* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download STRABISMUS DETECTION AND AMBLYOPIA PREVENTION IN
Survey
Document related concepts
Transcript
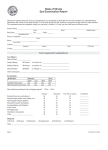
STRABISMUS DETECTION AND AMBLYOPIA PREVENTION IN PRIMARY CARE By Elizabeth Williams, BSN, RN Intercollegiate College ofNursing A Manuscript Submitted in Partial Fulfillment of the Requirements for the Degree of MASTER OF NURSING EASTERN WASHINGTON UNIVERSITY COLLEGE OF NURSING Intercollegiate College ofNursing, WSU Spokane Campus May, 2003 11 To the Faculty ofEastem Washington University To members of the committee appointed to examine the Clinical Project ofELIZABETH A. WILLIAMS find it satisfactory and recommend that it be accepted. :5~ti4Y0}~ (Chair) ill ACKNOWLEDGEMENT The guidance, assistance and support of Cindy Corbett, Ph.D, Lorna Schumann, Ph.D and Billie Severtson, Ph.D., Washington State University, Spokane, in preparation of this research paper is gratefully acknowledged. Sincere appreciation is extended to them for their time and energy for review and revisions. IV STRABISMUS DETECTION AND AMBLYOPIA PREVENTION IN PRIMARY CARE BY ELIZABETH WILLIAMS, BSN, RN Intercollegiate College ofNursing, WSU MAY, 2003 Abstract Chair: Lorna Schumann, Ph.D. Primary care providers are charged with the responsibility of identifying abnormal visual function when performing scheduled health screening of children. Providers performing pediatric well-child vision examinations are failing to diagnose 5-10% of children with amblyopia. Failure to recognize and immediately refer conditions such as amblyopia, strabismus, and uncorrected refractive errors can permanently jeopardize normal visual development. These conditions can result in poor academic performance and may progress to blindness. Because optic nerve development occurs until age 10, rapid diagnosis and treatment correlates to better outcomes, however, treatment should be pursued at all ages of diagnosis. Critical screening techniques for primary care providers and indepth information regarding referral and treatment options for clinicians and patients are reviewed. v TABLE OF CONTENTS Page SIGNATURE PAGE ii ACKNOWLEDGMENT iii ABSTRACT iv TABLE OF CONTENTS v LIST OF TABLES vi Introduction 1 Statement of Purpose . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 1 Fram.ework and Theory . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 2 Etiology and Pathophysiology of Amblyopia 4 History 5 Exam. 6 Review of Selected Research Literature . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 8 Synthesis of Research Findings 19 Management 20 Parental Information 22 Su.tnmary' . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 24 References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 25 VI LIST OF TABLES Page Definition of Terms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 29 Definition of Visual Testing Terms 30 Office Equipment for Vision Examination 33 Pediatric Eye Exanl Components . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 34 Pediatric Vision Testing Procedures To Detect Strabismus Screening and Referral Recommendations 35 . . . . . . . . . . . . . . . . . . . . . . . . . .. 37 Chronic Care Model A Pediatric Vision Screening Documentation Form B 1 STRABISMUS DETECTION AND AMBLYOPIA PREVENTION IN PRIMARY CARE Introduction The Department of Health and Human Services states in Healthy People 2010, that "vision affects development, learning, communicating, working, health and quality of life" (p 28-3). Improving the visual health of the nation through prevention, early detection, treatment and rehabilitation is currently a national priority (Healthy People, 2010). The 1994 National Health Interview Survey reported that 1% of the population under the age of 18 in the United States are visually impaired (Viisola, 2000). Visual impairment is defined as blindness in one or both eyes or trouble seeing even with glasses (Viisola, 2000). Strabismus, a misalignment of the eyes, is the most common eye condition found and occurs in 1 to 4% of the population (Viisola, 2000). Amblyopia, reduced visual acuity that develops as a result of strabismus, can cause in blindness and affects 1 to 2% of children (Viisola, 2000.) Early detection and treatment of strabismus in infancy and early childhood is critical for amblyopia prevention and vision loss because better outcomes occur when treatment is initiated before optic nerve development is completed at age 10. Children continue to go blind each year due to lack of screening by primary care providers and parents who fail to access services. Primary care providers playa critical role in achieving improvement in the visual health of the nation through early detection of strabismus and referral to ophthalmology or optometry for treatment. The purpose of this paper is to enhance primary care providers' ability to detect strabismus and amblyopia and facilitate parental access to immediate treatment. A definition of terms related to visual problems are found in table 1. 2 Framework and Theory The conceptual framework for this study was based on the Chronic Care Model (CCM) developed by Dr. Ed Wagner, M.D., M.P.H., national director of the Improving Chronic Illness Care (ICIC) program. The model was revised by a panel of national experts during a subsequent project, supported by the Robert Wood Johnson Foundation, for use in evaluating innovative programs recommended by experts. ICIC, based at Group Health Cooperative in Seattle Washington, is located at the Macoll Institute for Healthcare Innovation. The Chronic Care Model identifies elements of the health care system, individual provider issues and patient characteristics that create barriers and result in poor health care outcomes. These elements address: primary care providers who fail to provide thorough care because they are unable to follow established care guidelines due to time constraints, providers who provide fragmented care due to a lack of coordination with specialties, and patients who are not empowered to self manage their disease. The purpose of the model is to direct focus on system components to facilitate productive interactions between patients who take an active part in their care and providers who have the expertise and resources available to provide high quality care (Wagner, 1998). The Chronic Care Mode~ found in Appendix A, is multidimensional, separating the "community" and "health system" as the two major overlapping entities. Positioned below community and health system in a support location are the four essential elements of the health system. The elements are self management support, delivery system design, decision support and clinical information systems. The community and health system components all contribute 3 to expedite productive interactions between the patient and the provider or practice team located below the community and health care system (Hyatt, 2001). Community programs are valuable resources that, when identified, can provide evidence based programs in partnership with the primary care provider or health care system. Support from community programs improves patient outcomes, by enhancing the ability of the provider to detect, and manage specific medical conditions. Primary care providers or health care systems that work within the Chronic Care Model facilitate this interaction and work in tandem with the community (Wagner, 1998). Individual provider issues, when working within a chronic care model, are addressed by focusing on the health care system components of self-management, delivery system design, decision support and clinical information systems. The primary care provider is taught that to achieve self-management support, the provider should educate the patient about how to take better care