutlery in a drawer or cupboard out of your baby’s reach. 7. Try to keep bits of food off the floor, especially food that your baby could choke on. 8. If you drop a glass on the floor and it breaks, protect your crawling baby’s hands and knees by first vacuuming and then using a wet paper towel to get any remaining silvers. 9. Whenever you are handling hot liquids, check to see where your baby is BEFORE you pick up the tea kettle or pan. You do not want to trip and spill boiling water on your baby. 10. Teach baby from the beginning that the stove is off limits whether it is off or on. 11. Jagged edges on boxes of aluminum foil or plastic wrap can cause cuts; keep them out of reach. Childproofing the Living Room 1. Plan on putting away all delicate, breakable, and valuable items from tables and shelves until your baby is well past the curious/destructive stage (4 to 5 years old) 2. Check the floor area daily for small objects that baby could choke on: pins, small bits of food such as popcorn, peanuts, etc 3. Tables with sharp corners and edges can be protected with rubber corner guards. 4. Bookcases are great attractions for young babies. Make sure they are fastened to the wall so your baby can’t pull a bookcase over on top of himself. 5. Cover unused electrical outlets with plastic caps. You can also obtain boxes that will cover outlets that are being used. Where possible, place furniture on front of outlets. 6. Never leave extension cords plugged in where your baby can find and chew on them and be seriously burned or shocked. Tape any excess cord down so baby won’t be so interested. 7. Heaters, whether electric space heaters or wood stoves, can present serious hazards to a young baby. Make sure heaters are well ventilated and are protected by safety guards. 8. Telephones are fascinating to curious babies-make sure the cords are out of reach, so that the baby doesn’t pull the phone down on his/her head. If your put the phone on the floor, try putting a wide rubber band over the switch hook points so the phone line is not on when the receiver is lifted. You can still receive calls while the baby plays, but you won’t have any unexpected long-distance phone bills. Childproofing the Bathroom The bathroom is especially dangerous because it usually contains medicines, drugs, and other potentials poisons. Keep all medications in a locked cabinet out of your child’s reach. Shampoo and soap should also be kept out of the child’s reach. Haridryers should always be kept unplugged to avoid electric shock if they should be pulled or dropped into water. To avoid burns, lower the thermostat on your hot water heater to 120 degrees Fahrenheit (48.9 degrees C) Always check the water before temperature before putting your child into the bath water or under a faucet. 5. Your child will find the wastebasket full of interesting things. Be aware of what you throw away and put pills, razor blades, etc. in a special wastebasket that is out of the child’s reach. 6. Children have drowned in toilet bowls-always leave the lid down. High rubber stops on the lids will prevent his/her fingers from getting caught if he should happen to lift and the drop the lid. 7. A hook on the outside of the bathroom door or a plastic door knob cover may be necessary to keep the door closed and the child out of the bathroom. 8. Use plastic or paper cups and containers in the bathroom so there is less chance of broken glass. CHOKING Description: Choking is the coughing spasm and sputtering that happen when liquids or solids get into the airway. (This is called aspiration) A child’s cough reflex will clear the windpipe of liquid within 10 to 30 seconds. Complete blockage occurs when solid food or a foreign object becomes lodged in the voice box. (It can also occur with severe croup) If this happens a child is unable to breathe, cry, or speak. The child will be in a state of panic, and if the obstruction isn’t removed in 1 or 2 minutes, the child will pass out. First Aid: 1. Call the rescue squad (911) immediately. In general, choking on liquids is temporary and harmless. Call 911 if your child chokes on a liquid and turns blue, becomes limp, or passes out. 2. Encourage coughing: As long as your child is breathing and coughing, do nothing except encourage him/her to cough the material up by him/her self. The main purpose of your child’s cough reflex is to clear the windpipe. Don’t give your child anything to drink because fluids may take up space needed for the passage of air. 3. Heimlich maneuver if a child over 1 year old stops breathing: If your child can’t breathe, cough or make a sound, proceed with high abdominal thrusts. Grasp your child from behind, just below the lower ribs but above the waist, in bear hug fashion. Give a sudden upward jerk at a 45 degree angle to try to squeeze all the air out of the chest and dislodge the object from the windpipe. Quickly repeat this upward abdominal thrust 10 times in a rapid succession. If your child is unable to stand and is too heavy for you to suspend from your arms, lay him/her on his/her back on the floor. Put your hands on both sides of the abdomen, just below the ribs, and apply sudden, strong bursts of upward pressure. 