* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
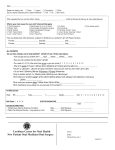
Download Co-Management Guide
Survey
Document related concepts
Transcript
GIMBEL EYE CENTRE Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Last revised May 2014 CALGARY: 403-286-3022 | Toll-free 1-800-661-1138 EDMONTON: 780-452-4111 | Toll-free 1-888-211-4822 gimbel.com Table of Contents If you are reading a digital format, you can click on the bolded headings to jump to that section of the guide. Introduction..........................................................................................................................................................................4 Meet our Doctors.................................................................................................................................................................5 Meet our Calgary Doctors.................................................................................................................................................5 Meet our Edmonton Doctors.............................................................................................................................................5 Contact Information............................................................................................................................................................6 The Role of the Co-Managing Eyecare Provider............................................................................................................7 Pre-Operative Evaluation...................................................................................................................................................7 Referrals to Gimbel Eye Centre.........................................................................................................................................7 Post-Operative Evaluations...............................................................................................................................................7 Corneal Refractive Surgery Descriptions........................................................................................................................8 IntraLase Laser Assisted In Situ Keratomileusis (IntraLASIK)...........................................................................................8 Photo Refractive Keratectomy (PRK)................................................................................................................................8 Photo Therapeutic Keratectomy (PTK)..............................................................................................................................8 Astigmatic Keratotomy (AK)..............................................................................................................................................8 KAMRA Inlay for Presbyopia..............................................................................................................................................8 Laser Technology and Wavefront Treatment.....................................................................................................................8 Corneal Refractive Surgery Patient Selection................................................................................................................9 Eligibility Criteria for Corneal Refractive Surgery...............................................................................................................9 Contraindications for Corneal Refractive Surgery...........................................................................................................10 Corneal Refractive Surgery Post Operative Care........................................................................................................11 Postoperative Medication and Follow Up Regimen........................................................................................................11 PRK Post-Operative Extended Medication Protocol.......................................................................................................12 Corneal Surgery Post Operative Presentation and Activity Restrictions.........................................................................13 Corneal Refractive Surgery Complications and Treatment.............................................................................................14 Phakic IOL Refractive Surgery Descriptions................................................................................................................16 Implantable Collamer Lenses (ICL).................................................................................................................................16 Angle Supported Phakic IOL (Cachet)............................................................................................................................16 gimbel.com | 2 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Phakic IOL Surgery Patient Selection............................................................................................................................17 Eligibility Criteria for Phakic IOL Surgery.........................................................................................................................17 Contraindications for Phakic IOL Surgery.......................................................................................................................17 Phakic IOL Postoperative Care.......................................................................................................................................18 Postoperative Medication and Follow Up Regimen........................................................................................................18 Phakic IOL Post Operative Presentation and Activity Restrictions..................................................................................19 Phakic IOL Postoperative Evaluation Considerations.....................................................................................................20 Phakic IOL Surgery Complications and Treatment.........................................................................................................21 Refractive Lens Exchange/Cataract Extraction Descriptions....................................................................................22 Surgery Description.........................................................................................................................................................22 Alberta Health Care (AHC) Covered Services.................................................................................................................22 Refractive Lens Exchange and Cataract Surgery Patient Selection.........................................................................23 Refractive Lens Exchange/Cataract Surgery Lifestyle Implant Choices.........................................................................24 Refractive Lens Exchange/Cataract Surgery Post Operative Care...........................................................................25 Refractive Lens Exchange and Cataract Surgery Post Operative Medications and Follow up......................................25 Refractive Lens Exchange and Cataract Surgery Post Operative Presentations and Activity Restrictions....................26 Refractive Lens Exchange/Cataract Surgery Complications and Treatment..................................................................27 Collagen Cross Linking Description..............................................................................................................................28 Accelerated Collagen Cross Linking Patient Selection..............................................................................................29 Presbyopia, Monovision and the Role of the Co-managing Doctor.........................................................................30 Special Considerations in Refractive Surgery.............................................................................................................31 Dry Eye Assessments and Treatment............................................................................................................................32 Fee Information.................................................................................................................................................................33 Frequently Asked Questions...........................................................................................................................................34 Forms..................................................................................................................................................................................35 Last Revised April 2014 3 | gimbel.com Introduction Dear Doctor, Welcome to our new and updated Co-management guide! Since 1964, Gimbel Eye Centre has been providing Refractive and Cataract surgical options in a convenient, compassionate, and caring manner to our mutual patients. As an established ophthalmic surgery practice, we pride ourselves in providing honest, high quality care and realize that our success lies in the company we keep. We are very aware that the relationship with our co-managing Doctors is an integral part of our success. As we are committed to reinforcing your role as the Primary Eye Care Provider, we provide the convenience of collecting your co-management fees at the time of their surgery payment, and then pass it along to you. This promotes patient compliance, and emphasizes the importance of the patient returning to you for proper follow up care and beyond. In recognizing that our Associated Eyecare Providers may have different practice needs, we can deduct from your patient’s surgery fees to enable you to charge your patient directly for follow up care based on your own fee schedule. Our goal with this new Co-management guide is to provide a concise, easy-to-reference resource to enable the busy practitioner to feel confident and up-to-date in our quickly evolving professions. Included are surgery descriptions, eligibility criteria, post-operative care, complication management, and fee structures. This resource is available in digital format and hard copy. In addition to the Co-management guide, Gimbel Eye Centre provides numerous other resources including YouTube videos with over 100 hours of intraocular surgery footage, our updated Website at www.gimbel.com, complimentary Continuing Education Seminars regarding a wide range of ophthalmic surgery topics, and periodic Webinars and Webcasts. We welcome an open dialogue with our team of surgeons, optometrists, and staff, to support both you and your patient in this important life experience. We would be pleased to have you visit our Calgary or Edmonton Centre, and perhaps observe a surgery or two! Thanks for sharing our vision of providing the best eye care solutions for our mutual patients. Sincerely, Gimbel Eye Centre Team gimbel.com | 4 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Meet our Doctors Meet our Calgary Doctors H.V. Gimbel, MD, MPH, FRCSC, AOE, FACS, CABES Executive Medical Director John van Westenbrugge, Marcella LaBelle BSc OD MD, FRCSC Associate Medical Director, Surgical Services Mona Purba BSc OD Leta Theissen BSc OD Meet our