of themselves to minimize complications, symptoms or disabilities. The provider should emphasize that the patient and their parents have the central role in managing their condition. Information and interventions to enhance confidence are provided to patients and their families to achieve this goal and ongoing collaborative support is made available. The delivery system design that is desired is preventive. The provider is taught to be focused on keeping a patient, as healthy as possible instead of reacting when the patient is sick (Wagner, 1998). To achieve decision support, the provider is taught that treatment decisions need to be based on explicit, proven guidelines supported by at least one defining study. Providers must 4 be exposed to current research findings and participate in continuing education. The provider should discuss guidelines with patients or patients' parents so they can make informed treatment decisions. The primary care provider must remain interactive with specialists when joint consultation is necessary. Clinical information systems assist the provider with tracking individual patients, as well as populations of patients. The provider can utilize the system to ensure that patients comply with recommended guidelines for screening and follow up exam resulting in better outcomes (Wagner, 1998). The Chronic Care Model provides a framework that facilitates the use of community resources, educates providers to enlphasize patient self-management, practice to prevent rather than react to illness, use of evidence based guidelines to manage conditions and the use of clinical information systems to improve patient monitoring. Utilizing the Chronic Care Model can improves communication between the patient and families and the practice team and results in superior clinical and functional outcomes in children with strabismus and amblyopia (Wagner, 1998). Etiology and Pathophysiology ofAmblyopia The normal visual pathway is developed by the age of2 to 3 months. To focus a visual image on the retina, all rays of light converge on the macula and retinal area. Images become sharply delineated. The ciliary bodies accomplish accommodation by contracting which allows the lens to increase in curvature and to increase refraction of light rays from near objects. This ocular convergence allows a binocular image to be maintained (Broderick, 1998). Binocular fusion is achieved by the brain. Each eye, while moving in unison, focuses the 5 retinal image on its macula and the brain fuses the image into one. If one eye has a distorted image on the retina, the brain suppresses the poor image to allow for clear vision. If suppression occurs, neurological development is interrupted causing visual impairment in the suppressed eye. (Broderick, 1998). There are three types of amblyopia; strabismic, refractive and deprivation. Strabismic amblyopia occurs in the presence of esotropia, exotropia, hypertropia or hypotropia. The visual axis misaligns the image on the retina and prevents binocular fusion. Refractive amblyopia occurs when both eyes have significantly different refractive scores. The eye that is unable to focus the image on the retina is suppressed. If both eyes lack focus, they may both become amblyopic. Deprivation amblyopia occurs when vision is never allowed to develop because the retina does not receive a clear image. Deprivation amblyopia can be the result of unilateral or bilateral congenital cataracts, corneal or vitreous opacity, severe ptosis or excessive patching (Kaw & Simon, 2001). Suppression over time results in monocular vision, eliminating peripheral vision and depth perception. History Primary care providers playa critical role in the detection of amblyopia, strabismus, and other visual disorders. A careful visual history and evaluation should be included in all well child examinations. The academy of ophthalmology and optometry recommend vision screening at the ages of newborn to 3 months, 6 months to 1 year, 3 years and 5 years (National Guidelines Clearinghouse, 1997). Comprehensive vision screening should include collecting information about the following: presenting problem or chief complaint, family 6 history of vision or eye problems, maternal and neonatal conditions that place the child at high risk for visual disorders, any parental concerns or school reports of visual abnormalities, worsening grades, poor school performance, ocular history of the patient, and dates of previous ophthalmologist or optometry examination (National Guideline Clearinghouse, 1997). Exam Primary care providers should complete a comprehensive visual examination of all children and have the ability to detect abnornw findings so that appropriate treatment referrals can be made. Table 2 lists equipment needed to perform a complete visual exam. The American Academy of Pediatrics has published pediatric vision screening guidelines that recommend the use of Snellen letters and numbers, tumbling E charts, picture tests and Allen figures to test distance acuity in children (Broderick, 1998). In addition, letter charts made up using the letters H, 0, T, V called HOTV charts, Leah Hyvarinen symbols, sterogram cards, Randot cards and Ishihara cards should be available to facilitate examination of children at various developmental stages. These tests are defined in table 3. Visual acuity at 14 feet and 20 feet, color vision results, and stereogram results should be obtained by age 3. Stereogram results are obtained with the child wearing three dimensional glasses and viewing stereogram cards such as the standard stereofly. Photoscreening using a camera or video system that documents images of the pupillary reflexes and bilateral red reflex can be utilized to confirm vision examination findings in young patients. Photoscreeening assists in making the determination to refer for amblyogenic factors, such as strabismus, medial opacities and significant refractive errors in one or both eyes. History information, visual acuity, color 7 vision, and stereogram testing could initially be obtained by office personnel checking patients in and then reviewed by the primary care provider during the exam portion of the visit. The visual exam at every age in the primary care office should include the four components listed in table 4: External inspection, penlight inspection, procedural testing and fundoscopic exam. The ability to perform certain procedures varies with age. All infants by the age of 6 months should be examined for fixation preference, ocular alignment and the presence of any eye disease (DeAngelis, Feigin, Oski & Warshaw, 1999). To assess vision in an infant, shine a bright light into the eyes, blinking indicates the infant can see. A second method is to move an object quickly towards the infant, extension of the head will occur if the infant can see. To assess for fixation preference hold the baby upright grasping the axilla with your hands and fixing the head with your thumbs. Then, extend your arms and rotate yourself with the baby slowly in one direction. The baby's eyes will open providing a clear view of the sclera, iris and extraocular movements. The eyes should look in the direction you are tlrrning and opposite direction when rotation stops (Bickley & Hoekelman, 2000). Visual acuity, stereopsis, color testing and strabismus procedures should begin by age 3. Allen or SheridanGardner cards can be used in young or illiterate children when testing for visual acuity. Stereogram testing using the stereofly cards should be initiated early but no later than age 3 to assess for binocularity. The Snellen acuity charts can be used for older children or those children that can use the alphabet (DeAngelis, Feigin, Oski & Warshaw, 1991). Specific pediatric vision testing procedures to detect amblyopia or strabismus