4. Back blows and chest compressions if a child under 1 year old stops breathing: If your infant can’t breathe or cough, place him/her face down over your knees or forearm (that is, use gravity to help propel the object) Then deliver 5 hard blows with the heel of your hand between the shoulder blades in rapid succession. (This is not helpful in older children) If the child does not start breathing again, lay your child on his/her back on the floor and apply 5 rapid chest compressions over the lower breast bone (sternum) using two fingers. 5. Resuscitation if your child passes out from choking: The rescue squad should be on its way. Quickly open your child’s mouth and look inside with a light to see if there is an object that can be removed with your fingers or tweezers (usually there is not). DO NOT put your fingers into your child’s mouth unless you already see the object. Doing this blindly can wedge an object deeper into the voice box (larynx). If you know how, begin mouth-to-mouth resuscitation. Air can usually be forced past the foreign object. If mouth-to-mouth breathing doesn’t move the chest, repeat the abdominal thrusts (if over 1 year old) or chest compressions (if under 1 year old). Prevention: Choking can be life-threatening, so try to prevent it from happening again by not giving young children foods or small objects that are most likely to cause choking. Foods that are most likely to cause choking are nuts of any kind, sunflower seeds, orange seeds, cherry pits, watermelon seeds, gum, hard candies, popcorn, raw carrots, raw peas, raw celery, and tough meats. Do not give these hard foods to children who are less than 4 years old. They do not have enough molar teeth to chew them well and they may not understand that some seeds should be spat out rather than swallowed. The soft foods that most often cause fatal choking are hot dogs, sausages, and grapes. These foods must be chopped up before serving. Warn baby-sitters and older siblings not to share these foods. Choking on a rubber balloon is the leading cause of deaths resulting from choking on objects other than foods. Most incidents occur when children suddenly inhale a deflated balloon they have been chewing. Warn your child to never chew or suck on pieces of rubber balloons. Even teenagers have died from this freak accident. Chewing on an inflated balloon is also dangerous because it could burst. Mylar helium balloons are safer, but rubber balloons are fine if they are used with supervision. Written by B.D Schmitt, M. D. author of “Your Child’s Health,” Bantam Books. Published by Clinical reference Systems, a division of HBO & Company HINTS FOR DAILY LIVING WITH A TRACHED CHILD Bathing: Baths are all right if the water is shallow, the child is watched, and the tracheostomy is covered by an artificial nose or ventilator tubing remains connected. Showers should only be the hand-held type. Playing: No contact sports No playing in and around a sandbox o Limit outdoor play on windy days. Place an artificial nose and a scarf or mask over the tracheostomy to keep dust or cold air out. Household Safety: Limit irritating substances; perfumes, sprays, powder, and smoke. Keep house clean; try to eliminate dust and molds. Pets and birds may cause serious respiratory problems. Dogs and cats shed, and hair may get into the trach tube. Decannulation Decannulation: When the trach tube comes out accidentally. Always keep a spare trach tube readily available. Also keep an “EMERGENCY” one that is a half size smaller that the current trach, in case the usual size cannot be inserted. Don’t panic; the child can breathe through the stoma for a short time. Secure the stoma with the nondominant hand. Insert the new trach tube and secure. (Some bleeding may be observed due to trauma of decannulation) If same size trach tube cannot be inserted, use the “EMERGENCY” trach. If you are unable to insert the “EMERGENCY” trach tube, cover the stoma with a clean gloved finger and use the ambu mask placed over the child’s mouth and breathe for the child using the ambu bag. This is an emeregent situation, doctor notified. 