Edmonton Doctors Geoffrey B Kaye, MB, ChB. Nohad Teliani BSc OD FCS(SA), FRCSC Executive Medical Director, Gimbel Eye Centre, Edmonton Last Revised April 2014 5 | gimbel.com Contact Information Office Addresses Gimbel Eye Centre Gimbel Eye Centre CALGARY EDMONTON Market Mall Executive Professional Centre 450, 4935 - 40th Avenue NW Calgary, Alberta T3A 2N1 Mira Health Centre 140, 11910 - 111th Avenue Edmonton, Alberta T5G 0E5 Office Telephone Numbers Office Telephone Numbers (403) 286-3022 1 (800) 661-1138 (780) 452-4111 1 (888) 211-4822 Office Fax Numbers Office Fax Numbers (403) 286-2943 (780) 452-4114 Manager, Operations Manager, Operations Lynda Kelly, COMT Violet Wray, LPN Your Contact Person Glenn Gimbel, President (403) 202-3312 [email protected] gimbel.com | 6 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 The Role of the Co-Managing Eyecare Provider As the Primary Eyecare provider, your role is important in the patient’s Refractive Surgery journey, from beginning to end. Pre-Operative Evaluation A full eye examination including complete ocular and health history, refractive status, and dilated ocular health evaluation is recommended prior to referring the patient to our Centre. This is advantageous to the patient because we can pre-screen the referral and handle/discuss any issues prior to the patient’s arrival for Gimbel Eye Centre assessment. This is advantageous to you because it establishes your participation in the patient’s experience and encourages the patient to return to you for follow up care and beyond. The data collected in your referral will be carefully evaluated in conjunction with a complete Gimbel Eye Centre assessment to maximize accuracy and repeatability in the data used for surgery purposes. There is historical precedence that it is both the Refractive Surgery Centre’s and the Primary Eyecare Provider’s responsibility to ensure adequate informed consent surrounding the risks and benefits of refractive surgery, including presbyopia considerations and monovision. Refractions: For refractive surgery purposes: it is recommended to maximize the cyl and minimize the sphere component as this increases the odds of achieving emmetropia. Visual Acuity: For testing standardization, we request measurements up to 20/15. Referrals to Gimbel Eye Centre Pre-Operative Surgery Assessment Referral Forms (provided in this guide) can be forwarded via fax or e-mail. Our Patient Counselor will then contact the patient directly to make arrangements for a Gimbel Eye Centre preoperative assessment, surgery, and 1-day post-operative follow-up. A few things to be aware of in referring your patients: For All Surgery Types: The patient is required to discontinue soft contact lens wear for a minimum of 48 hours prior to testing at Gimbel Eye Centre, or 2 weeks for RGP contact lenses. For Potential Phakic IOL candidates: The patient should be prepared for two days of pre-operative testing at Gimbel Eye Centre and should make their travel arrangements accordingly. Post-Operative Evaluations After the patient’s 1-day follow up visit, we encourage the patient to return to you for their follow up care. A report will be sent to you indicating type of surgery performed and the patient’s current vision status. Follow up frequency and testing will be outlined in each section of this guide. A Post-Operative Follow Up Referral form (provided in this guide) should be sent to Gimbel Eye Centre for review, and a response will be returned if requested. We are happy to reassess the patient upon your request at no additional fee. Please be advised that due to processing times, it may be several weeks before you receive co-management fees. Last Revised April 2014 7 | gimbel.com Corneal Refractive Surgery Descriptions IntraLase Laser Assisted In Situ Keratomileusis (IntraLASIK). There are two lasers used in this procedure. The IntraLase Femtosecond Laser creates a flap by introducing focused energy, which creates a CO2 bubble in between the corneal layers. The laser then creates the laser flap edge by cutting around the perimeter, leaving a superior hinge. This advanced method of flap creation avoids most of the risks of using a mechanical microkeratome blade, reducing post-operative complications such as dryness, providing better contrast sensitivity, and creating an optimal stromal bed surface. Once the flap is lifted, the Nidek Excimer Laser EC5000 CXIII re-contours the corneal surface by ablating tissue to correct the refractive error and minimizing higher order aberrations. If IntraLASIK Xtra was chosen, the KXL collagen cross linking procedure is performed (see KXL Collagen Cross linking section). The surgeon replaces the flap, taking care to ensure good flap position and adherence. Photo Refractive Keratectomy (PRK) The surgeon loosens the corneal epithelium with an alcohol-based chemical solution and gently removes the epithelial cells. The Nidek Excimer Laser EC5000 CXIII re-contours the corneal surface by ablating tissue to correct the refractive error and minimizing higher order aberrations. If PRK Xtra was chosen, the KXL collagen cross linking procedure is performed (see KXL Collagen Cross linking section). The surgeon inserts a bandage contact lens. Photo Therapeutic Keratectomy (PTK) This procedure is not a refractive surgery in that it is done therapeutically, primarily for corneal conditions such as scarring, haze, or recurrent corneal erosion. It is similar to PRK as described above, except the surgeon limits the laser tissue ablation to the pathology or higher order aberrations being treated and stops once sufficient pathological tissue has been removed. The surgeon then inserts a bandage contact lens and healing will be similar to PRK. Astigmatic Keratotomy (AK) This procedure is generally done in conjunction with Intraocular surgery such as cataract surgery, and is done to reduce minor amounts of corneal astigmatism. The surgeon strategically creates a partial thickness peri-limbal incision. The length of the incision influences the amount of flattening of the steepest corneal meridian. KAMRA Inlay for Presbyopia KAMRA Inlay is a polyvinylidene fluoride inlay with a 1.6 mm aperture placed into the cornea of the non-dominant eye. It brings the depth of focus into arms length range for the presbyope. The cornea is marked for centration, and the IntraLase Femtosecond Laser creates a tunnel 200 microns into the stroma (or 100 microns under a original IntraLASIK flap). The surgeon inserts the KAMRA inlay into the tunnel using specialized forceps. Laser Technology and Wavefront Treatment All patients at Gimbel Eye Centre undergo wavefront analysis, which measures the Higher Order Aberrations of the entire eye. Factors affecting Higher Order Aberrations include refractive error, corneal abnormalities (such as scars), and lenticular changes, which can impact the quality of the vision. The standard laser treatment for all Gimbel Eye Centre patients is an aspheric, wavefront-optimized treatment. In addition, our surgeons use Active Tracker technology to follow the eye’s movements during laser treatment, and Torsion Error Detection to compensate for natural rotation of the eye while lying down. Iris recognition technology is used, which takes the OPD scan iris information to align the cylinder treatment axis at surgery. gimbel.com | 8 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Corneal Refractive Surgery Patient Selection Eligibility Criteria for Corneal Refractive Surgery* Type of Surgery Refractive Range Healing Time/Time off Work Other Considerations PRK -0.75 to -8.00D +1.00 to +2.00D cyl -0.50D to -4.00D 7-10 days healing 1 week off work 3 days discomfort • adequate pachymetry • acceptable corneal topography • may be preferred for certain occupations (police) • ease of enhancement PTK any 7-10 days healing 1 week off work 3 days discomfort • reserved for corneal pathologies such as scars, haze, or recurrent corneal erosion, higher order aberrations IntraLASIK -0.75 to -8.00D +1.00 to +2.00D cyl -0.50D to -4.00D 3-5 days 3 days off work minimal discomfort • adequate pachymetry • acceptable corneal topography • consider rare risk of flap dislodgement AK cyl -0.50D to -2.00D Must have spherical equivalent of almost plano if this is a primary surgery orthogonal cylinder axis. 1-2 days healing minimal discomfort • less predictable than other refractive surgery options • acceptable corneal topography • often done in conjunction with other procedures, thus post operative medications are those of the primary surgery. KAMRA inlay Sphere 0.0 to –1.00D Cylinder < -1.00D For combined procedures, the starting cylinder amount must be less than 3.00D 3-5 days healing May take up to 6 weeks for vision clarity to return 3 days off work Minimal discomfort • adequate pachymetry • acceptable corneal topography • age 45-65 • mesopic dim pupil size < 6 mm • for combined procedures, must wait 3 months after primary surgery prior to doing KAMRA inlay * The patient should be at least 18 years of age, not pregnant or nursing, with at least 12 months of stable refractions (within +/-0.50D). Last Revised April 2014 9 | gimbel.com Corneal Refractive Surgery Patient Selection Contraindications for Corneal Refractive Surgery Category Condition Comments Ocular Pathology Corneal scar PRK may be preferred due to risk of flap complication Endothelial Dystrophy PRK may be preferred due to risk of endothelial cell damage with flap creation Map Dot Fingerprint Dystrophy and/or Recurrent Corneal Erosion PRK may be preferred due to weak Bowman’s layer Herpes Simplex/Zoster with history of ocular involvement Considered on a case-by-case basis due to risk of re-activation Lid Disease i.e. Blepharitis Must be pre-treated due to risk of infiltrates/ infection Extreme Dry Eyes Considered on a case-by-case basis Phakic IOLs may be preferred Binocular Dysfunction If prism required in glasses and/or pt experiences diplopia/headaches with contact lenses, then there may be a risk of decompensation after surgery and may require glasses with prism after surgery. Amblyopia (BCVA <20/40) Pt must understand the risks/implications of doing surgery when one eye is already weak Nystagmus Considered on a case-by-case basis. Consider challenges in eye stability during the surgical procedure. Other i.e. macular degeneration, retinal holes or tears Priority will be given to the pathology first. Consider potential vision loss due to surgery. Autoimmune Disorders: – rheumatoid arthritis, Sjogren’s syndrome, Lupus Considered on a case-by-case basis due to risk of corneal melt Phakic IOLs may be preferred Gastrointestinal Disorders: – Ulcerative Colitis, Crohn’s Disease, Irritable Bowel Syndrome Considered on a case-by-case basis due to risk of inflammatory reaction. Must be in remission. Phakic IOLs may be preferred Diabetes Must not have any retinopathy, and blood sugar levels should be controlled. Consider infection risk. Immuno-compromised patients: HIV, AIDS, Hepatitis Prefer that the patient is on HART therapy and the virus is not detectable in the blood. Consider infection risk. For Hep B or C, consider risk of transmission. Accutane, Clarus Must be off this medication for 6 months prior to surgery due to risk of severe dryness Systemic Pathology Medications gimbel.com | 10 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Corneal