* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Full Product Information
Survey
Document related concepts
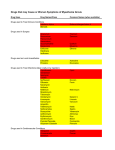
Transcript
LATANOPROST/TIMOLOL MALEATE XALACOM 1.0 TRADE NAME OF THE PRODUCT Xalacom 2.0 DESCRIPTION Timolol C13H24 N4O3 S 1/2 H20. 325.43. (1) 2-Propanol, 1-[(1,1-dimethylethyl)amino]-3([4-(4morpholinyl)-1,2,5thiadiazol-3-yl]oxy]-, hemihydrate, (S)-; (2) (S)-1-(tert Butylamino)-3-[(4-morpholino-1,2,5-=thiadiazol-3-yl)-2-propanol hemihydrate. CAS 91524-16-2, INN; BAN anti-adrenergic (β -receptor). Latanoprost C26H40O5. 432.59 (1) 5-Heptenoic acid, 7-[3,5-dihydroxy-2-(3-hydroxy-5phenylpentyl)cyclopentyl]-1-methylethyl ester, (iR-[1 α(Z),2β(R*), 3α,5α]; (2) Isopropyl (Z)-7-(IR,2R,3R,5S)-3,5-dihydroxy-2-(3R)-3-hydroxy-5phenylpentyl0[cyclopentyl]-5-heptenoate. CAS-130209-82-4. INN; BAN: Antiglaucoma agent. 3.0 FORMULATION Each mL contains: Latanoprost 50 mcg Timolol maleate equivalent to 5mg timolol 4.0 CLINICAL PARTICULARS 4.1 Therapeutic indications Reduction of intraocular pressure (IOP) in patients with open angle glaucoma or ocular hypertension who are insufficiently responsive to topical IOP lowering agents. 4.2 Dosage and method of administration Use in adults (including the elderly): One drop in the affected eye(s) once daily. The dosage of latanoprost-timolol maleate should not exceed once daily since it has been shown that more frequent administration of latanoprost decreases the intraocular pressure lowering effect. If one dose is missed treatment should continue with the next dose as planned. If more than one topical ophthalmic drug is being used, the drugs should be administered at least five minutes apart. Contact lenses should be removed before instillation of the eye drops and may be reinserted after fifteen minutes. (See section 4.4 Special Warnings and Special Precautions for Use – General). When using nasolacrimal occlusion or closing the eyelids for 2 minutes, the systemic absorption is reduced. This may result in a decrease in systemic side effects and an increase in local activity. Use in children: Safety and effectiveness in children have not been established. 4.3 Contraindications Latanoprost-timolol maleate (Xalacom) is contraindicated in patients with: • • Reactive airway disease including bronchial asthma, a history of bronchial asthma or severe chronic obstructive pulmonary disease. Sinus bradycardia, sick sinus syndrome,sino-atrial block, second or third degree atrioventricular block not controlled with pacemaker, overt cardiac failure or cardiogenic shock. • 4.4 Known hypersensitivity to latanoprost, timolol-maleate or any other component of this product, i.e., benzalkonium chloride, sodium chloride, sodium dihydrogen phosphate monohydrate, disodium phosphate anhydrous. Special warnings and precautions for use General: This product contains benzalkonium chloride, which may be absorbed by contact lenses. (See section 4.2 Dosage and Method of Administration) Latanoprost: Latanoprost may gradually increase the brown pigment of the iris. The eye color change is due to increased melanin content in the stromal melanocytes of the iris, rather than to an increase in the number of melanocytes. Typically, the brown pigmentation around the pupil spreads concentrically towards the periphery of the iris and the entire iris or parts of the iris become more brownish. The change in iris color is mild in the majority of cases and may not be detected clinically. The increase in iris pigmentation in one or both eyes has been documented predominantly in patients who have mixed-color irides that contain the color brown at baseline. Neither nevi nor freckles of the iris have been affected by treatment. No accumulation of pigment in the trabecular meshwork or elsewhere in the anterior chamber has been observed in clinical trials. In a clinical trial designed to assess iris pigmentation over five years, there was no evidence of adverse consequences due to increased pigmentation even when administration of latanoprost continued. These results are consistent with post-marketing clinical experience since 1996. In addition, IOP reduction was similar in patients regardless of the development of increased iris pigmentation. Therefore, treatment with latanoprost can be continued in patients who develop increased iris pigmentation. These patients should be examined regularly and, depending on the clinical situation, treatment may be stopped. Onset of increased iris pigmentation typically occurs within the first year of treatment, rarely during the second or third year, and has not been seen after the fourth year of treatment. The rate of progression of iris pigmentation decreases with time and is stable by five years. The effects of increased pigmentation beyond five years have not been evaluated. During clinical trials, the increase in brown iris pigment has not been shown to progress