911should be called and the Hand Washing Hand washing, when done correctly, is the most important method of preventing the spread of illness and disease. Any type of soap may be used, but antibacterial pump soap is the best Steps to take when washing hands thoroughly before and after contact with the child: 1. Wet hands and wrist thoroughly with warm water 2. Apply soap generously to hands and work up a soapy lather 3. Wash hands vigorously for 10-15 seconds (Sing the Happy Birthday Song twice to yourself while you wash is typically long enough) 4. Rinse with clean warm water with wrists down 5. Dry hands with clean paper towel, and then use the paper towel to turn off the water. Tips: When soap and water are not available or between washings, you can also use antimicrobial gel such as Purell to keep hands clean Apply lotion liberally, especially during the winter to protect hands and prevent chapping Keep nails clean, trimmed and without polish (polish can chip) HINTS FOR DAILY LIVING WITH A TRACHED CHILD Feeding and Drinking: Keep tracheostomy covered during feeding with the thermovent or trach collar; if the child is not on the ventilator. Do not prop a bottle, as the child may aspirate from liquid getting into the trach tube. Watch toddlers to prevent them from putting food or other objects into the tracheostomy. If the child begins to vomit, immediately turn the child’s head to the side to avoid aspiration and tracheal occlusion. If the child is suspected of aspirating, suction immediately and check the secretions for food particles. Water Play: No swimming, as the risk is too great of getting water in the tracheostomy. There is a risk of aspiration, be watchful when playing in water such as a sprinkler. HOME NEBULIZER TREATMENTS Many medications are most effective when inhaled directly into lungs. To be inhaled into the airways of the lungs, medication must be changed from a liquid to a fine mist. To create this fine mist at home, you need a nebulizer and an air compressor. A nebulizer is a plastic container that changes liquids into a fine mist using a jet of air. The compressor, runs by electricity or battery, provides the jet of air to the nebulizer. How is the home nebulizer used? 1. Place the compressor on a hard surface. Make sure the filter is free of dust and dirt. If it is dirty, rinse it with water and then dry it. Plug in the compressor. 2. Place the prescribed amount of medication(s) into the nebulizer with a dropper or a syringe. Two medications can usually be mixed together. If you have any questions please contact your physican or Breath of Life. 3. Some asthma medicines come premixed with saline. Other medications need saline added. You can buy sterile normal saline in two ways: in unit dose plastic vials or a pressurized canister (Bronchosaline). Two squirts from the canister should be enough. Never put a homemade saline solution into a nebulizer. 4. Attach the nebulizer to the compressor tubing. Turn the power on. (The medication will immediately begin to nebulizer) Place the mouthpiece in the mouth and breathe in and out slowly through the mouth until the medication is gone. If the child is able, tell the child to take an extra deep breath every 10 breaths or so, hold that breath for 10 seconds, and then breathe out slowly. This technique permits the medication to stay in the lungs longer for better effect. If a child is too young to use a mouthpiece, use a mask. The mask can be secured loosely over the nose and mouth so the child does not become frightened. Most nebulizers must be held in an upright position to work well. If the mixture has coated the sided and isn’t being nebulized, gently shake the nebulizer occasionally during the treatment. An average treatment takes 10-15 minutes. The treatment is over when all the medication is gone and the nebulizer makes a constant sputtering noise. Some children cough up mucus after breathing treatments. Observe the mucus color and thickness. Normal secretions are usually thin and white or clear. Thick and sticky mucus that is yellow or green may indicate an infection. Call your physician to report a change. If your child needs more treatments than prescribed by your doctor, or if the treatments do not improve the symptoms, call your physician. How and When Should the Nebulizer be Cleaned? After each treatment rinse the nebulizer, mouthpiece or mask, and T-piece under hot running water. Shake off excess water, place the pieces face down, and let them air dry. Store the pieces in a clean bag. It is not necessary to clean the compressor tubing. If you use the nebulizer frequently, you should clean it about 3 times a week. Wash your hands before handling the nebulizer. 1. Soak the nebulizer, mouthpiece, and measuring devices in warm water with a mild liquid detergent. If you are using a mask, wipe down the inside and outside of the mask with a paper towel mixed in the detergent solution. 2. Rinse each piece thoroughly in clean, warm running water. 3. Soak all the pieces for 20 minutes in a freshly prepared solution of 1 part vinegar and 8 parts water. 4. Remove the pieces from the vinegar and water solution and rinse them thoroughly again in clean, warm running water. 5. Shake off any moisture and allow them to air dry on a clean towel. When the pieces are completely dry, store them in a sealed plastic bag. Special Instructions: Your physician has prescribed nebulizer treatments to be given ____________ times a day. The medications to be used are ______________________________________________________________________________ ______________________________________________________________________________ HOME SAFETY Power Outage Tips: The electric and utility companies must be notified of equipment. These companies are to provide advance notice in case of a planned outage and are to contact the families as soon as possible in the event of an unplanned power failure. In any event, the following steps need to be taken: 1. 