Refractive Surgery Post Operative Care Postoperative Medication and Follow Up Regimen Type of Corneal Surgery Medication/Treatment Protocol IntraLASIK or Epi ON Therapeutic Cross Linking ➢ ➢ ➢ Prednisolone 1.0% • qid x 7 days Vigamox 0.5% • qid x 7 days then stop Artificial Tears: • q15-30 minutes during waking hours x 2 days, then prn • Celluvisc for first 4 sleeps, then prn Follow Up Schedule Day 1, Week 1, Month 1 Then yearly eye examinations Eye Shields: • First 5-7 nights to protect the eyes/maintain hydration PRK or PTK or Epi OFF Therapeutic Cross Linking ➢ ➢ ➢ ➢ ➢ Vigamox 0.5% • qid x 7 days then stop Gabapentin • 300 mg p.o. tid x 3 days • okay to use Advil or Tylenol in conjunction with Gabapentin if needed FML 0.1% • qid x 1 month minimum (see Extended Medication Protocol next page) Voltaren 0.1% • qid on day of surgery then prn up to qid for the first week Tetracaine 0.5% • last resort pain eye drop prn, used sparingly Day1, Day 3, Week 1, Month 1, Then monthly until 1 month after FML is discontinued, then yearly eye examinations Artificial tears • q15-30 minutes-waking hours until contact lens is removed then prn • Celluvisc for first 4 sleeps, then prn Eye Shields: • First 5-7 nights to protect the eyes/maintain hydration Bandage Contact Lens: • To be removed after re-epithelialization, with forceps, by Doctor KAMRA Inlay Same meds as IntraLASIK, but at 1 week, add FML 0.1% qid x 3 weeks, then tid x 4weeks, then bid x 4 weeks, then stop Day 1 Week 1 Week 2 Month 1, 2, and 3 * More or less visits can be scheduled as deemed clinically necessary. Last Revised April 2014 11 | gimbel.com PRK Post-Operative Extended Medication All patients require FML qid for the first month. Taper regimen is based upon primary preoperative refraction. For patients having an enhancement, the taper regimen is determined by the initial preoperative refraction prior to the first surgery; not the current refraction. Pre-Operative Spherical Equivalent FML 0.1% Duration Guideline +2.00D to -3.00D Qid x 1 month then stop -3.00D to -6.00D Qid x 1 month Tid x 1 month Bid x 1 month Qd x 1 month then stop -6.00D or greater Qid x 2 months Tid x 1 month Bid x 1 month Bid/qd alternating x 1 month Qd x 1 month Qd every 2nd day x 1 month Then 1 gtt 2 times per week x 1 month Guidelines in altering FML 1% taper regimens: 1) If the patient has corneal haze, increase the dose and advise UV protection. 2) If the patient shows myopic regression, increase dose and/or maintain current dosage for longer. 3) If the patient has a hyperopic response, consider decreasing the FML dosage faster Examples of deviation from protocol: 1. Patient’s post op Rx is -0.75D and is currently on FML bid, consider increasing to qid. 2. Patient’s post op Rx is +1.00D and is currently on FML qid, consider decreasing to bid. 3. Patient’s post op Rx is +1.00D and has significant corneal haze: treat aggressively with FML medications i.e. qid (the need to treat the haze is priority over the hyperopia). NOTE: Patients who show consistent regression and are more than 6 months post surgery, are unlikely to respond to an increase in FML and should be monitored for stability in consideration of enhancement. NOTE: All patients require monthly tonometry measurements while taking FML. gimbel.com | 12 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Corneal Surgery Post Operative Presentation and Activity Restrictions The following is a summary of potential symptoms and findings associated with each surgery. For the normal findings, an expected timeline for the finding to subside is provided. (H= hours, D= days, W=Weeks, M= Months) Type of Surgery Normal (Time to Subside) Not Normal Activity Restrictions IntraLASIK or KAMRA Inlay VA 20/15 to 20/50 (may take 3-5 days to start improving) Foreign Body Sensation (48 H) Tearing/Photophobia (72H) Dry Eyes (up to 6M) Sub-conjunctival hemorages (2-3W) Ghosting/Halos/Glare (2-3M) Less contrast sensitivity (improves up to 6M but usually reaches 98% of original contrast) Epithelial edema (2-4W) Pus-like discharge Dislocated/wrinkled flap/inlay” Unusually high pain Interface cloudiness Epithelial Defect Infiltrate Epithelial cells under flap Foreign body/debris under flap Diffuse Lamellar Keratitis Defects, tears in inlay Blocked perforations in inlay (on retroillumination) • No pets in the bed for 2 nights after surgery PRK or PTK *AK does not have the same discomfort elements as PRK and PTK Last Revised April 2014 VA 20/30 to 20/400 (up to 1W) Mild to severe pain (48H) Foreign body sensation (3-5D) Tearing, Photophobia (3-5D) Lid edema (3-5D) Ghost images (2-4W) Dry eyes (up to 3 M) Halo/Glare (2-3M) Drop in VA/diplopia (occurs at day 3-5 and is a result of fusion line formation)(72H) Less contrast sensitivity (improves up to 6M but usually reaches 98% of original contrast) Descemet’s Folds (72H) Epithelial Defect (3-5D) Presence of Contact Lens (remove after re-epithelialization) • No eye make-up for 7 days • No swimming, hot tub, water sports for 21 days • No Dusty/smoky environments for 21 days • No eye rubbing for 6 weeks • UV protection for 6 months • Safety glasses during appropriate activities Pus-like discharge Infiltrate/infection Anterior chamber cells Non-healing epithelial defect (beyond 5-7 days) Raised IOP (check after 3W) Corneal haze 13 | gimbel.com Corneal Refractive Surgery Complications This list contains the most likely observed complications. If you have any questions please contact us. Complication IntraLASIK PRK/PTK/AK KAMRA inlay Description Treatment Dry Eyes X X X Common after surgery and usually improves over time although can be permanent. If severe diffuse SPK noted, consider preservative toxicity. Traditional Dry Eye Therapy modalities Inflammation X X X May present as whitish distinct or diffuse infiltrates sometimes in a perilimbal arcuate pattern. Risk of corneal melt in rare cases. Look for corneal thinning. May be associated with systemic autoimmune conditions. Refer to GEC for assessment. Prompt and aggressive treatment is needed. Halos/ Starbursts X X X Usually diminish over a few months but can be permanent and affect night driving. Patients with large pre-op pupil size should be advised of this potential risk. Usually subsides but can use yellow tinted glasses, or Alphagan gtts prn Epithelial Ingrowth X X Migration and proliferation of epithelial cells under the flap. More common after relifting of a flap i.e. enhancements. May cause blurry vision, FBS, dryness, tearing. Monitor, if migrating more than 1 mm consider surgical intervention. Infection X X X Rare but possible. Ulcers, epithelial defects, haze, decrease in vision, pus-like discharge, red eye. Contact GEC for guidance in treatment Corneal Haze X X X With IntraLASIK can have patchy areas of haze that are not clinically significant. With PRK it appears like superficial white grainy subepithelial cells that don’t stain. It typically presents within 1 month and peaks around 2-3 months before subsiding. For PRK: Advise UV protection, treat with steroids. In rare cases, PTK may be considered. Ectasia X X X Corneal instability resulting in refractive error, vision decline with visual distortion. Usually requires topography to diagnose. Refer to GEC for assessment if vision affected. Flap Disturbances X Mild wrinkles, shifting of flap, striaie formation. May or may not be visually significant. Refer to GEC for assessment. gimbel.com | 14 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Corneal Refractive Surgery Complications and Treatment (con’t) Complication Intra LASIK PRK/PTK/ AK KAMRA inlay Description Treatment Epithelial Erosion X X X May result in loose epithelium, rough edges or defects especially along flap margin in IntraLASIK, or ablation zone in PRK. Foreign body sensation, pain especially when opening eyes in the morning, decrease in vision. Increases risk of DLK and epithelial ingrowth in IntraLASIK patients. May subside as eye heals further. Copious non-preserved lubrication. Some cases may require antibiotics and/or bandage contact lens. Rarely, PTK may be considered. Diffuse Lamellar Keratitis (Sands of Sahara) X X Rapid onset, non-infectious white blood cells reaction in the interface (looks like fine white grainy cells). May have pain, blurry vision, FBS, photophobia and can rapidly progress if not aggressively treated. In early stages may be asymptomatic and limited to the periphery of the flap, and one needs to rely on clinical diagnosis. More severe cases can involve the central cornea, and present with sanddune-like cell accumulation, hazy flap, edema and striaie. Usually occurs within 1-3 days post-operatively but can also present later in cases of trauma. Prompt and aggressive treatment is needed. Please contact GEC immediately so the surgeon can be involved in treatment as this has the potential to have permanent vision effects. Refractive Error X X May be due to regression (mild keratometry changes from either epithelial fill-in or prolific epithelial growth resulting in refractive error). May settle/resolve over time. May also be influenced by dry eyes, therefore dry eye therapy is recommended for all patients with post-operative refractive error. Consider enhancement after 3 months of stable vision. Coverage is 18 months. Minimum refractive error is >0.50D. May enhance only one eye at a time. If deemed unsafe, the surgeon may advise against further surgery. X Centration of the inlay cannot be accurately assessed at the slit-lamp due to parallax. Pt should have an AcuTarget map done at Gimbel Eye Centre. Surgical Repositioning of the inlay can be done to provide better centration. Decentred Inlay Last Revised April 2014 X 15 | gimbel.com Phakic IOL Refractive Surgery Descriptions Phakic IOLs refer to synthetic implants that are inserted into the eye without removing the natural crystalline lens. They are considered a “premium” option as they provide superior quality of optics compared to corneal refractive surgery in all but relatively small refractive errors. They are removable, preserve remaining natural accommodation, and pose less retinal risk compared to lensectomy surgeries i.e. Refractive Lens Exchange. Please be aware that the need for special testing, calculations, and lens implant ordering times necessitates a processing time of 1-3 months from the date of the initial consultation to the actual surgery date. Gimbel Eye Centre currently performs two types of Phakic IOL surgeries: Implantable Collamer Lenses (ICL) Performed at Gimbel Eye Centre since 1997, this implant sits in the posterior chamber, supported by the sulcus and aqueous humour pressure. Prior to the day of surgery, a prophylactic peripheral iridotomy will be performed (usually 2 iridotomies between the 10 and 2 o’clock position in the eye). This is done to ensure adequate aqueous flow. Occasionally, a single Surgical Iridectomy will be chosen instead, if the patient’s irises are very darkly pigmented. The surgery takes about 15 minutes per eye, involves less than a 3 mm self-sealing clear corneal incision, and usually no stitches or needles are required. After the incision is made, and the anterior chamber is filled with a viscoelastic material, the implant is placed initially in the anterior chamber. Then the plate haptics are manipulated to go behind the iris, so that the implant vaults over the natural