are explained in table 5 and should be consistently performed, as early as possible, but no later than age 3. Abnormal 8 findings can be identified when performing the Hirschberg test, cover-uncover, pupillary checks and ophthalmic examination. Asymmetry, an uneven finding during testing is the hallmark symptom that should trigger concern. Specific abnormal findings requiring referral to ophthalmology or optometry are identified in table 6. Children with strabismus or any obvious ocular problem should immediately be seen by an ophthalmologist or optometrist (DeAngelis, Feigin, Oski & Warshaw, 1999). The vision screening form in Appendix B can be utilized to document exam findings. Review ofthe Literature A literature search of peer reviewed research articles was performed using the following keywords: Amblyopia, strabismus, and pediatric vision. Medline and CINAHL databases were searched from 1998 to 2003, Pubmed and Medscape databases were searched from 2000 to 2003 and additional references were identified from bibliographies. Research about amblyopia is limited and does not address the statistical occurrence of misdiagnosis of strabismus and amblyopia by primary care providers. Ophthalmology and Optometry disciplines each manage strabismus and amblyopia differently, however, there are very limited studies that address outcomes in relation to achieving acuity, binocularity and peripheral vision. Many providers utilize combinations of physical therapy, occupational therapy, chiropractic care or corneal refraction therapy to address conditions associated with strabismus and amblyopia but research has not documented a correlation between the benefit of these therapies and improved outcomes. Available research is critiqued below. Anderton et aI., (2002) using a descriptive survey design sent out questionnaires to 400 9 optometrists practicing in New South Wales to investigate methods used in examining pediatric optometry patients and the management of amblyogenic conditions. The questionnaire was constructed following published research guidelines and piloted on 10 optometrists. The instrument consisted of 17 questions in three divided sections: section A, addressed professional qualifications and practice type, section B, dealt with methods of pediatric visual assessment and section C, addressed the management of strabismus. The questionnaire asked respondents to identify the following methods used for visual acuity measurement and refraction: Leah symbols, Ffookes cube, Preferential looking cards (Teller, Cardiff), Sheridan-Gardiner test, Tumbling E, Landolt C, Broken wheel test, Sjogrens hand test, Snellen chart, autorefractor, retinoscopy (cycloplegic or near fixation). Explanations of these tests are provided in table 2. Respondents were also asked to identify whether they tested monocular acuities and binocular acuities and to indicate the methods used for binocular vision assessment, specifically, ocular motility, cover test, stereopsis, near point convergence, phoria measurement, fusional reserves, accomodative facility and or suppression tests. Finally, respondents were asked if they performed direct ophthalmoscopy, binocular indirect ophthalmoscopy, visual field testing, contrast sensitivity, color vision and or electrophysiology to test visual fimction and ocular health. Ofthe 400 questionnaires sent out to optometrists, 179 (45%) were returned. The data collected from the questionnaire was extrapolated into the statistical frequency at which respondents performed specific exam procedures and a comparison was made between children under the age of 4 and children 4 to 8 years old. Reliability and validity of the tool were not cited in this study (Anderton et aI., 2002). 10 Survey results indicated that none of the respondents had taken postgraduate courses or obtained specialty qualifications in pediatric optometry or visual development. The respondents identified that 2% of their patients were under 4 years of age and 10% were in the 4 to 8 year age group. The population estimates for New South Wales, indicated that 5% of the population is lmder 4 and 5% of the population is aged 4 to 8. Most of the respondents indicated that they did not use tests specifically designed for pediatric visual acuity assessment. Monocular acuity, a critical assessment used to diagnose unilateral strabismus or amblyopia was not evaluated by 15% ofthe respondents in children aged less than 4 and not evaluated by 1% ofthe respondents in children aged 4 to 8. However, for patients in both age groups, binocular visual function was assessed by ocular motility 94% of the time, cover testing 96% of the time, stereopsis testing 73% of the time, and a measure of near point convergence 80% ofthe time. Most respondents reported that amblyogenic factors such as strabismus must be detected before the age of eight for treatment to be most effective. They reported that they would not delay treatment and would use refractive correction, occlusive therapy, prism therapy or refer to another provider for care. Respondents were asked for their comments and observations about pediatric visual assessment, but the Slunmary of findings did not document any opinions regarding specific recommendations for screening (Anderton et aI., 2002). The study findings are limited by the use of a questionnaire without documented reliability and validity. Although the questionnaire tool was trialed by optometrists, revisions were not cited. The findings cannot be generalized as a convenience sample was utilized with all optometrists located from within the same geographic area who were without specialized 11 training in pediatrics. However, the study did yield a 45% response rate which is valid for analysis. Study findings are important because the information indicates that primary care providers may have the opportunity to screen many children under the age of 8 who are not screened by an optometrist. Study findings also indicate that exam procedures and techniques among optometrists vary and this lack of standardization may result in a failure to detect strabismus or amblyopia. Therefore, primary care providers need to continue to be vigilant for amblyogenic risk factors despite previous examination by optometry. Optometry respondents did not believe deferment of treatment to be beneficial for children and usually included ophthalmology as a co-manager when strabismus is diagnosed (Anderton et al., 2002). Many areas of the nation have instituted 100% screening programs to improve strabismus and amblyopia detection. The "See to Learn" program sponsored by the Kansas Optometry Association allows every three year old to be assessed for free by optometry specialists (Kansas Vision Developmental Center, 2003). Primary care providers should anticipate an ophthalmology referral rate of approximately 8% of their caseload and should educate all parents regarding the benefits of obtaining a comprehensive exam by the age of 3 (Azari, Bertakis, Callahan & Robbins, 2001). Preschool vision screening programs have been studied to determine how well strabismus and refractive errors are detected when trained public health nurses administer tests of visual acuity, stereoacuity and ocular alignment. Bobier, Bryant, Martin, & Robinson (1999) studied 3,434 children over a 3 year period and found that 28.9% of children failed the vision screening 12 in year one, 34.7% failed in year 2 and 25.5% failed in year 3. Vision screening tests were conducted by 9 different public health nurses who targeted all children registered for kindergarten. The public health nurses were trained yearly to conduct visual acuity and ocular alignment. During the second year of screening steroacuity testing was added. If the child failed a component of the screening they were referred to an eye