2. 3. 4. Use battery-powered lights. Use backup marine batteries for life support equipment. Follow the manufacturer’s guidelines for respiratory equipment. Activate any backup generators. Obtain a generator from the local fire department if the patient does not have one and is on life support equipment. 5. Check the circuit breaker or fuse box; reset the breaker or replace fuses as needed. 6. If a power outage source cannot be identified, or if it may take an extended period of time to resume power, arrange for the patient to be transported to the nearest location for emergency power, such as a local fire station or nearest hospital. HUMIDIVENT OR “ARTIFICIAL NOSE” Purpose: To provide humidification for the respiratory system, to assist in keeping secretions manageable, and to prevent airway damage due to dryness. When to use a humidivent: When your child is disconnected from bedside, water humidity source. How to use: The humidivent is placed between the trach tube under the child’s chin and the ventilator tubing attachment. If your child has a trach, but not a ventilator, the humidivent sits directly on the trach opening. How it works: There is moisture in our exhaled air. The tiny, rolled fiber inside the humidivent collects the moisture from your child’s exhaled air, holds it in the paper, and uses that moisture to humidify the next breath taken in. NOTE: The humidivent helps add moisture to each inhaled breath, but doesn’t do as thorough a job as the heated humidifier used at your child’s bedside. If your child will be away from the bedside humidification system for several hours, or the air is particularly dry, it may be helpful to place three or four drops of normal saline on the rolled fiber areas of the humidivent. REMEMBER: The humidivent is disposable and is not to be cleaned. For infection control purposes, it would be wise to discard the used humidivent daily. If the inside of the humidivent is saturated with secretions, discard it and use a new humidivent. Information Physicians to contact for trach care: Trach care frequency:_____________________ Trach Size: ___________________________ Suction frequency: _____________ Trach Type: __________________________ Size of suction catheter: _________ Cuffed: ________ Uncuffed: ___________ Size of emergency trach:_________ Other:___________________________________ Type of emergency trach:_________ Trach change frequency:______________________________ When last changed:_______________________________ Other Instructions:______________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ LAY PERSON CPR ON CHILDREN What is child CPR? CPR is also called cardiopulmonary resuscitation. CPR is used when a child is found not breathing and his/her heart has stopped beating. CPR may be able to start their breathing and heart beating again. If CPR is started early and done correctly, you may be able to save a child from dying. Child CPR should be used on children from 1-88 years old. Rescue breathing is done whan a child is not breathing but the heart is still beating. By breathing for the child, you may deep him/her alive. Rescue breathing may m be done by itself, or with chest compressions. When res rescue cue breathing and CPR are done together, it is called CPR. What is the cardiopulmonary system? The heart, blood vessels, and lungs make up the cardiopulmonary systems. The heart is in the middle of the chest between the spine (backbone) and the sternum (breastbone). The two lungs are inside to the right and left sides of the chest. The job of the heart is to pump blood to the lungs and then out to the body. The lungs put oxygen into the blood to feed muscles, bones and tissues of the body. Blood vessels called arteries and veins carry the blood throughout the body. Without oxygen, organs, muscles, bones and tissues will die within a short time. Why would a child need CPR? The main reasons that a child may stop breathing and his/her heart stop beating are the following • Blocked airway – This could be by the tongue, food or a small object • Cardiac arrest – The heart stops • Drowning • Infection • Injuries – Such as from falling or burns • Pneumonia • Poisioning ng What can I do to help prevent cardiac arrest and injuries in children? • • • • • • • • • • Do not leave plastic bags around that your child could put over his/her head Do not leave your child alone in or near water Do not leave small objects around that your child can pick up and put in his/her mouth. A good rule to follow is to not allow your child to play with anything small enough to fit through a toilet paper roll If you must keep guns in the house, put them out of your child’s reach. All guns should have a safety lock on them, be locked up out of reach of our child, and kept unloaded Keep cleaning supplies and other