crystalline lens. If a Toric Implant is inserted, the surgeon manipulates the implant to the desired orientation. The viscoelastic material is flushed from the eye and care is taken to ensure the wound is secure. These implants are not visible to the naked eye. Angle Supported Phakic IOL (Cachet) Performed at Gimbel Eye Centre since 2010, this surgery differs from ICL in that the lens (or implant) is placed in the anterior chamber. It is supported by its flexible haptics nestled in the anterior chamber angle, similar to a shower curtain rod. The surgery takes about 15 minutes per eye, involves less than a 3 mm self-sealing clear corneal incision, and usually no stitches or needles are required. After the incision is made, and the anterior chamber is filled with a viscoelastic material, the implant is placed in front of the iris in the anterior chamber. The flexible haptics are manipulated into position. The viscoelastic material is flushed from the eye and care is taken to ensure the wound is secure. These implants can be cosmetically visible at close range with proper lighting, much like the edge of a contact lens. As of the most recent revision of this comanagement guide, the Cachet implants are not currently available for implantation. We do not know when they will become available again.” gimbel.com | 16 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Phakic IOL Surgery Patient Selection Eligibility Criteria for Phakic IOL Surgery Type of Surgery Refractive Range Healing Time/Time off Work Other Considerations ICL -2.75D to -20.00D +2.00D to +14.00D cyl up to -5.00D (myopic torics only) 3 days healing 1 week off work (for numerous appointments) • Minimum AC depth 2.6/2.75 mm. Younger patients need more generous AC depth • Corneal diameter 10.50 - 13.00 mm • Bioptics can be considered Cachet -6.00D to -16.50D 3 days healing 3-4 days off work (for numerous appointments) • Minimum AC depth plus pachymetry = 3.2 mm • Must meet minimum age adjusted endothelial cell count • Mesopic pupil size <7.00D • Corneal diameter 10.50 - 13.00 mm • Bioptics can be considered * The patient should be at least 18 years of age, not pregnant or nursing, with at least 12 months of stable refractions (within +/-0.50D). Contraindications for Phakic IOL Surgery Category Condition Comments Ocular Pathology Glaucoma May impede aqueous flow Pigment Dispersion Syndrome Implant may interact with weakened iris layer, worsening the condition Recurrent Uveitis Implant may exacerbate the condition Binocular Dysfunction If prism required in glasses and/or pt experiences diplopia/headaches with contact lenses, then there may be a risk of decompensation after surgery Amblyopia Pt must understand the risks/implications of doing surgery on an amblyopic system Other i.e. macular degeneration, retinal holes/tears Priority will be given to the pathology first. Consider potential vision loss. Diabetes Must not have any retinopathy, and blood sugar levels should be controlled. Consider infection risk. Immuno-compromised Patients: HIV, AIDS, Hepatitis Prefer that the patient is on HART therapy and the virus is not detectable in the blood. Consider infection risk. For Hep B or C, consider risk of transmission. Systemic Pathology Last Revised April 2014 17 | gimbel.com Phakic IOL Postoperative Care Postoperative Medication and Follow Up Regimen Type of Phakic IOL Surgery Medications/Treatment Protocol Follow Up Schedule ICL Prednisolone 1.0%: • qid starting day of surgery until 1 week post op • bid x 2 weeks Day 1, Week 2, Month 2, Month 6, Month 12, then yearly eye examinations Vigamox 0.5%: • qid starting 1 day pre-op until 1 week post op Emergency Medications: Cyclogel 1.0% as instructed Phenylephrine 10% qhs on day of Sx, then as instructed” (to be taken if symptoms of brow ache, pt to first contact their follow up Doctor) Artificial tears: q1h for 1-2 days then prn Cachet Prednisolone 1.0%: • qid starting day of surgery until 1 week post op • bid x 2 weeks Vigamox 0.5%: • qid starting 1 day pre-op until 1 week post op Artificial tears: • q1h for 1-2 days then prn Day 1, Week 2, Month 2, Month 6, Month 12, then yearly eye examinations *Pt is required to return to GEC every 6 months for Specular Microscopy for an indefinite period of time. The patient will remain with their Primary Eyecare Provider for all routine eye care. The fee for each Specular Microscopy visit is $75. *Please do once yearly gonioscopy testing to monitor for angle synechiaie *More or less visits can be scheduled as deemed clinically necessary. gimbel.com | 18 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Phakic IOL Post Operative Presentation and Activity Restrictions The following is a summary of potential symptoms and findings associated with each surgery. For the normal findings, an expected timeline for the finding to subside is provided. (H= hours, D= days, W=Weeks, M= Months) Type of Surgery Normal (Time to Subside) Not Normal ICL VA 20/15 to 20/50 (accommodation may be affected by pupil dilation) Foreign Body Sensation (48 H) Tearing/Photophobia (48H) Dry Eyes (up to 2M) Ghosting/Halos/Glare (may take a while for pupil to return to normal size )(6M) Edema at the incision side (1W) Descemet’s Folds (72H) Pupil Dilation (48H) Vault 2-4+ (see next page) Orientation should be on target immediately Mild AC reaction (1-2+ cells, 1+flare) Pus-like discharge Wound gaping/leak Unusually high pain Epithelial Defect Elevated IOP High Vault (see next page) Low to No Vault Shallow Angle Iris to Corneal touch Iris Transillumination Non resolving anterior chamber reaction Iridotomy not patent Progressively excessive deposits on the IOL Anterior subcapsular lens changes ICL is rotated (see next page) Retinal Detachment VA 20/15 to 20/50 Foreign Body Sensation (48 H) Tearing/Photophobia (48H) Dry Eyes (up to 2M) Ghosting/Halos/Glare 6M) Edema at the incision site (1W) Descemet’s Folds (72H) Pus-like discharge Wound gaping/leak Unusually high pain Significant corneal haze Non-resolving Descemet’s folds Elevated IOP Progressive pigment on IOL Implant sits close to the cornea Pupil irregular Haptics not located in angle Anterior Subcapsular lens changes Iris Transillumination Non resolving AC reaction Cachet Last Revised April 2014 Activity Restrictions • No pets in the bed for 2 nights after surgery • No eye make-up for 7 days • No swimming, hot tub, water sports for 14 days • No Dusty/smoky environments for 14 days • No vigorous eye rubbing • Safety glasses during appropriate activities 19 | gimbel.com Phakic IOL Postoperative Evaluation Considerations The Phakic IOLs have special considerations during the follow up care. If you have any questions please contact us. Type of Surgery Special Consideration Description/Evaluation Interpretation ICL Vaulting The subjective assessment of how many central IOL thicknesses could be placed in the space between the natural crystalline lens and the implant. This may be influenced by implant length, thickness, position in the sulcus, trapped viscoelastic fluid behind the implant, and PI patency. Example: 2 IOL thicknesses= 2+ vault • Vault less than 1+ poses risk of cataract formation • Vault more than 4+ poses risk of pupil block In both situations, GEC should be notified. Orientation The subjective assessment of the location of the Toric engraving on the implant haptic, in relation to a 180 degree scale. Must be done dilated to see the marking. Example: 030 degrees *Note this does NOT equal refractive error axis • If orientation does not match intended orientation, refractive error will be impacted • Consider improper implant rotation if pt presents with a significant hyperopic astigmatic error Example: +2.50-2.50 x 010 Vaulting Given the very flexible haptics, the implant length is much more forgiving in these implants. In general one would like to see a small vault over the iris so as not to rub the iris, but not too high as to risk endothelial damage. • A very high vault may risk endothelial cell damage over time Orientation Although Cachet implants are not available in astigmatic correction, and therefore orientation does not impact refractive error, practitioners are still encouraged to document the physical orientation of the implant in relation to a 180 degree scale. Rotation would indicate too loose a fit or eye rubbing • Implant rotation would risk damage to the trabecular meshwork and/or endothelium. Cachet gimbel.com | 20 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Phakic IOL Surgery Complications and Treatment This list contains the most likely observed complications. If you have any questions please contact us. Complication ICL Cachet Description Treatment Pupil Block X X Pain, brow ache, photophobia, blur, nausea, elevated IOP. Usually occurs early postoperatively and can be associated with implant length, trapped viscoelastic fluid, or PI patency issues. Contact GEC ASAP for guidance as the treatment varies with different causes of pupil block and amount of IOP elevation. Cataract X X Occurs later postoperatively (mean time is 3 years) and is often associated with low vault. It is important to distinguish implant related lens changes (anterior subcapsular) versus natural progression of age-related (nuclear sclerosis or cortical spoking). Contact GEC for guidance in treatment. The risk of removal and replacement of the implant has to be considered (traumatic cataract). Infection X X Endophthalmitis is rare. Unilateral red, painful eye, anterior and/or posterior chamber reaction, blurry vision, hypopyon, white clumps in vitreous. Contact GEC immediately for surgeon guidance as this is a potentially sight threatening condition. Intraocular Inflammation X X Significant AC reaction. Aggressive steroidal treatment, contact GEC. Corneal Haze/ Decompensation X X Descemets folds, corneal edema, decrease in vision. Muro 128 gtts qid, contact GEC if no improvement after 72 hours. Dry Eyes X X Common early post-operatively but longer term is less risk than corneal refractive surgery and similar to cataract surgery. Traditional Dry Eye Therapy Modalities Halos/glare X X More common with Cachet as the lens is more anterior to pupil. Greater risk with large pupils and high correction. May subside over time. May subside after 6 months, monitor. Alphagan gtts prn may be considered. Refractive Error X X May be associated with temporary corneal edema. May also be associated with implant rotation. Consider etiology and treat accordingly. Bioptics may be considered. Implant Rotation X X Usually obvious by the 2-week check after surgery. Refractive error and blur are present if toric ICL. Often a hyperopic astigmatic error. Contact GEC for surgical treatment consideration. Wound Leak X X Very low IOP, ache, blur. Globe soft on palpation. +/- Seidel sign. Wound may be gaping. Contact GEC ASAP for surgical intervention, risk of endophthalmitis. X Cachet: pupil ovalization Cachet: Angle synechiaie Monitor, contact GEC if IOP affected. Other Last Revised April 2014 21 | gimbel.com Refractive Lens Exchange/Cataract Extraction Descriptions Surgery Description Refractive Lens Exchange (RLE) and Cataract Extraction (CE) are both intraocular lensectomy procedures that have been performed at Gimbel Eye Centre for several decades. The surgeon creates a strategically placed incision near the cornea or at the limbus, usually 