care practitioner of their choice. Children who were unable to complete the screening were also referred to an eye care practitioner. For each child that failed the exam the nlll'Se referred the next child in line that passed the exam as a control. The eye care practitioners were then required to file reports that described the major results of their examination. Personnel from the county health unit compared each practitioner's report to the screening result. Data from both sources were entered into a computer data base and compared. What constituted a "visual problem" was defined as the presence of any strabismus, anisometropia, a difference of 1 diopter or more of refractive error between the eyes, hyperopia of2 diopters or more in either eye, myopia of one diopter or more in either eye and astigmatism of more than 1 diopter in either eye. During the three year study, 118 children passed the screening by the public health nurse, but had vision problems as defined above and identified by examination of the control group by the eye care practitioner. During year 2 of the study, stereoacuity assessment was added to the screening procedure and the number of children who passed the public health screening with vision problems decreased. Sensitivity of visual acuity plus Hirschberg testing in year 1 was 69.9%, in year 2 with stereoacuity 70.9% and year 3, 60.4%. Specificity testing in year 1 was 75.6%, in year 2 with stereoacuity 69.6% and year 3, 79.7% 13 (Bobier et aI., 1999). The study findings cannot be generalized to the public as a convenience sample was utilized with analysis of children from the same geographic area. A standardized definition of "visual disorder" strengthens validity. The sensitivity and specificity findings are weakened since the number of controls referred was never equal to the nurrlber of screening failures referred. Strength in the results can be found in the sample size of3,434 children with a mean age of 51 to 54 months (Bobier et aI., 1999). The study results indicate that providers are failing to detect vision problems before kindergarten due to the poor quality of screening procedures or parental failure to access examination for their child. The study also demonstrates that quality visual examinations can improve the rate of strabismus and amblyopia detection. Stereoacuity testing appears to playa very important role in improving this detection (Bobier et aI., 1999) Vision screening, although critical, is difficult in the preschool population because of developmental norms such as failure to follow directions, inability to fixate for a prolonged period of time, and refusal to cooperate with the examiner. Past randomized surveys of vision screening practices among pediatricians in Illinois revealed that comprehensive vision examinations of children are difficult to perform due to "inadequate time" and "children too young" (Berry et aI., 2001). Photoscreening devices have been developed to improve vision screening in children. Photoscreening instruments are noninvasive devices that can detect refractive errors, cataracts, medial opacities and misalignment ofthe eyes, but require minimal cooperation from the child. 14 Berry et aI's., (2001) study compared the use ofa photoscreening device in a total of 51 preschool children (experimental group) against ophthalmic examination (control group). The children had developmental delays, behavioral problems or medical problems. Every preschool child in the study was photoscreened and then given a complete ophthalmic examination. Children. were photoscreened using the instructions in the manual that accompanies the MTI photoscreener. The lights in the exam room were reduced so that the subject's face was barely visible. Using the aiming lights, the camera was aimed at a spot in the center of the forehead and 1.25 inches above the center of the pupils. The subject's attention was then captured by activation of fixation lights or sound. Once alignment and fixation was obtained the shutter was triggered. The process was repeated after the flash recharged for a second photograph. The criteria for photographic quality was symmetric pupil size, appropriate camera fixation, symmetric corneal reflections and a good view of both eyes and cornea. Pictures were retaken, immediately, ifreview of the photograph did not meet the specified criteria. Eye photos were examined, coded and interpreted by a registered nurse who did not have knowledge of medical record or previous examination findings. A pediatric ophthalmologist, then performed a complete eye examination consisting of Snellen or Allen optotype recognition, Teller visual acuity, or assessment of fixation reflex, measurement of ocular alignment both distance and near, cover/uncover testing, and evaluation of pupils. These procedures are defined in table's 2 and 5. The photoscreening and ophthalmology examination findings were entered into a computer data base and interpreted using a standardized measuring tool with four categories. 15 Category A listed failure of both vision screening and ophthalmology evaluation as a true positive, category B listed failed vision screening and passed ophthalmology evaluation as a false positive, category C listed passed vision screening, but failed ophthalmology evaluation as a false negative, category D listed passed vision screening and ophthalmology evaluation as a true negative. Sensitivity is the probability that the screening test will be positive when an abnormality is present. Specificity is the probability that the screening test will be negative when an abnormality is not present. When compared to complete ophthalmic examination, the Medical Technology Incorporated photoscreener was found to have a sensitivity of 83% and specificity of 68% (Berry et aI., 2001). The study findings were limited by the use of a convenience sample. Additional studies with larger sample sizes need to be pursued to examine if interventions such as additional technician training or repeat photographs of abnormal findings can improve sensitivity and specificity. Also, the sample selection which targeted non verba~ uncooperative and developmentally delayed children may have impacted sensitivity and specificity. The use of photoscreening devices in an office setting can be an important tool to stimulate learning and reinforce the ability of the primary care provider to adequately screen patients for strabismus (Berry et aI., 2001). A randomized, controlled trial study by Harrod, Harvey, Northstone, Sparrow and Williams (2002) investigates whether early treatment of amblyopia is more effective when initiated at younger ages. The convenience sample of3,490 children were born to parents during the last 6 months of a previous longitudinal study of parents and their siblings in Avon, England. This study compares a group of children who received intensive orthoptic screening 16 at ages 8,12, 18,25,31 and 37 months with a group of children who receive orthoptic screening at age 37 months only. Prevalence of amblyopia and visual acuity in the worse seeing eye was analyzed at 7.5 years of age in this longitudinal study. All 3,490 children were invited to attend the final examination; however only 1,929 arrived, of which 15 were excluded based on developmental delay or organic ocular pathology. The parents of the 1,914 children examined at 7.5 years completed a questionnaire that addressed specifics regarding previous ophthalmic treatment with eye patching. Random assignment of3,490 children into a control or intensive group was performed. Children were allocated into different arms ofthe study according to the last digit in the mother's date of birth. The intensive group was chosen using the numbers 1, 3, and 5 the control group was chosen using the numbers 2 and 4. The numbers