harmful products out of your child’s reach and locked up tightly Keep your child secured in a car safety seat while driving. Never leave your child in a care alone, especially not when the windows are rolled up Never drive in a car with your child if you have been drinking alcohol. Or if you have taken illegal drugs or medications that make you sleepy Watch your child carefully in the kitchen and around hot objects or machinery Watch your child if he is playing on or around anything from which he may fall What do I do first when I find a child that looks to be not breathing, or heart is not beating? • • • • Make sure the area is safe for you to enter Find out if the child is OK. Do this by tapping the child. Shout very loudly “Are you OK?” If the child does not respond, send someone to call 911 for help. If you are alone, begin the steps of CPR and do them for 1 minute. After 1 minute, call 911 yourself. The sooner caregivers arrive, the greater the chance the child will live. Stay on the phone with the 911 operator until you are told to hang up. Make sure the 911 operator is told the following important information: Where you are, including the address and the cross streets or roads. This will help EMS find you quickly The telephone number from where you are calling What happened, such as the child stopped breathing or was found under water If there are other injuries that you can see, such as bleeding from the head What help has been given to the sick or injured child so far How do I give a child rescue breathing or CPR? • By following the “ABC’s”, you can remember the steps to use when giving CPR. The letter A stands for airway, B stands for breathing, and C stands for circulation. Airway: • • • If you suspect broken arms, legs or back do not move the child. Moving a child with a broken neck or back could cause them to become paralyzed. If you don’t see other injuries, turn the child onto their back while supporting the head. The child should be face up on a firm, flat surface. The child’s head must be on the same level or lower than his/her heart. Check if the child has an open airway. Kneel beside the child and open the airway by gently tilting the head back and lifting the chin. Never lift under a child’s neck to tilt their head. Look into the child’s mouth and check if anything is blocking the airway. This may be food or a small toy. If you see something, scoop it out with your finger. If you thing the child may have a head or neck injury, lift the jaw forward instead of tilting the head. This should open the airway. Breathing: • • • • • Check if the child is breathing. Look at the child’s chest and belly to see if it goes up and down with breathing. Take 5 or 10 seconds to look, listen and feel, even if you are nervous and anxious. Feel for breathing by putting your face close to the child’s face. Put your hand lightly on the child’s chest to feel for chest movement. Make sure the airway is open, and listen and feel for air coming out of the mouth or nose. If the child is breathing on his own, and there are no injuries to the head or neck, turn the child on his/her side. This is called the recovery position and is used to prevent choking if the child throws up. Wait for EMS help to arrive. If there is no breathing, you must breathe for the child. This is called rescue breathing. Keep the airway open my having the head tilted and the chin slightly lifted by keeping one hand on the child’s forehead. Gently pinch the child’s nose with one hand. This keeps air from escaping from the nose. Take a deep breath for yourself and place your lips over the mouth of the child. Try to make an airtight seal with your mouth. Give two slow breaths (1-1/2 seconds per breath). Make sure you take a breath for yourself after giving each breath. If you don’t see the child’s chest rising with each breath, the airway may not be open. Gently move the child’s head to open the airway and try again to breathe for him. Any time you see that air is not going in (the chest is not rising with your breaths), check for something that may be blocking the airway. If you see something, scoop it out with your finger. Circulation: • • • • • • • • • • Check for signs of blood and oxygen circulation in the child. Signs of circulation are breathing (not gasping), coughing or movement after you do rescue breathing. Put your ear next to the child’s mouth and look, listen and feel for breathing. Look for other movement from the child. If the child is not breathing, coughing, or moving, you should immediately begin chest compressions. Chest compressions are when you put pressure on and off the chest with your hand. These compressions press the heart between the spine (backbone) and sternum (breastbone). This forces blood from the heart and into the rest of the body. To find the right place to do compressions, put the fingers of the hand furthest away from the head of the child on the child’s lower rib cage. Move the fingers up the rib cage to the place where the ribs meet in the middle