2.2 mm in length. The anterior chamber is filled with viscoelastic gel. An anterior capsular curvilinear capsulorhexis (CCC) is made with forceps and the lens is removed with a phacoemulsification technique. The synthetic implant is inserted and placed within the natural lens’ capsular bag. If a Toric Implant is inserted, the surgeon manipulates the implant to the desired orientation. The viscoelastic material is aspirated from the eye, intra ocular antibiotics are instilled and care is taken to ensure the wound is secure. Alberta Health Care (AHC) Covered Services It is an ongoing challenge to the ophthalmological community to manage the aging population’s growing need for cataract extraction. All cataract surgeons are given a finite number of cataract surgery allotments each year, which directly influences the length of the waiting lists, and this can change depending on the political environment. As lens changes are part of aging (as are a few wrinkles and a few grey hairs), patients with early lens changes are not classified as cataracts. They can be monitored until such time as the changes become significant enough to be disabling and require a medically necessary cataract operation. Also, choosing the option of uninsured Refractive Lens Exchange (RLE) for refractive purposes may be considered. We are committed to working within the public healthcare system, while respecting the needs and desires of the patient. Implant Choices Over the years the lensectomy procedure has evolved with improved surgical techniques and implant choices, and consequently the expectations of the patient has risen. At Gimbel Eye Centre we are constantly evaluating technological advancements and weighing them against current market demands. It is our position at Gimbel Eye Centre that no implant choice can provide a total replacement for natural accommodation. However, with careful patient selection, we can offer the patient a wide selection of implant choices and tailor the treatment plan to the individual’s lifestyle. In the section titled Refractive Lens Exchange/Cataract Surgery Lifestyle Implant Choices, we will discuss the implant choices currently offered at Gimbel Eye Centre. The choice of implant is a very personal choice made between the patient and the surgeon. Any insight you can give us regarding your patient’s lifestyle is immensely helpful in arriving at the final implant choice. gimbel.com | 22 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Refractive Lens Exchange/Cataract Surgery Patient Selection Eligibility Criteria for Refractive Lens Exchange/Cataract Surgery Type of Surgery Refractive Range Healing Time/Time Off Work Other Considerations Refractive Lens Exchange All ranges of correction IOL powers available -10.00D to +40.00D Astigmatism: -0.75D to -11.00D Toric considered if corneal cyl >=-0.50D 3-5 days healing 3-5 days off work • careful lifestyle review will influence implant selection • pt is responsible for all costs • pt must understand loss of accommodation and the limitations of lifestyle implants Cataract Surgery All ranges of correction IOL powers available -10.00D to +40.00D Astigmatism: -0.75D to -11.00D Toric considered if corneal cyl >=-0.50D 3-5 days healing 3-5 days off work • only a standard spherical implant is covered under AHC • for all other implant choices, pt to pay the difference • pt must understand loss of accommodation and the limitations of lifestyle implants Contraindications for Refractive Lens Exchange/Cataract Surgery Category Condition Comments Ocular Pathology Endothelial dystrophy/poor endothelial morphology Rarely, corneal decompensation can occur, sometimes requiring corneal transplant. Any acute ocular condition that warrants priority treatment Example: uncontrolled glaucoma or wet macular degeneration or retinal pathology • Priority treatment is given to the acute ocular condition before surgery. • A risk/benefit analysis should be viewed quite differently between an elective (RLE) and medically necessary procedure (cataract surgery) Immuno-compromised Patients: HIV, AIDS, Hepatitis Prefer that the patient is on HART therapy and the virus is not detectable in the blood. Consider infection risk. For Hep B or C, consider risk of transmission. Congestive Heart Failure, COPD and other lung problems If necessary, the surgery can be performed with the chest elevated 30-45 degrees. Flomax Risk of Floppy Iris Syndrome. GEC would like to be informed in advance if pt is taking this medication. Systemic Pathology Medications Last Revised April 2014 23 | gimbel.com Refractive Lens Exchange/Cataract Surgery Lifestyle Implant Choices Careful screening of patient’s lifestyle should be done prior to implant selection. Implant Type Description Advantages Disadvantages Comments Fixed Focus (Acrysof, Acrysof Toric, Rayner T Flex Toric etc.) The traditional treatment using a fixed focus implant to either target OU distance, intermediate, near or monovision. Highest quality optics Only one ideal range for each eye — the patient is expected to be dependent on glasses for all other ranges. Toric considered for corneal cyl greater than -0.50D. Monovision (same brands as above) Using a fixed focus implant targeting one eye for near (-1.00D to -2.50D). Greater range of functional vision Distance vision quality compromise. May affect depth perception. Recommend trialing with contact lenses prior to surgery if possible. Please note this will not be exact demonstration of surgery due to presence of lens changes/ loss of remaining accommodation. Accommodative (Tetraflex) Implant is designed to move forward with the movement of ciliary body for near work. Single optics therefore minimal compromise in quality of vision. Higher incidence of residual refractive error . High incidence of needing YAG treatment May have gradual loss of near benefit as fibrotic tissue forms. Pt should be prepared to do 6 months of near vision exercises to “train” how to maximize lens advantages. Should try to avoid reading glasses as much as possible. Multifocal (Restor, Restor Toric. Rayner M Flex, Rayner M flex T) Power is in annular rings which splits the images in a refractive or diffractive pattern. Functions may be influenced by changes in pupil size during far/near work. Better refractive predictability than Accommodative implants. Loss in contrast sensitivity/distance vision quality. Potential halos or rings of lights around light sources at night. Intermediate range is the weakest. Neural adaptation may have symptoms reduce after 2-6 months. Sulcoflex Pseudophakic supplementary IOL can provide additional sphere, toric or multifocal power to the eye. Removable Predictable outcomes The multifocal choice has the same disadvantages as noted above but is easily removable. A removable option that can be done during primary surgery or as secondary surgery KAMRA inlay *for details, please refer to the Corneal Refractive Surgery Section Small inlay implanted into the cornea of the non dominant eye, done after primary surgery Can restore functional intermediate/near vision without the imbalance of monovision Mild reduction in contrast sensitivity A removable option that is done a minimum of 3 months after primary surgery. gimbel.com | 24 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Refractive Lens Exchange/Cataract Surgery Post Operative Care Post Operative Medication and Follow Up Regimens Type of Surgery Medication/Treatment Protocol Refractive Lens Exchange Vigamox 0.5%: qid starting 1 day pre-op until 1 week post op Prednisolone 1.0%: • qid starting day of surgery until 1 week post op • bid x 2 weeks Follow Up Schedule Day 1, Week 2, Week 8 then yearly eye examinations Artificial Tears: • q1/2 hour x 3 days • prn afterwards Glasses: • Should allow 4-6 weeks for capsular contraction before prescribing glasses for any residual refractive error. Cataract Surgery Vigamox 0.5%: qid starting 1 day pre-op until 1 week post op Prednisolone 1.0%: • qid starting day of surgery until 1 week post op • bid x 2 weeks Day 1, Week 2, Week 8 then yearly eye examinations Artificial Tears: • q1/2 hour x 3 days • prn afterwards Glasses: • Should allow 4-6 weeks for capsular contraction before prescribing glasses for any residual refractive error. *More or less visits can be scheduled as deemed clinically necessary. For Cataract Surgery, billing is in compliance with Alberta Health Care Regulations. Last Revised April 2014 25 | gimbel.com Refractive Lens Exchange and Cataract Surgery Post Operative Presentations and Actvity Restrictions The following is a summary of potential symptoms and findings associated with each surgery. For the normal findings, an expected timeline for the finding to subside is provided. (H= hours, D= days, W=Weeks, M= Months) Type of Surgery Normal (Time to Subside) Not Normal Activity Restrictions Refractive Lens Exchange/ Cataract Surgery VA 20/15 to 20/50 (consideration should be given to other ocular conditions affecting BCVA) Foreign Body Sensation (48 H) Tearing/Photophobia (48H) Dry Eyes (up to 2M) Ghosting/Halos/Glare (2-3M) Edema at the incision site (1W) Descemet’s Folds (72H) Pupil Dilation (24H) Reflections/Distortions from IOL (4W) Increase in floaters (indefinite) Mild AC reaction (1-2+ cells, 1+flare)Change in pupil size/shape Pus-like discharge Wound gaping/leak Unusually high pain Epithelial Defect Elevated IOP Significant anterior chamber reaction Fibrous tissue formation Hypopyon Lens is rotated (Toric) Retinal Detachment Posterior capsular opacification Macular Edema Implant not sitting “in the capsular bag” Implant displaced from central position Posterior capsular tear Implant decentration off of the visual axis (especially for multifocal implants) • No pets in the bed for 2 nights after surgery • No eye make-up for 7 days • No swimming, hot tub, water sports for 21 days • No Dusty/smoky environments for 14 days • No eye rubbing • Safety glasses during appropriate activities gimbel.com | 26 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Refractive Lens Exchange/Cataract Surgery Complications and Treatment This list contains the most likely observed complications. If you have any questions please contact us. Complication Description Treatment Infection Endophthalmitis is rare. Unilateral red, painful eye, anterior and/or posterior chamber reaction, blurry vision, hypopyon, white clumps in vitreous. Contact GEC immediately for surgeon guidance as this is a potentially sight threatening condition. Hours of waiting can make a big difference. Elevated IOP Common early postoperatively, trapped viscoelastic fluid. May or may not be symptomatic. Topical and oral medications. If IOP > 40 mm Hg consider paracentesis aqueous drainage by the surgeon. Intraocular Inflammation Significant AC reaction. Rarely fibrous strands across the pupil. Aggressive steroidal treatment – Prednisolone 1% q1h, Atropine 1% or at least Cyclopentolate 1% , contact GEC. Corneal Haze/Decompensation Descemets folds, corneal edema, decrease in vision. Muro 128 gtts qid, can also add Pred Forte 1.0% qid if needed, contact GEC if no improvement after 72 hours. Cystoid Macular Edema Painless decrease in vision usually after the first few weeks. Elevated macula with or without hemorrhages. Contact GEC for further diagnosis (OCT) and treatment considerations. Posterior Subcapsular