from 6 through 9 were not utilized for the randomization process. The orthoptists did not know the mother's dates of birth or how the allocation was carried out (Harrod et aI., 2002). The results ofthe study documented that the prevalence of amblyopia was 1.5% in the intensive group and 2.7% in the control group at the age of7.5 years. Prevalence rates at ages 8,12, 18,25,31 and 37 months were not reported. Residual amblyopia, despite treatment, was more prevalent in the control group (10/40) than the intensive group (3/40). Visual acuity in the amblyopic eye was significantly better for treated children in the intensive group with a mean acuity of 0.15 LogMAR (Log of the Minimum Angle of Resolution) units, than in the control group with a mean acuity of 0.26 LogMAR units. The LogMAR is used to determine the geometric mean of the Snellen values. This is necessary because visual acuity chart lines 17 progress in size on a logarithmic scale. Using the arithmetic mean of the decimal Snellen value can overestimate the visual acuity mean line on the chart. The LogMAR value is calculated as -Log(Decimal Acuity). Children screened early can see an average of one line more with their amblyopic eye than children screened at 37 months after treatment. More children in the intensive group (19/40) received eye patching treatment before the age of3 than in the control group (5/40). The study suggests that early treatment is more effective than later treatment for amblyopia (Harrod et aI., 2002). Study limitations include a lack of documented reliability and validity in regards to orthoptic examinations and treatment. The questionnaire has no documented reliability and validity. Generalizability to the general public was strengthened by the randomized, controlled study design and large sample size. The Borja et aI., (2002) study analyzed information obtained by questionnaire from a previous national surveillance study performed for 24 months from July, 1997 to July, 1999. All ophthalmologists in the United Kingdom were asked to complete a questionnaire on every patient who had unilateral amblyopia and a corrected acuity of worse than 6/12 in the amblyopic eye, or newly acquired loss of vision in the nonamblyopic eye for any reason resulting in acuity worse than 6/12 or visual field impairment that restricted driving. Visual field impairment specifications were not addressed for those subjects aged 16 years or less. The questionnaire required the ophthalmologist to report detailed information about demographics, diagnosis, the date and context of how the vision loss in the nonamblyopic eye was detected, the level of visual function, the cause of vision loss in the nonamblyopic eye and 18 past and present management. Over a 24 month period, 370 cases were identified. One year after the initial report was completed the surveillance team sent a second questionnaire to the ophthalmologist requesting information on changes in visual functions, management, and outcomes such as employment status. This study extrapolated and analyzed information about 254 of the 370 subjects, aged 11 years or older, who were without any other disorder affecting their amblyopic eye. This study calculated the improvement in acuity in the amblyopic eye one year after initial presentation of symptoms. The Snellen classification was used for analysis. A gain of two lines or more of Snellen acuity was defined as a clinically significant improvement. Increased acuity in the amblyopic eye was reported in 19% of people and worsening acuity in the amblyopic eye was reported in 8% of people. Several factors were found to be associated with this subsequent improvement in the amblyopic eye. The greater severity of visual loss in the nonamblyopic eye, and the younger the age at presentation of amblyopia, together with better previous acuity in the amblyopic eye and new optical treatment all correlated to higher rates of improvement in the amblyopic eye, despite worsening acuity in the nonamblyopic eye. Study results indicated that amblyopia can be improved in patients after the age of 11 (Borja et al., 2002). Study findings were limited by vague information about the questionnaire and failure to identify reliability and validity information. Univariate and multivariate statistical analysis were provided for each predictive factor to substantiate associations with acuity outcomes in the amblyopic eye. The study utilized a convenience sanlple, which limits the ability to generalize 19 findings to the public. However, it is significant that this specialized population was reported to have improvement in visual acuity in the amblyogenic eye after age 11. Optic nerve development is thought to be complete by age 10. The study findings demonstrate the need for primary care providers to refer all children, regardless of age for treatment of strabismus and amblyopia. Synthesis ofResearch Findings Anderton et aI., (2002) identified a lack of consistency in exam procedures among optometrist in New South Wales and estimated that optometrists were seeing approximately 50% of children aged 4 years or younger during the critical time point for strabismus and atrlblyopia detection. Bobier, Bryant, Martin & Robinson (1999) found that approximately 25% of kindergarten children failed vision screening performed by trained public health nurses and that stereoacuity testing significantly improved the sensitivity of the testing. These study findings suggest that vision examinations performed by some providers lack the components required to provide adequate detection of amblyopia and strabismus. The chronic care model calls for a delivery system design that emphasizes keeping patients healthy rather than responding to illness and the use of community screening programs when available. Standardized examination guidelines based on current research findings need to be developed and utilized. Primary care providers should interact closely with optometrists and ophthalmologists to ensure quality examinations and management of strabismus and amblyopia. Harrod, Harvey, Northstone, Sparrow and Williams (2002) found that children screened 20 and treated for strabismus and amblyopia at multiple time points before the age of 37 months can see better than children who are screened after 37 months. Borja et aI., (2002) found that visual acuity improvement occurs in patients over the age of 11 with treatment. The Chronic Care Model encourages primary care providers to remain educated about current research findings, which suggest intensive screening for amblyopia and strabismus should occur before the age of3 to ensure the best outcomes. However, referral should be made for amblyopia and strabismus treatment in patients at all ages to ensure that the patient maintains the maximal functional level. Management Evidenced based guidelines should be written to guide the primary care provider through action steps designed to improve the detection and management of strabismus and amblyopia. A review of literature is necessary to understand which treatment options result in the best outcomes. Treatment for strabismus will improve the prognosis for achieving visual function and good cosmetic results. The first goal of treatment for strabismus is to obtain good visual acuity in each eye. The treatment usually prescribed is correction of the refractive error followed by patching of the good eye to stimulate optic nerve development in the suppressed eye. Occlusion therapy is continued until the best visual acuity is reached. The second goal of treatment is correction of the strabismus. Miotic therapy, corrective lenses, orthoptics vision therapy and or surgery are all utilized to achieve this correction. Vision therapy is provided by developmental optometrists who are board certified in the diagnosis