of the chest. This is the sternum. Place the heel of one of your hands on the sternum right above where your fingers just were. Your hand should be on the lower part of the sternum. Correct hand positioning for chest compressions is important because ribs connect to the sternum. Incorrect hand placement can break the ribs during compressions. Getting up on your knees, position your body right over the child, not to the side. With the heel of one hand, press straight down on the child’s chest, 1 inch to 11/2 inches in depth. This should be about one third the depth of the child’s chest. Try to keep your arm straight when doing chest compressions. Look down at your hand. You should give compressions at a rate of 100 per minute. Do the compressions in a smooth, equal way. Do not lift your hand off the child’s chest between compressions. But do not leave pressure on the chest between compressions. This lets the heart fill back up with blood. Keep your other hand on the child’s forehead. After giving 30 compressions, make sure the airway is open and pinch the child’s nose. Give two slow rescue breaths to the child. Continue with cycles of 30 compressions followed by two breaths. Check the child’s circulation after one minute of CPR. Check for normal breathing, coughing or movement. With your ear next to the child’s mouth, look, listen and feel for breathing. If no one has called 911, if the child is not breathing, coughing, or moving continue cycles of 30 compressions, followed by two breaths. Checking for breathing and signs of circulation every few minutes until help arrives. If there are signs of circulation, but you do not see or feel breathing, do rescue breathing as outlined in the steps above. You should give 1 breath every 3 seconds when you do rescue breathing. In this case, do not do chest compressions, but continue breathing for the child. • If the child is breathing normally, moving, or coughing, this means they are breathing and their heart is beating. If there are no signs of head or neck injury, turn the child on to his side and stay with him. Watch him carefully in case he stops breathing as you wait for help to arrive. If the child looks like he/she is getting worse, follow the ABC’s as described above. MANUAL VENTILATION Anytime you have a patient with a tracheostomy or compromised airway you may need to manually ventilate the patient. When performing this procedure, keep in mind these important steps: Always watch for CHEST RISE and FALL Time the breaths that you are delivering with the spontaneous breaths of the child. This will help eliminate any discomfort felt by the patient and any difficulty you may have with providing the patient with a breath. Do not hyperventilate the patient by bagging too fast. Hyperventilation will blow off the child’s CO2 which may cause them to faint When using a manual resuscitator it should be connected to 100% oxygen If the child’s lips and nail beds are turning blue (cyanotic) while you are manually ventilating, make sure you are connected to the oxygen. If the child is on CPAP or has any PEEP with the ventilator, make sure that it is also on the manual resuscitator and appropriately set. TRACHEOSTOMY What is a Tracheostomy? A tracheostomy is a surgical procedure that creates an opening in your child’s neck and windpipe (trachea). A tube is then placed in the opening to keep it open. The procedure helps get air to your child’s lungs. The term tracheostomy may be used to refer both to the procedure and to the opening created by the procedure. When is it Used? A tracheostomy may be done when your child has a problem with the airway. If the upper airway is blocked, a tracheostomy can bypass the blockage to provide airflow to the lungs. It is also used to provide oxygen to the lungs more efficiently and to clear secretions from the airway. Examples of when your child might need a tracheostomy include: The upper airway is blocked by swelling, a tumor, vocal cord problems, or a severe narrowing of the trachea. Your child will be on a breathing machine (ventilator) for a long time. Your child has had a traumatic injury and needs the airway to be protected. Your child has lots of secretions or too much saliva that he/she cannot get rid of and so he/she needs frequent suctioning of the airway. TRACH CARE The skin around a child’s tracheostomy needs special care. Secretions (mucus) from around the tracheosotmy tube or directly from the trachea can cause skin to become red and sore if allowed it remains on the skin too long. As much as possible, the skin should be kept clean and dry. Several times a day, you should clean the skin around the stoma. The solution used to clean the skin around the stoma will depend on the child’s orders. The method will vary from child to child, and you should follow the plan designed for each individual. Dip cotton-tipped applicator in half-strength hydrogen peroxide (hydrogen peroxide mixed with an equal amount of distilled water) Starting as close to the tracheostomy as