further upon discontinuation of treatment, but the resultant color change may be permanent. Eyelid skin darkening, which may be reversible, has been reported in association with the use of latanoprost. Latanoprost may gradually change eyelashes and vellus hair in the treated eye; these changes include increased length, thickness, pigmentation, and number of lashes or hairs, and misdirected growth of eyelashes. Eyelash changes are reversible upon discontinuation of treatment. The potential for heterochromia exists for patients receiving unilateral treatment. Macular edema, including cystoid macular edema, has been reported during treatment with latanoprost. These reports have mainly occurred in aphakic patients, in pseudophakic patients with torn posterior lens capsule, or in patients with known risk factors for macular edema. Caution is recommended when using latanoprost in these patients. There is no documented experience with latanoprost-timolol in inflammatory, neovascular, chronic angle closure glaucoma, in open angle glaucoma of pseudophakic patients and in pigmentary glaucoma. Therefore it is recommended that latanoprost-timolol should be used with caution in these conditions until more experience is obtained. Latanoprost should be used with caution in patients with a history of herpetic keratitis, and should be avoided in cases of active herpes simplex keratitis and in patients with a history of recurrent herpetic keratitis specifically associated with prostaglandin analogues. Timolol Maleate: The same adverse reactions found with systemic administration of betaadrenergic blocking agents may occur with their topical administration. Patients with a history of severe cardiac disease should be monitored closely for signs of cardiac failure. The following cardiac and respiratory reactions may occur after topical application of timolol maleate: • aggravation of Prinzmetal’s angina • aggravation of peripheral and central circulatory disorders • hypotension • cardiac failure resulting in death • severe respiratory reactions, including fatal bronchospasm in patients with asthma • bradycardia Due to its negative effect on conduction time, beta-blockers should only be given with caution to patients with first degree heart block. Patients with severe peripheral circulatory disturbance/disorders (i.e. severe forms of Raynaud’s disease or Raynaud’s syndrome) should be treated with caution. Timolol maleate should be used with caution, in patients with mild/moderate chronic obstructive pulmonary disease (COPD) and only if the potential benefit outweighs the potential risk A gradual withdrawal of beta-adrenergic blocking agents prior to major surgery should be considered. Beta-adrenergic blocking agents impair the ability of the heart to respond to beta-adrenergically mediated reflex stimuli, which may augment the risk of general anesthesia in surgical procedures. Protracted severe hypotension during anesthesia and difficulty restarting and maintaining the heartbeat have been reported. During surgery, the effects of beta-adrenergic blocking agents may be reversed by sufficient doses of adrenergic agonists. Beta-blocking ophthalmological preparations may block systemic betaagonist effects e.g. of adrenaline. The anaesthesiologist should be informed when the patient is receiving timolol. Beta-adrenergic blocking agents may increase the hypoglycemic effect of agents used to treat diabetes, and can mask the signs and symptoms of hypoglycemia. They should be used with caution in patients with spontaneous hypoglycemia or diabetes (especially those with labile diabetes), who are receiving insulin or oral hypoglycemic agents. Therapy with beta-adrenergic blocking agents may mask certain signs and symptoms of hyperthyroidism. Abrupt withdrawal of therapy may precipitate a worsening of this condition. When treated with beta-adrenergic blocking agents, patients with a history of atopy or severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge with such allergens. They may be unresponsive to the usual doses of epinephrine used to treat anaphylactic reactions. Timolol maleate has been reported to rarely increase muscle weakness in some patients with myasthenia gravis or myasthenic symptoms (e.g. diplopia, ptosis, generalized weakness). Choroidal detachment after filtration procedures has been reported with the administration of ocular hypotensive agents. Ophthalmic beta-blockers may induce dryness of eyes. Patients with corneal diseases should be treated with caution. 