and treatment of children's visual disorders. Surgery on the extraocular muscles is performed by an 21 ophthalmologist-(Gellis & Kagan, 2002). The chronic care model encourages the provider to maintain a close interaction with all specialists involved in the care. A team approach to care is essential because complex treatment options may need to be explained to the patient and or parents to ensure that self management decisions will result in good outcomes. A retrospective review of records performed by FitzGerald and Krumholtz (1999) investigated outcomes related to treatment modalities in patients diagnosed with refractive amblyopia. A protocol for treatment of refractive amblyopia was developed and distributed to all pediatric clinical doctors within the State College of Optometry. The clinical setting consisted of students with supervising clinicians who verified all findings. The guidelines required an exam visit 4 to 6 weeks after initial diagnosis and again in 2 to 4 months. Visual acuity and binocular testing were required at every visit. For a period of 6 months, all pediatric patients with a new diagnosis of unilateral refractive amblyopia were retrieved and the patient was then tracked for 6 months from diagnosis. The olitcome analysis was limited to two areas: visual acuity and stereopsis. Improvement was defined as an increase of at least 20 seconds of arc on the stereopsis test and at least a two line improvement in visual acuity on the Snellen chart. The convenience sample obtained was 78, consisting of 44 male slLbjects and 34 female subjects. There were 3 patients aged 0 to 1 yr 11 months, 24 between the ages of2 and 5 years 11 months, 31 between the ages of 6 and 8 years 11 months, and 20 patients in the 9 to 14 year old category. Four treatment modalities were offered to these patients: no intervention, optical correction only, or optical correction with a patching regimen and vision 22 therapy. The sample was reduced to 52 patients because 4 patients did not receive any treatment and 22 subjects did not attend the follow up visit or had erratic attendance for vision therapy. Optical correction alone was utilized as treatment for 17 patients, optical correction and occlusion was utilized by 23 patients, and 12 patients received optical correction and or patching in conjunction with vision therapy. Results are not reported for the 4 patients who did not receive any treatment (FitzGerald & Krumholtz, 1999). The study found that optical correction alone increased visual acuity in 41 % of the subjects and 18% demonstrated an improvement in stereopsis. The optical correction and patching group demonstrated a 69% improvement in acuity and 30% increase in stereopsis. The vision therapy group showed a 67% improvement in visual acuity and a 67% increase in stereopsis. The study results indicate that patching alone can improve visual acuity, but stereopsis (binocular acuity) is improved at a higher rate when vision therapy is added to the treatment regimen (FitzGerald & Krumholtz, 1999). The study findings would have been strengthened with the inclusion of the record data gathering form from the patient records. Also, the study would be more complete with the inclusion of the follow up results on the children who chose no treatment. However, validity was established with the stated definition of improvement in visual acuity and stereopsis. The findings cannot be generalized to the public, as a convenience sample was utilized and the sample size was small. Parental Information Primary care providers should encourage parents to investigate treatment options for 23 visual disorders. There is a national nonprofit organization established by parents dedicated to raising public awareness about vision. State chapters can be located by calling 1-800PAVE988; email: [email protected]; or access the internet web page at www.visiontherapydirectory.com. Amazon.com has many books about the myths of20/20 vision and strabismus and amblyopia. Vision therapy is usually supervised by the behavioral optometrist, but carried out by a trained vision therapist. The frequency and length of treatment needs to be discussed. If parents choose to investigate vision therapy, the primary care provider should advise parents to obtain the following information from potential vision providers. The frequency and length of treatment needs to be discussed. The cost and length of sessions should be discussed. How often does the vision therapist and optometrist conference regarding progress or problems? Does the office provide the option of home computerized therapy and if so, what is the cost? To identify health insurance coverage, parents should obtain the diagnosis and ICD 9 from the provider and contact the company to ask "Do you cover vision therapy services for the diagnosis of X, ICD 9 code X, for my child who is X years of age. Be aware that age limitations for the benefit may exist. What is the benefit amount per session? Is a preferred provider benefit available? What is the plan maximum? Many insurance companies do not cover vision therapy. Vision therapy can result in multiple contact lens and eye glass prescription changes. Parents should be advised to investigate the most inexpensive places to purchase glasses and contact lenses. Typically, the behavioral optometrist is unable to provide contact fitting 24 services, which should be done on a yearly basis. Disposable contacts may be the most cost effective. Summary The Chronic Care Model emphasizes the benefit of working in partnership with community entities, such as the "see to learn" program that provides free screening for strabismus and amblyopia. The primary care provider and the patient both benefit from utilization ofthese resources. The Chronic Care Model encourages primary care providers to follow a delivery system design based on detection and prevention as opposed to reactionary responses to acute conditions. Support for participation in activities that promote expertise in the performance ofquality history, physical and examination ofthe visual system are necessary to reduce the incidence of amblyopia. Access to the randomized amblyopia treatment studies that are currently in progress will be integral to the creation of quality management guidelines. Coordination with optometry and ophthalmology services is vital because ofthe complexity of treatment options. Patients and their parents will require extensive information to successfully self manage the treatment. Primary care providers who recognize the need for comprehensive vision examination and who refer all children with amblyogenic characteristics to eye specialists can facilitate change by eliminating amblyopia caused by strabismus. Providers must recognize that delays in diagnosis and referral can permanently impair visual health. Providers who are knowledgeable about visual impairments, skilled in detection, and who make referrals in a timely manner, will improve the visual health ofthe nation. 