possible, clean the skin by rolling a cotton tipped applicator away from the tracheostomy opening. Repeat with a newly moistened cotton-tipped applicator until all crusts and drainage have been removed. Using dry cotton-tipped applicator, dry the area thoroughly with the same motion. Avoid using baby oil, lotions, or ointments around the tracheostomy unless they are specifically ordered by the physician. If the child is having a lot of tracheal secretions, you may wish to place a dry trach sponge between the skin and the trach tube to absorb the secretions. The dressing may need to be changed frequently so that wet gauze does not sit on the skin for a long period. Make sure the dressing does not cover the tracheostomy opening, making it difficult for the child to breathe. TRACHEOSTOMY CARE: HUMIDIFYING AND SUCTIONING Why is Humidifying and Suctioning Important? When you breathe through your mouth and nose, air is naturally warmed, moistened, and cleaned. Air coming in from a tracheostomy (trach) tube does not get moistened and cleaned. When this cool, dry air comes into the tube, it causes the lungs to make more mucus. These thick mucus secretions can block the trach tube and make it hard for your child to breathe. Making sure your child gets the right amount of humidity and suctioning to clear secretions will decrease the risk of an emergency because the tube is blocked. Blockages can be very dangerous and stressful. Work with your healthcare provider to learn how to manage your child’s tracheostomy care and allow your child to have a normal, active life. Humidification: Humidification is very important for thinning secretions so they do not block the trach tube. Humidification is needed even in very damp climates, at least at first. Humidity in the lungs helps to protect the lining of the lung and keep secretions thin. How do I keep the air humidified? Air is humidified using a humidifier or an HME (heat moisture exchanger) at different times during the day. The humidifier is used at night and periodically during the day. The HME is a device that your child can wear during the day to help keep the air moist without having to be hooked up to the humidifier. Before your child is discharged from the hospital, your discharge planner or instructor should make arrangements with a medical supply company to get a humidifier, HME, and any other equipment you will need. Humidifier: Several different types of humidifiers are available. They all have a water reservoir, a connecting hose, and a collar that fastens around your child’s neck. The humidity keeps a pocket of moist air at the opening of the trach tube. This type of humidifier should be used at night and periodically during the day. You will need to clean and disinfect the humidifier at least once a week. The thickness of the secretions as well as changes in your child’s breathing rate and pattern will help you decide if your child needs to stay on the humidifier during the day. Faster breathing, a heavy cough and thicker secretions mean your child probably needs to use the humidifier. If these are not present, your child is probably ready for the HME (heat moisture exchanger) and normal activity. HME (Heat Moisture Exchanger): An HME is also known by other names including an artificial nose, filter, or T-piece. They come in different shapes and styles, but it is usually a T-shaped device with gauze in it. The HME fits onto the end of the trach tube and collects exhaled moisture to humidify the next breath. This device should be worn whenever your child is out of the home or when the child is awake and active and needs freedom from humidifying equipment. The goal is to use the HME when your child is awake and active. Then, use the humidifier during naps, meals, and at night to replenish the lost moisture in the lungs. Usually, a child with a new tracheostomy can start out wearing an HME for at least 1 hour at a time or 2 or 3 times a day. As long as the secretions do not get too thick and your child seems to handle the HME well, he can start wearing the HME for a longer amount of time. Even after a short break using the humidifier, your child will be ready to use the HME again and lead an active life. Disposable HME’s are meant for a single use and need to be thrown away when clogged with mucus. If too much mucus is a problem, a reusable HME (a plastic T-Piece with replaceable gauze) is a less expensive option. The plastic T-piece can be washed and disinfected many times, whereas the disposable HME’s cannot. You may find it helpful to use both types. For example, use a T-piece with guaze in the morning (until the amount of secretions goes down) and then use a disposable HME in the afternoon. If the child has been using the device for a long period of time, or if it is hot and dry or windy, a few drops of saline may be added to the guaze to replace the lost moisture. You can buy saline drops at your local drug store or pharmacy. If your child is drinking plenty of fluids and has been using the humidifier, no