Opacification Painless decrease in vision usually after the first few weeks. Posterior capsule may have white or clear fibrotic cells, Elschnig pearls, or visually significant striations. Non-urgent referral to GEC if visually significant. *YAG treatment preferably deferred until 3 months post op if possible to minimize risks of treatment. Retinal Detachment/Hemorrhage Painless decrease in vision associated with increase in floaters, flashes, or curtain to side of vision. May also see hemorrhages/red blood cells in the vitreous/retina. Urgent referral to retinal specialist. Refractive Error May be associated with temporary corneal edema near the incision. May also be associated with implant rotation. Consider etiology and treat accordingly. Consider further refractive surgery, or glasses, after 6-8 weeks. Implant Dislocation Usually a result of trauma with zonular tears if capsule and IOL are subluxated by the CCC. May subluxate months or years after surgery. Refer to GEC for surgical treatment. Last Revised April 2014 27 | gimbel.com Collagen Cross Linking Description Collagen Cross Linking The concept of collagen cross linking has been prevalent in dentistry for several decades. In ophthalmic practice, collagen cross linking has been used to treat pathological corneas such as keratoconus for a number of years. Historically, the Collagen Cross Linking procedure (CXL) required a corneal soak with Riboflavin (vitamin B2) for about 30 minutes and then exposure to UV light for 30 minutes. Originally it was believed that this process strengthened the collagen fibrils, but more recent studies suggest it increases the bond strength in between the collagen. This would be similar to adding more and stronger rungs to a ladder, if the sides of the ladder were the collagen fibrils. The UV exposure is equivalent to about one day in the sun. The procedure results in a strengthening of the cornea to almost 4 times its original strength, thus stabilizing the cornea. In addition, Mi et al have reported that cross linking during the laser procedure increases the flap-to-interface adhesion, thus potentially reducing the risk of epithelial ingrowth and/or flap dislodgement.1 The cross linking process has evolved, and Gimbel Eye Centre Calgary location is pleased to provide Accelerated Collagen Cross Linking (KXL) with the Avedro system. The higher energy allows for a much shorter Riboflavin soak time of 1-5 minutes and UV exposure of 3-5 minutes. The speed of this new technology allows us to incorporate the procedure more easily into a refractive practice and opens up the possibilities of routine usage. The total energy absorption remains the same, therefor one can expect equivalent results to the previous technology, but in a more practical timeframe. There are two types of situations in which KXL is performed at Gimbel Eye Centre: Prophylactic Treatment Patients may opt to have Prophylactic KXL treatment in conjunction with their corneal refractive surgery especially if there is a pre-operative risk factor for corneal instability. The refractive procedure is performed as usual, and after the laser ablation, the cornea is soaked with a riboflavin solution. If IntraLASIK, the flap is replaced prior to UV light KXL treatment. If PRK, the UV light KXL treatment is done prior to bandage contact lens placement. The healing experience and follow up are the same as regular IntraLASIK or PRK surgery. If a patient opts for this treatment option, their procedures are called IntraLASIK Xtra or PRK Xtra. Post operative care is equivalent to the primary corneal surgery undertaken. Therapeutic Treatment Patients who have diagnosed pathology on the cornea may undergo KXL treatment to stabilize the corneal pathology. Examples of potential Therapeutic KXL candidates are people who have frank Keratoconus, Pellucid Marginal Degeneration, or Iatrogenic Ectasia. In the future, patients who suffer from vision fluctuation as a result of previous Radial Keratotomy procedures may also be candidates. The treatment approach is carefully evaluated by our experienced surgeons, and may include some ablation of the tissue (PRK) for some or all of the refractive error. Currently, therapeutic treatment patients require epithelial debridement to prepare the cornea for the Riboflavin soak, and therefore the healing time/follow up and medication schedule is the similar to a PRK patient. A new formulation of the riboflavin solution means that performing the surgery without removing the epithelium is now available, at the discretion of the surgeon. It is recommended that these patients have a regular post operative topographical analysis of their corneas. Currently this procedure is not an Alberta Health Care insured service. For information regarding Post procedure medication and treatment protocol, please refer to Corneal Refractive Surgery Post Operative Care on page 11. gimbel.com | 28 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Accelerated Collagen Cross Linking (KXL) Patient Selection Eligibility and Contraindications for Collagen Cross Linking Type of Treatment Clinical Findings Contraindications Comments Prophylactic Minimum residual corneal bed depth after laser ablation of 325 microns Some eligible risk factors are: • Young age • Thin corneas • Minor topographical asymmetry • Against-the-rule astigmatism • Steep Keratometry Pseudophakia if no IOL UV protection Aphakia Macular Degeneration Pregnancy Herpetic keratitis Rheumatoid disorders Known riboflavin allergy Patients who are diagnosed with corneal pathology and are not good candidates for refractive surgery The minimum corneal thickness of 325 microns is to protect the endothelium and is an improvement over the previous technology (minimum was 400 microns) *Patients must discontinue vitamin C supplements for 1 week prior and 1 week after surgery Therapeutic Minimum starting pachymetry of 325 microns Corneal pathology such as: • Keratoconus • Pellucid Marginal • Degeneration • Iatrogenic Ectasia Pseudophakia if no IOL UV protection Aphakics Macular Degeneration Pregnancy Herpetic keratitis Rheumatoid disorders Known riboflavin allergy Currently not insured by Alberta Health Services The minimum corneal thickness of 325 microns is to protect the endothelium and is an improvement over the previous technology (minimum was 400 microns) *Patients must discontinue vitamin C supplements for 1 week prior and 1 week after surgery Last Revised April 2014 29 | gimbel.com Presbyopia, Monovision and the Role of the Co-managing Doctor The Presbyopic Conundrum All ophthalmic practitioners are familiar with the longstanding Achilles heal of our industry—the inevitable onset of Presbyopia. When preparing for Refractive Surgery of any type, careful consideration must be given to the effect on near vision. For example, presbyopic patients who are used to removing their glasses to read must understand their current near benefit, and the need for glasses for all tasks arms length and closer after surgery. Refractive Lens Exchange patients also need to have this emphasized, and told that even a monovision trial with contact lenses isn’t a true demonstration given the removal of the accommodative lens after surgery. Monovision The technique of Monovision has been used in prescribing optical devices and in surgeries for decades. The obvious advantage is a wider range of functional vision, at the sacrifice of some distance clarity and perhaps some depth perception. For Refractive Lens Exchange and Cataract patients, it is the ONLY surgical option that uses the highest quality single fixed focus implant while still giving a wide range of vision. It is important to recognize that although there are other “premium” options available such as accommodative and multifocal options, they come at a sacrifice of vision quality. Monovision is the only option where most concerns regarding vision quality can be easily alleviated by a pair of task-specific glasses. With this in mind, Monovision is the most widely used technique to address the needs of the presbyope at Gimbel Eye Centre. The Monovision Trial Recognizing that not every patient will easily adapt to a monovision system, a monovision trial is required prior to surgery. Gimbel Eye Centre encourages the patient to work with their Primary Eyecare Provider in fitting, trialing, and adjusting their own individual monovision system, via contact lenses, to ensure acceptance and adaptation prior to undergoing surgery. This step is an essential component prior to the surgeon making final decisions/calculations for surgery. We encourage the patient to trial monovision for a few days to a few weeks in order to experience what monovision feels like in their own daily environment. The patient should expect to pay the appropriate fees to the Primary Eyecare Provider for this service. Once the trial is completed, we ask that the Primary Eyecare Provider send a report detailing the final monovision fit information (see Monovision form included in this guide). Included in this report we request that you provide a contact lens over-refraction using the final set of contacts that were deemed ideal for the patient. This is in recognition of vertex differences, tear film qualities and astigmatism masking in the contact lens. gimbel.com | 30 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Special Consideration in Refractive Surgery There will always be special circumstances that may arise surrounding Refractive Surgery. Below are a few of these situations: Previous RK patients Radial Keratotomy (RK) was one of the first refractive surgeries performed at Gimbel Eye Centre in the mid 1980’s. A diamond knife was used to create spoke-like incisions on the cornea to flatten the overall curvature. Although quite successful considering the choices available at the time, many patients have experienced a moderate to high hyperopic drift over the years. They may also experience moderate fluctuations in refractive error throughout the day. Patients with this condition desiring refractive surgery should have multiple refractions performed, at different times of the day, to carefully evaluate the range of refractive errors. Choices of surgery may include Refractive Lens Exchange, Phakic IOLs, or PRK surgery depending on the circumstance. Refractive Surgery for the Unusual or High Refractive Error Sometimes the patient’s refractive error exceeds any surgical option available. In these cases, a Bioptic procedure can be considered–where multiple procedures can be combined to achieve the desired result. Usually the primary surgery will be chosen to address the majority of the prescription. For example, a +12.00-3.00 x 010 patient could consider an ICL for their hyperopia, then consider corneal refractive surgery for the remainder of the astigmatism. In these cases, the patient will likely wait 2-4 months in between the procedures to allow for stabilization, and the patient should be advised of the need of a pair of interim glasses. Refractive Surgery for Keratoconics A keratoconic patient is a good example of a potentially difficult refractive error to manage, due to corneal pathology. Often it is a challenge to work within the traditional methods of optical devices due to the refractive error. Gimbel Eye Centre has successfully treated many of these patients with Phakic