25 Reference List American Foundation for Vision Awareness. (2001). A nurse's guide to children's vision and learning. (1 st ed.). [Brochure]. St. Louis, MO: B. Edwards. Anderton, P., Kim, H., Kim, J., Lee, M., Suttle, C., & Wong, R. (2003). A survey of pediatric visual assessment by optometrists in New South Wales. Clinical and Experimental Optometry, 86, (1), pp. 19-33. Azari, R., Bertakis, K., Callahan, E., Robbins, J. (2001). Predictors ofpatient referrals by primary care residents to specialty care clinics. Retrieved April 3, 2003, Fronl http://www.stfm.org/fmhub/Fullpdf7march01/crm.pdt: Bane, M & Beauchamp, G. (2001). Update on vision screening. Retrieved March 24, 2003, From http://www.revophth.com/2001/march01pediatricpatient.htm. Berry, B., Duthie, M., Flynn, J., Schiffman, J., Siatkowski, R., & Simons, B. (2001). Preschool vision screening using the MTI-photoscreener. Pediatric Nursing, 27, (1), pp. 27-34. Bickley, L. & Hoekelman, R. (2000). Physical exam and history taking. (3 rd ed.). Philadelphia, PA: J.B. Lippincott Co. Bobier, W., Bryant, L., Martin, E., & Robinson, B. (1999). Measurement ofthe validity of a preschool vision screening program. American Journal ofPublic Health, 89, (2), pp. 193-198. Borja, M., Eggitt, I., Logan, S., Rahi, J., Taylor, D., & Timms, C. (2002). Prediction of improved vision in the amblyopic eye after vision loss in the non-amblyopic eye. The 26 Lancet, 360, 621-622. Broderick, P. (1998). Pediatric vision screeningfor the family physician. Retrieved March 26, 2003, From http://www.aafp.org/afp/980901ap/broderic.html. VA HIV collaborative chronic care model. (n.d.). Retrieved April 10, 2003, From http://www.qualityschlar.com/TWIV sNA%20HIVN A%20model%20for%20effective%2 O. DeAngelis, C., Feigin, R., Oski, F., Warshaw, J. (1990). Principles and practice of pediatrics. (4th ed.). Philadelphia, PA: J.B. Lippincott Company. Edelman, C. & MandIe, C. (2002). Health promotion throughout the lifespan. (5 th ed.). St. Louis, MO: Mosby. Eggitt, I., Logan, S., Rahi, J., Taylor, D., & Timms, C. (2002). Risk, causes, and outcomes of visual impairment after loss of vision in the non-amblyogenic eye: a population based study. The Lancet, 360, 597-602. Krumholtz, I., FitzGerald, D. (1999). Efficacy oftreatment modalities in refractive amblyopia. Journal ofthe American Optometric Association, 70, (6), pp. 399-404. Gellis & Kagan. (2002). Current Pediatric therapy. (17th ed.). Philadelphia, PA: W.B. Saunders. Halle, C. (2002). Achieve new vision screening objectives. The Nurse Practitioner, 27, (3), pp. 15-31. Harrod, R., Harvey, I., Northstone, C., Sparrow, J., & Williams, C. (2002). Amblyopia treatment outcomes after screening before or at age 3 years: Follow up from randomized 27 trial. BMJ, 324, 1549-1551. Hyatt, J. (2001). Integrating disease management across multiple disease states. Retrieved April 8, 2003, From http:www.kpcmi.org/presentations/HO-IntegratingDM-NMHCC82001.pdt: Kansas Vision Developmental Center. (2003). Children's vision information network: Lazy eyes. Retrieved February 28, 2003, From http://www.childrensvision.com/lazy_eyes.htm. Kaw, P. & Simon, J. (2001). Commonly missed diagnoses in the childhood eye examination. American Family Physician, 64, (4), pp. 623-628. Mills, M. (1999). The eye in childhood. Retrieved March 21,2000, From http://www.aafp.org/afp/99090 1ap/907.html. National Guideline Clearinghouse. (1997). Pediatric eye and vision examinations. Retrieved August 29, 2002, From http://www.summary.asp?guideline=OO1211 &summary_type=briet: National Guideline Clearinghouse. (1997). Pediatric eye evaluations. Retrieved August 29, 2002, From http://www.summary.asp?guideline=000406&summary_type=briet: Newell, F. (1992). Ophthalmology principles and concepts. (7th ed.). St. Louis, MO: Mosby Ohio KePRO. (2002). Chronic care model components and change concepts. Retrieved From http://www.ohioKeproinc.com/providers/HCQIP/change%20packet%20CD/QualitYOA»20. U.S. Department of Health and Human Services. (2000). Healthy people 2010. (Conference Ed.). Washington, DC: Author. 28 Virtual Naval Hospital. (2003). Put prevention into practice: Clinician's handbook of preventive service, 2nd edition: children and adolescents screening. Retrieved February 28, 2003, From http://www.vnh.org/PreventionPractice/ch11.html. Viisola, M. (2000). Statistics on children with visual impairments. Retrieved April 3, 2003, From http:www.lighthouse.org/edstats_2000.pdf. Wagner, E. (1998). Improving chronic illness care. Retrieved April 8, 2003, From http:wwwimproving chroniccare.org/change/modeVcomponents.html. Weber, J. (2000). Nurses' handbook ofhealth assessment. (4th ed.). Philadelphia, PA: J.B. Lippincott Company. Wong, D. (1999). Whaley & wong's nursing care ofin/ants and children. (6th ed.). St. Louis, MO: Mosby. 29 Table 1 Definition ofTerms Amblyopia A reduction in vision acuity in one or both eyes not attributed to structural or pathological anomalies. It is not correctable by refractive means and results from a developmental abnormality of the central visual pathway. Binocular Coordination The ability to use both eyes together. Stereopsis (Binocular depth perception) The ability to judge relative distances of objects and to see and move accurately in three dimensional space. Strabismus A misalignment of the eyes. Four types: Esotropia, exotropia, hypertropia, hypotropia. Esotropia While one eye looks straight ahead, the misaligned eye looks toward the nose. Exotropia While one eye looks straight ahead, the misaligned eye looks away from the nose. Hypertropia While one eye looks straight ahead, the misaligned looks upward. Hypotropia While one eye looks straight ahead, the misaligned looks downward. American Foundation for Vision Awareness 30 Table 2 Definition of Visual Testing Terms Snellen Letters and Number Test. Square black symbols that uses letters or numbers of the English alphabet for testing at 20 feet. For testing acuity of distant vision; The letters vary in size in such a way that each one sub tends a visual angle of5' at a particular distance (Whaley & Wong, 1999). Tumbling E Charts Square black symbols of the letter E used in such a way to measures visual acuity in children. Uses the capitol E pointing in four directions; children "read" the chart by showing the direction ofthe letter E or using a large duplicate E to match the chart E at 20 feet (Whaley & Wong, 1999). Allen Figure Test Picture cards of a tree, birthday cake, horse and rider, telephone, car, house, and teddy bear used to test visual acuity at 15 feet in children who cannot read but can recognize pictures (Whaley & Wong, 1999).. HOTV Charts A chart with the letters H, 0, T & V for testing visual acuity at 10 or 20 feet. The child names the letters on the chart or matches them to a demonstration card (Whaley & Wong, 1999). Lea Hyvarinen Test The child identifies figures on a wall chart by matching the picture in the Lea book. The Lea book is a spiral bound book of flash cards of a house, apple circle and square in different sizes (Whaley & Wong, 1999). Stereogram Test A diagram or picture which represents objects in such a way as to give the impression of relief of solidity; also a stereograph (Newell, 1992) 31 Randot Test The Randot tests the ability to identify six geometric forms from random dot backgrounds. The figures cannot be identified without glasses (Newell, 1992) Ishihara Test A test for color vision deficiency that utilizes a series ofpsuedoisochromatic plates on which numbers or letters are printed in dots of primary colors surrounded by dots of other colors; the figures are discernable by individuals with normal color vision (Newell, 1992) Preferential Looking Cards (Teller, Cardiff) Selection of preferential looking pictures designed to measure acuity in toddlers aged 13 years and in individuals with intellectual impairment. The calm infant is held in front of two screens of matching luminance, one displays a grating pattern, the other displays a blank field. Infants prefer to look at the pattern and visual acuity is estimated by the hidden examiner who estimates the stripe width seen by the infant (Newell, 1992). Sheridan-Gardiner Test A test that uses geometrical shapes, letters or patterns in decreasing sizes to test visual acuity in a child who is illiterate or below reading age. The child and examiner are spaced 6 meters apart. The child is then asked to point to identical patterns on a chart held at reading distance (DeAngelis, Feigin, Oski & Warshaw, 1990). Landolt C The Landolt broken ring is a round black symbol with a break in the ring that subtends a 1 minute angle and the entire ring subtends a 5 minute angle. It is used to test visual acuity in preschool children and illiterates. The child stands 5 meters away and identifies the location of the gap in the ring; top, left, right, or bottom. The ring is rotated over multiples of 45 degrees on the chart. Commonly used in research studies (Newell, 1992). 