moistening of gauze in the HME is needed. The best way to judge how long your child can use an HME is to periodically suction the trach. If the secretions easily pass through the catheter, your child can wear the HME for a longer period of time. If secretions are sluggish through the catheter, your child may need a few drops of saline on the HME to replace the evaporated moisture. If secretions coat the outside of the catheter or clog it, your child may need to use the humidifier for at least ½ to 1 hour or need several drops of saline put into the trach tube, followed by suctioning until the secretions thin out Remember To: Check the HME gauze to be sure it doesn’t get covered over with secretions. Have your child drink plenty of fluid each day. Taking in plenty of fluid will help keep secretions thin. Suctioning: Suctioning is important to keep mucus from blocking the trach tube. When do I suction the tube? Suctioning should be done whenever it is needed. Signs that your child needs suctioning include: Gurgling or bubbly sounds Coughing Suctioning should also be done at the following set times: Before eating (waiting until after eating may lead to vomiting) Before and after sleeping (including naps) How often your child needs to be suctioned depends on the child’s age and the reason they needed a tracheostomy. A baby or toddler may need more frequent suctioning because of crying, a less efficient cough, and more frequent colds. An older child may need suctioning only occasionally when they are healthy and more often when he or she is sick. What equipment is needed? You will need the following: A suction machine with tubing A clean catheter Ambu bag Emergency trach How do I suction the tube? To suction the tube: 1. Wash your hands with soap and water and dry them well. 2. Pick up the catheter from the end that is attached to the suction machine. Do not pick up the end that will go into the trach tube. 3. Connect the catheter to the suction machine tubing and turn on the machine. 4. Insert the catheter into the trach tube. The catheter will follow the curve of the trach tube. Be sure you know how far the catheter should go in before you begin suctioning, usually the length of the trach tube plus ¼ inches. Stop the catheter at this point. 5. Apply suction by putting your thumb over the hole in the catheter back out. Gently roll the catheter back out. Gently roll the catheter between your thumb and forefinger as you pull the catheter out. Normal secretions are clear to white and are thin to slightly thick. If the secretions are very thick, you may need to suction a second time. Put several drops of saline (not plain sterile water) down the trach and suction again. Putting saline solution down the trach and suctioning will likely cause coughing and choking. This is normal and helps to loosen secretions. How do I clean the suctioning equipment? Rinse the catheter with sterile water and store it in a commercially made solution or a solution of vinegar (1 part white vinegar) and water (2 parts sterile water) The catheter suction machine, tubing, and any other parts that that have touched the secretions must be cleaned regularly. TRACHEOSTOMY CARE: WARNING SIGNS Warning signs of a blocked tracheostomy: There are warning signs that a child with a tracheostomy is having serious trouble breathing, the following are signs your child might have: Your child is unusually anxious and has a frightened look Your child is restless Your child has trouble eating Your child is breathing rapidly You hear a wheezing sound The nostrils flair with each breath The mouth, lips, or fingernails are pale bluish or dusky The hollow in the neck, the skin between the ribs and the skin under the breast bone may pull inwards with each breath. If you see any of these signs, immediately suction the trach tube. If the signs continue, change the trach tube and suction again. If the signs still persist after changing the tube call 911 right away. Warning Signs of Infection: Look carefully at secretions in the catheter for signs of infection. Call the doctor if the following occurs: The secretions become yellow or green, or if they have an unusual or bad smell. (The first 1 or 2 hours in the morning, the secretions may be yellowish, but they should soon become clear or white color) You see bright red blood in the secretions. (A few streaks of blood or faint pinkish tinge in the catheter may be normal following a trach tube change) Your child has a fever or is vomiting Warning Signs of Dehydration: Make sure your child has enough to drink each day so that secretions remain thin and do not block the trach tube. Your child will need to drink extra fluids when he or she is sick. Signs that your child may not be getting enough fluids include: Your child has stopped wetting his/her diapers or wetting a lot less Your child goes to the bathroom less than 3 times a day You notice a change in the color and smell of the urine. A darker color and strong ammonia smell are signs of dehydration.