IOLs. More recently, PRK with topography guided segmental ablation with therapeutic cross linking has been introduced into the practice when the refractive error is low to moderate. Although it is recognized that the refractive procedure has not halted the underlying pathological condition after cross linking, it can bring the patient’s refractive error into a more manageable range and can be used in conjunction with other optical devices. Often the overall optical quality of the vision may improve, by neutralizing the majority, if not all, of the current refractive error. Second Opinions Gimbel Eye Centre welcomes requests for second opinions on patients who have had surgery at another clinic and desire an assessment of their results/concerns. We are committed to provide an honest, but diplomatic consultation and make every effort to respect the patient’s needs and fears, as well as our colleague’s need for respectful consideration. Last Revised April 2014 31 | gimbel.com Dry Eye Assessments and Treatment The Gimbel Eye Centre offers an in depth dry eye assessment for patients suffering from dry eyes. We recommend the patient have a full eye examination by their regular eyecare provider within 12 months of the dry eye assessment. The dry eye assessment consists of multiple tests performed to isolate the diagnosis of type of dry eyes based on the different layers of the tear film. Included in this assessment is LipiView, an interferometric evaluation of the tear film and blinking patterns of the individual. Treatment options are offered based upon the diagnosis and recent research findings. Should you wish to send your patient to us for a dry eye assessment, please fill in a “Refractive Surgery Assessment and Referral Form” and indicate in the comments that you are sending the patient for a “dry eye assessment”. Prior to this assessment, patients should be advised to refrain from eye makeup, eyedrops on the day of the assessment, and lubrication ointments and gels for 24 hours. Treatment Options The treatment approach is based upon the diagnosis of type of tear film deficiency and may include the following: • Brand specific artificial tears • Punctal Plugs • Medication regimen such as steroids and/or Restasis • Warm compresses/lid scrubs • Environmental considerations • Ergonomic training • Lid debridement • LipiFlow procedure The Gimbel Eye Center can also work with the patient’s family Dr to obtain pertinent bloodwork to evaluate systemic causes of dry eyes, when appropriate. LipiFlow Procedure The Gimbel Eye Centre offers a 12 minute LipiFlow Procedure for patients suffering from lipid tear film deficiencies. The Doctor anesthetises the eye with topical medications and instills dye into the eye to visualize the line of Marx. The Doctor debrides the epithelium overlying the meibomian glands. Specialised eye cups are then placed underneath the lid and the LipiFlow device expands to heat and massage the blocked meibomian glands according to a computerized program. The essence of the procedure is to “clear out” whatever is in the blocked glands (much like clearing plaque off teeth) so that further targeted dry eye therapy can be more effective as the lipid layer is returned to a more normal consistency. It is important to properly educate the patient on the expectations and limitations of the procedure. Treatment after LipiFlow Following the LipiFlow procedure, the Gimbel Eye Centre doctor prescribes further dry eye treatment which includes a steroid medication for at least 1 month after the procedure. Patients may also return to their referring eyecare practioner for ongoing dry eye treatment. The LipiFlow may be repeated as often as once a year, depending on symptomology. gimbel.com | 32 Printed in Canada | 2014 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 Fee Information The following is a table outlining surgical fee information. All prices are per eye unless otherwise indicated. This is a general range of fees, apply to Alberta residents only, and are subject to change. Additional fees may apply for out-of-province patients, clinical testing, or complex intraocular cases. Please contact us for residents outside of Alberta. Procedure Type Total Patient Fee Primary Eyecare Provider Co-management Fee (deducted from Fee) IntraLASIK or PRK $1800 $225 IntraLASIK Xtra or PRKXtra (prophylactic cross linking with refractive laser tx) $2200 $225 Therapeutic KXL (may or may not include therapeutic laser tx) $2500 $225 AK/LRI (if primary surgery) $1395 $225 AK/LRI (if done at same time as another primary surgery) $500 — ICL/TICL $3800/$4150 $225 Cachet $4200 $225 RLE (fee depends on implant chosen) $2500-5600 $225 Cataract with Standard IOL No fee to patient (AHC covered) Charge to AHC accordingly Cataract with Premium IOL (toric, multifocal, etc.) $850-3000 Charge to AHC accordingly Bioptics (add to primary surgery fee) $1400 — Second Opinion $250 (single fee, not per eye) Secondary Corneal Surgery (when Primary Surgery was done elsewhere) $2750 $225 Secondary Intraocular Surgery (add fee to regular cost of procedure) (when Primary Surgery was done elsewhere) $1000 $225 Lipiflow Procedure $850 The fee is for the procedure only and any additional fees regarding dry eye treatment should be charged as appropriate Last Revised April 2014 33 | gimbel.com Frequently Asked Questions Will I be awake for the surgery? Yes, all of our procedures are done while the patient is awake, and topical anesthesia is used to numb the eye before surgery. Medication can be given prior to surgery to reduce anxiety. What if I can’t keep my eye open? A fine eyelid speculum is used to gently hold the eyelid open during surgery, while the other eye is covered by a shield. Try not to squeeze your eyes during surgery, and breathe normally. Will the treatment be permanent? Consider refractive surgery like resetting the prescription. Once the vision stabilizes after the initial healing period, only natural and gradual changes that would have otherwise happened may occur. Approximately 5% of patients return to correct residual refractive error. What are the success rates for surgery? For laser surgery, more than 95% of patients enjoy at least 20/40 vision without glasses or contact lenses, which is clear enough to drive and perform most daily tasks without correction. For Phakic IOL patients, more than 98% enjoy the same. Does Gimbel Eye Centre have financing available? Gimbel Eye Centre refers patients to Medicard, which provides financing options for patients seeking elective medical procedures. The patient may contact a Gimbel Eye Centre Counselor to discuss financing options or contact Medicard directly by telephone, toll-free at 1-888-689-9876, or via website, www.medicard.com. gimbel.com | 34 Printed in Canada | 2014 Refractive Surgery Assessment & Referral Form PLEASE PRINT or TYPE Assessment Date (m/d/y):_________________ Patient Name (Dr./Mr./Mrs./Ms./Miss):______________________________ Sex: M Female M Male DOB (m/d/y):________________________________ Address:____________________________________________________ City:_________________________Prov/State:___________________________ Postal/Zip:_____________________________ Telephone (res):_________________Telephone (bus):______________________ Telephone (cell):________________________ Name of Doctor Assessing:_________________________________________________________________________________ Telephone:__________________________________ City:________________________________________________________ Patient History Ocular History (e.g., Injury, Amblyopia, Previous Eye Surgery Dry Eye, Motivation for surgery, etc.): ______________________________________________________________________________________________________ Medical History:_________________________________________________________________________________________ ______________________________________________________________________________________________________ Please Check: M Diabetes M Vascular Disease M Ocular Herpes Simplex/Zoster M Pregnancy/Nursing M Collagen M Auto Immune M Other (please specify):_____________________________ List Medications, include Imitrex® (migraine), Accutane® (acne), Amiodarone® (cardiac anti-arrhythmic) &/or Flomax® (urinary flow): Ocular:___________________________________________ Systemic:____________________________________________ _________________________________________________ ____________________________________________________ Current Spectacles Rx Prism: M Yes Current Contact Lens Rx OD___________________________ OS_____________________________________ M No Refraction Date:___________________ Vertex Distance:___________________ OD M Manual Pupil Size (Diameter in dim illumination)_ M Soft OS _______________ 20/_________ ___________________________ _______________mm_______ _______________ mm_________ _________________________ ___________________________ _________________________ ___________________________ M Dilated M Undilated _________________________ ___________________________ C/D (Cup-to-disc ratio)_________________________ ___________________________ _________________________ Macula _________________________ Periphery _________________________ Pachymetry _________________________ Monovision Discussed M OS M Monovision Simulated M Auto_________________________ Anterior Segment Crystalline Lens M RGP _______________20/________ Best Corrected Visual Acuity Posterior Segment M OD OD___________________________ OS_____________________________________ If contact lenses are worn, indicate: Keratometry Readings Eye Dominance: M Yes M No ___________________________ ___________________________ ___________________________ ___________________________ Contact Lens Monovision Trial Completed M Yes M No Comments:_____________________________________________________________________________________________ ______________________________________________________________________________________________________ _____________________________________________________ Doctor Signature:___________________________________ M Gimbel Eye Centre Calgary Fax: (403) 202-3303 M Gimbel Eye Centre Edmonton Fax: (780) 452-4114 Primary Eye Care Provider Refractive Surgery Follow Up Form Patient Name (Dr./ Mr./Mrs./Ms./ Miss):_____________________________________________________________________ DOB (m/d/y):_______________________________________ Examination Date:_____________________________________ Assessing Doctor:___________________________________________________ Surgery Date: _____________Type: M LASIK M PRK M ICL M OD M Cachet M RLE M MD M Cross Linking EXAMINATION Visual Acuity Without Correction ODOS _________________________ ___________________________ Manifest Refraction _________________________ ___________________________ _________________________ ___________________________ __________________ mm Hg ____________________ mm Hg _________________________ ___________________________ Keratomerty Intraocular Pressure Ocular Medications: LASIK PRK Current Interface clear M Yes M No M Yes M No Flap smooth M Yes M No M Yes M No Flap in good condition M Yes M No M Yes M No Haze Grading (please specify) M Clear M Clear M Mild M Mild M Marked M Marked RLE / ICL Iridotomy/s patent (ICL only) M Yes M No M Yes M No IOL/ICL centred M Yes M No M Yes M No Crystalline lens grading (ICL only) M Yes M No M