32 Broken Wheel Test An acuity test produced by Bemell Corporation. The child using his or her finger points to the broken part on the car (Newell, 1992) Sjogren Hand Test A test for visual acuity using isolated hand charts (Newell, 1992) Auto Refractor An instrument that automatically measures the deviation of rays of light when passing from one transparent medium into another of different density (Newell, 1992). Retinoscopy (Cycloplegic, Near Fixation) The objective method of determining the refraction ofthe eye by observing the movements of the reflection of light from the eye by means of ophthalmoscope (Newell, 1992). 33 Table 3 Office Equipment For Vision Examination Tools Acuity Charts Miscellaneous Ophthalmoscope Snellen letter charts Polarized glasses - 3 dimensional Penlight Numbers charts Stereogram cards Adhesive Occluder Tumbling E chart Randot cards Plastic Occluder Titmus slide letters HOTV Ishihara color vision cards Stationary target Allen Figures Puppet Photoscreening Camera Leah Hyvarinen Symbols 34 Table 4 Pediatric Eye Exam Components External Inspection Penlight Inspection Procedures Fundoscopic Exam Lids Conjunctiva Peripheral Vision ck Red Reflex Lashes Sclera Visual Field ck Optic Disc Lacrimal gland Iris Accommodation Retinal Arteries Tear Duct Pupillary Response Alignment Veins Orbital protrusion Cornea Craniofacial configuration Weber, 2000 Arteries Macula 35 Table 5 Pediatric Vision Testing Procedures to detect Strabismus Name of Test Procedure Peripheral Vision Check Examiner faces client at a distance of2-3 feet. Client and examiner look directly ahead and covers the eye directly opposite each other. Client and examiner should report seeing object at the same time as it approaches the periphery. Visual Field Examiner asks client to follow an object as it is moved through the six cardinal fields of vision. Eyes should move smoothly throughout the fields. Eye jerking is abnormal. Accommodation Client should be directed to stare at an object 3-4 feet away. Examiner moves the object toward's the nose. Pupils should converge and constrict as object moves in. Pupil responses should be uniform. Alignment. CoverlUncover. Have the client focus on a stationary target. The examiner places a hand or cover in front of one eye and observes the other eye. The observed eye should not move and the covered eye should not move as cover is removed. Movement is abnormal and demonstrates the presence of strabismus. If the child moves to avoid occlusion refer. 36 Pupillary Response Check direct pupil response by asking the client to look straight ahead. The examiner approaches each eye with a penlight from the client's side. Illuminated pupils should constrict. Consensual pupil response is checked by following the same procedure and noting if the pupil opposite to the one illuminated constrictssUnuhaneously. Corneal Light Reflex Have the client fixate on a penlight 2 feet away; shine the light directly in eyes and observe the light reflection. Displacement of the light reflex from the center of the pupil or asymmetry demonstrates abnormal alignment and indicates strabismus. Red Reflex Darken the room, client should have eyes open voluntarily. The ophthalmoscope is held to the examiner's eye and arm's length from the client's eyes. The red reflex exam is rated as normal when the reflections of the two eyes are seen as equivalent in red-gold color, intensity, and clarity and there are no opacities or white spots within the area of either or both the red reflexes. Lack of red reflex means the client has a cataract or is blind. (Virtual Navy, 2003) (Weber, 2000) 37 Table 6 Screening and Referral Recommendations Age Screening Method Newborn to 3 months Red Reflex 1 month Indicators Requiring Eva) I Abnormal or Asymmetric Corneal Light Reflex Asymmetric Inspection Structural Abnormality Fixation Poor following Intermittent strabismus Constant strabismus Acuity 20/400 to 20/600 Deviation Horizontal follow to midline normal alignment Acuity 20/300 2 months Vertical following to midline normal alignment 6 months to 1 year old Red Reflex Abnormal or Asymmetric Corneal Light Reflex Asymmetric Alternate Occlusion Failure to see object equally Inspection Structural Abnormality Visual Acuity 20/20 to 20/30 Binocularity well developed Fix and Follow with each eye Failure to fix and follow Visual Acuity 20/50 or worse or difference of2lines between eyes Red Reflex Abnormal or Asymmetric Corneal Light Reflex Asymmetric CoverlUncover Ocular RefixationIMovement 3 years old 38 5 years old Older than 5 years Stereoacuity Failure to identify random dot or Titmus stereogram Inspection Structural abnormality Visual Acuity 20/30 or worse or difference of2lines between eyes. Red Reflex Abnormal or Asymmetric Corneal Light Reflex Asymmetric CoverlUncover Ocular RefixationIMovement Stereoacuity Failure to appreciate random dot or Titmus stereogram Inspection Structural abnormality Visual acuity 20/30 or worse, or 2 lines of difference between the eyes Corneal light reflex Asymmetric CoverlUncover Ocular refixation movement Steroacuity Failure to appreciate steropsis Red Reflex Abnormal or asymetric Inspection Structural abnormality American Academy of Ophthalmology, 1997. Virtual Naval Hospital, 2003. 39 e ... ······· (~':;:-:~t Support ........................................................... H..; alth System ......... Organization of Health Care Delivery System Design Clinical Information Systems "",.. "" ..., ...... , ~ Informed, Activated Patient Functional and Clinical Outcomes -Sa tisfaction -Clinical Measures -Cost -External Review Measures . . . ..--,,///-/ 40 I I I I AppendixB I : Pediatric Vision Screening Documentation Form :EXAM: Newborn-3 month_ _ 6 month-1 yr _ _ 3 yr_ _ 5 yr _ Yearly after 5 yrs /Age Ophthalmology/Optometry last exam date . Date of Referral Optician/Ophthalmologist _ _ I :mSTORY: :Presenting/Parent Concerns: I _ Patient Medical Hx Birth Hx MatemalHx Family Ocular Hx Diabetes Juvenile RA Neuro-degenerative dx Premie 28wks/< Steroid admn Oxygen at birth Rubella Toxoplasmosis Herpes/CMVIHIV Glasses Strabismus Ambylopia Retinoblastoma Cataract Glaucoma SYMPTOM SCREENING: Fatigue w/reading Worsening Grades Poor academic performance Head tilting Closing/blocking one eye Loss of place w/reading Failure to recognize same word in next sentence Omits, inserts or rereads letters/words. Avoidance of near work Letters/lines run together or jump around Letter reversals after second grade Poor eye hand coordination Jerky eye movement Eyes Crossed/turned inlout Squinting Eye rubbing Excessive blinking Tearing w/computer use Blurred/double vision Headache Dizziness Nausea VISUAL ACUITY: Uncorrected: (20 ft) Corrected: (20 ft) N ear acuity (14 ft): Color vision: I right eye right eye right eye Normal left eye left eye left eye Abnormal INSPECTIoN: WNL NE Lids, Lashes Lacrimal gland/duct Orbit (protrusion) Cranial Facial features Peripheral vision Visual Fields (6) Accommodation Alignment cover/uncover PENLIGHT EXAM: Iris Sclera Conjunctiva Pupil direct & consensual Corneal light check FUNDoScoPIc EXAM: Red Reflex Optic Disc Retinal AV Vessels Macula () () () () () () () () () () () () () () () () ( ( ( ( ( ) ) ) ) ) ( ( ( ( ( ) ) ) ) ) ( ( ( ( ) ) ) ) ( ( ( ( ) ) ) ) Norm (Age 3: 20/50, age 5: 20/40, >5: 20/30.) (Refer if 2 lines difference between eyes) _ . Stereogram: Normal Abnormal EXCEPTION A: - - - - - - - - - - - - - - P: Referral to Optometry or Ophthalmology