Yes M No Periphery intact M Yes M No M Yes M No Vaulting grading ______________________ +Vaulting _____________________ +Vaulting (Visual estimate of space between back surface of ICL and front of crystalline lens, i.e., If space is 2x central ICL thickness, then 2+ vault) Toric ICL orientation (in degrees) _______________________ Degrees ________________________ Degrees Comments or questions:___________________________________________________________________________________ ______________________________________________________________________________________________________ Treatment plan:__________________________________________________________________________________________ ______________________________________________________________________________________________________ Is the patient satisfied with the surgical outcome? M Yes M No Comments:_____________________________________________________________________________________________ Assessing Doctor’s Fax:___________________________________ Would you like a reply:_ M Yes M No Signature of Assessing Doctor:________________________________________________ FOR GEC OFFICE USE ONLY Surgeon Comments:______________________________________________________________________________________ M Gimbel Eye Centre Calgary Fax: (403) 202-3303 M Gimbel Eye Centre Edmonton Fax: (780) 452-4114 Cataract Surgery Assessment & Referral Form Patient referred for: M Cataract Assessment M Secondary Cataract/YAG laser Tx M Primary Cataract M 2nd Opinion on Previous Cataract Sx Referral Date (m/d/y):__________________________________________ Patient Name (Dr./Mr./Mrs./Ms./Miss):___________________________ Sex: M Female M Male DOB (m/d/y):_________________________________________________Alberta Health Care #:________________________ Address:______________________________________________________E-mail:____________________________________ Telephone (res):_______________________________ (bus):_______________________ (cell):__________________________ City:_______________________________________ Prov/State:___________________ Postal/Zip:______________________ If the Patient may not be reached or would have difficult answering questions, please indicate a contact person below: Name of Contact Person:_________________________________Relationship to Patient:______________________________ Telephone (res):_______________________________ (bus):_______________________ (cell):___________________________ Assessing Doctor Name:____________________________ Type of doctor: M OD M MD M OPH Address:_______________________________________________________PRACID #: _______________________________ Telephone:________________________________________ Facsimile:______________________________________________ City:_______________________________________ Prov/State:___________________ Postal/Zip:______________________ Patient Health History Ocular History (e.g., Injury, Amblyopia, Dry Eye, etc.):__________________________________________________________ ______________________________________________________________________________________________________ If Patient has had previous eye surgery, please indicate type of sx: OD_____________________________________ OS______________________________________ Name of Surgeon:___________________________________________Location:______________________________________ Date of Sx (m/d/y):__________________________________________Was a lens implanted? Please Check: M Yes M No M Diabetes M Mobility Problem M Benign Prostatic Hypertrophy M Heart M Asthma M Auto Immune Disease M Immune Deficiency M Language Difficulty M Hepatitis M Ocular Herpes Zoster M Ocular Herpes Simplex M Hearing Difficulty M Atopy M Pregnancy/Nursing M Collagen Vascular Disease M Hypertension M Other health problems or concerns (If yes, please specify): _______________________________________________________________________________________________ List medications, include Imitrex® (migraine), Accutane® (acne), Amiodarone® (cardiac anti-arrhythmic) &/or Flomax® (urinary flow): Ocular:___________________________________________ Systemic:_____________________________________________ ___________________________________________ ____________________________________________ ___________________________________________ ____________________________________________ List allergies to food (include nuts and shellfish) medications, surgical tape, eye drops, iodine &/or latex: ______________________________________________________________________________________________________ __________________________________________________ Specify if allergies are: PLEASE COMPLETE BOTH SIDES OF THIS FORM M Airborne M Contact Cataract Surgery Assessment & Referral Form cont’d Patient Name:___________________________________________________________________________________________ Does Patient have cataracts? M Yes M No If Yes, indicate: M OD M OS Does Patient have glaucoma? M Yes M No If Yes, indicate: M OD M OS Current or last IOP:_________________ OD_______ OS IOP measured by: M AT M NCT Does Patient have macular degeneration? M Yes M No If Yes, indicate: M OD M OS Any abnormalities of the cornea? M Yes M No If Yes, indicate: M OD M OS If Yes, please explain:______________________________________________________________________________________ ______________________________________________________________________________________________________ Any abnormalities of the iris? M Yes M No If Yes, indicate: M OD M OS If Yes, please explain:______________________________________________________________________________________ ______________________________________________________________________________________________________ Best Corrected Visual Acuity OD 20/________________ Current Spectacles Rx OD____________________ OS_______________________________ Does the patient wear prism(s) in his/her current spectacles? OS 20/____________________________ M Yes M No Would you prefer that our office (Calgary or Edmonton) performed follow-up care? M Yes M No M Other If Other, please specify: ___________________________________________________________________________________ Does Patient wear contact lenses? If Yes, indicate: M Hard M Yes M Soft M No M Rigid Gas Permeable M Other, please specify:______________________ M Instructed to leave out contact lenses for _______ days prior to assessment Comments:_____________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ Has Gimbel Eye Centre seen this Patient previously? M Yes M No Signature of Assessing Doctor:___________________________________________ For Office Use Only Patient ID:_____________________________________________________________________________________________ Appointment Date:_____________________________________Appointment Type:___________________________________ Comments:_____________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ M Gimbel Eye Centre Calgary Fax: (403) 202-3303 M Gimbel Eye Centre Edmonton Fax: (780) 452-4114 Primary Eye Care Provider Cataract Surgery Follow-Up Form PLEASE TYPE / PRINT Patient Name (Mr./Mrs./Ms.):_____________________________________________________________________________ DOB (m/d/y):____________________________________ Follow-Up Exam Date (m/d/y):____________________________ City:___________________________________________ Patient’s Telephone:______________________________________ Assessing Dr.:____________________________________ M OD M MD City:____________________________________ Surgery Date (m/d/y):___________________________________________ EXAMINATION ODOS Visual Acuity Without Correction _________________________ __________________________ Manifest Refraction _________________________ __________________________ Keratomerty _________________________ Visual Acuity With Above Refraction Intraocular Pressure by Slit Lamp M NCT ___________________________ _________________________ __________________________ M AT __________________ mm Hg ___________________ mm Hg AC clear M Yes M No M Yes M No Cornea clear M Yes M No M Yes M No IOL centred M Yes M No M Yes M No Posterior Capsule clear M Yes M No M Yes M No Retina Posterior Pole intact M Yes M No M Yes M No Additional Observations, Comments or Questions:____________________________________________________________ _____________________________________________________________________________________________________ _____________________________________________________________________________________________________ Is the patient satisfied with the surgical outcome? M Yes M No If No, please indicate why the patient is dissatisfied.____________________________________________________________ _____________________________________________________________________________________________________ Next visit scheduled (m/d/y):____________________________________ Would you like a reply? M Yes M No Assessing Doctor’s Fax:_____________________________ ____________________________________________________ Signature of Assessing Doctor FOR GEC OFFICE USE ONLY Surgeon Comments:_____________________________________________________________________________________ _____________________________________________________________________________________________________ M Gimbel Eye Centre Calgary Fax: (403) 202-3303 M Gimbel Eye Centre Edmonton Fax: (780) 452-4114 Refractive Surgery Monovision Form PLEASE PRINT or TYPE Assessment Date (m/d/y): ________________ Patient Name (Dr./Mr./Mrs./Ms./Miss):_____________________________ Sex: M Female M Male DOB (m/d/y):_______________________________ Address: ___________________________________________________ City: ________________________Prov/State:__________________________ Postal/Zip: ____________________________ Telephone (res):________________Telephone (bus): _____________________ Telephone (cell):________________________ Name of Doctor Assessing:________________________________________________________________________________ Telephone:_________________________________ City: _______________________________________________________ The following data is required for a monovision treatment plan: Eye Dominance: M OD M OS Final Monovision Contact lens Info: Contact Lens Power: OD __________________________ OS ____________________________________ Monovision Over-Refraction Info: CL Over-Refraction: OD __________________________ OS ____________________________________ (In other words: What monocular refraction, with the patient wearing the monovision contact lenses, gives them best corrected distance vision again? This is especially important to confirm in light of vertex changes, tear film influence, and masking of astigmatism. We are confirming patient’s desired residual myopia {usually between –0.75 and –2.50D.}) Thank you for your valuable contribution to our mutual patient’s surgical care. M Gimbel Eye Centre Calgary Fax: (403) 202-3303 M Gimbel Eye Centre Edmonton Fax: (780) 452-4114 Surgery Co-Management Guide LEADERS IN CORRECTIVE EYE SURGERY SINCE 1964 References 1. MiS, Dooley EP, Albon J, Boulton ME, Meek KM, Kamma-Lorger CS. The adhesion of LASIK-like flaps in the cornea: effects of cross-linking, stromal fibroblasts and cytokine treatment: Presented in part in British Society for Matrix Biology annual Meeting 2008, Cadiff, UK, 8-9 September 2008. Last Revised April 2014 41 | gimbel.com gimbel.com | 42 Printed in Canada | 2014