4.5 Interaction with other medicinal products and other forms of interaction Specific medicinal product interaction studies have not been performed with latanoprost-timolol maleate. The effect on intraocular pressure or the known effects of systemic betablockade may be potentiated when latanoprost-timolol maleate is given to patients already receiving an oral beta-adrenergic blocking agent, and the use of two or more topical beta-adrenergic blocking agents is not recommended. There have been reports of paradoxical elevations in IOP following the concomitant ophthalmic administration of two prostaglandin analogs. Therefore, the use of two or more prostaglandins, prostaglandin analogs, or prostaglandin derivatives is not recommended. Mydriasis has occasionally been reported when timolol maleate was given with epinephrine. The potential exists for additive effects resulting in systemic hypotension and/or marked bradycardia when timolol maleate is administered with: • calcium channel blockers • catecholamine-depleting drugs or beta-adrenergic blocking agents • antiarrythmics (including amiodarone) • digitalis glycosides • guanethidine Potentiated systemic beta blockade (e.g., decreased heart rate, depression) has been reported during combined treatment with CYP2D6 inhibitors (e.g. quinidine, fluoxetine, paroxetine) and timolol. Beta-adrenergic blocking agents may increase the hypoglycemic effect of agents used to treat diabetes. (See section 4.4 Special Warnings and Special Precautions for Use – Timolol Maleate). 4.6 Fertility, pregnancy and lactation Fertility: Latanoprost has not been found to have any effect on male or female fertility in animal studies. Reproduction and fertility studies of timolol maleate in rats demonstrated no adverse effect on male or female fertility at doses up to 21,000 times the systemic exposure following the maximum recommended human ophthalmic dose. (See section 5.3 Preclinical Safety Data – Impairment of Fertility - Latanoprost and Timolol Maleate) Pregnancy There are no adequate and well controlled studies in pregnant women. Latanoprost-timolol maleate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. (See section 5.3 Preclinical Safety Data – Latanoprost and Timolol Maleate). Lactation Latanoprost and its metabolites may pass into breast milk. Timolol maleate has been detected in human milk following oral and ocular drug administration. Because of the potential for serious adverse reactions in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. 4.7 Effects on ability to drive and use machines Instillation of eye drops may cause transient blurring of vision. Until this has resolved, patients should not drive or use machines. 4.8 Undesirable effects Latanoprost-Timolol Maleate: Clinical Trials: Adverse events observed in ≥1% of the patients treated with latanoprosttimolol maleate in three controlled, phase three clinical trials (6 month, 6 month, and 12 month, respectively) were: Ocular: Eye Disorders: Abnormal vision, blepharitis cataract, conjunctival disorder, conjunctivitis, corneal disorder, errors of refraction, eye hyperemia, eye irritation, eye pain, increased iris pigmentation, keratitis, photophobia, and vision field defect. Systemic: Infections and Infestations: Infection, sinusitis, and upper respiratory tract infection. Metabolism and Nutrition Disorders: Diabetes mellitus, hypercholesterolemia. Psychiatric Disorders: Depression. Nervous System Disorders: Headache Vascular Disorders: Hypertension. Skin and Subcutaneous Tissue Disorders: Hypertrichosis, rash, and skin disorder. Musculoskeletal and Connective Tissue Disorders: Arthritis Other significant adverse events that have been reported with the individual components of latanoprost-timolol maleate are listed below. Latanoprost: Clinical Trials: The following events were considered drug related: Eye Disorders: Eye irritation (burning, grittiness, itching, stinging and foreign body sensation), transient punctuate epithelial erosions, and eyelid edema Skin and Subcutaneous Tissue Disorders: Skin rash Post Marketing Surveillance: The following additional events have been reported: Nervous System Disorders: Dizziness Eye Disorders: Corneal edema and erosions, eyelash and vellus hair changes (increased length, thickness, pigmentation, and number), iritis/uveitis, macular edema, including cystoid macular edema, misdirected eyelashes sometimes resulting in eye irritation; vision blurred, photophobia, periorbital and lid changes resulting in deepening of the eyelid sulcus. (See section 4.4 Special Warnings and Special Precautions for Use – Latanoprost). Respiratory, Thoracic and Mediastinal Disorders: Asthma, asthma aggravation, acute asthma attacks, and dyspnea. Skin and Subcutaneous Tissue Disorders: Darkening of the palpebral skin of the eyelids and localized skin reaction on the eyelids. Musculoskeletal and Connective Tissue Disorders: Muscle /joint pain. General Disorders and Administration Site Conditions: Non-specific chest pain. Infections and Infestations: Not known: herpetic keratitis Timolol Maleate (Ocular Administration): Immune System Disorders: Signs and symptoms of systemic allergic reactions including anaphylaxis, angioedema, urticaria, pruritus and localized and generalized rash. Metabolism and Nutrition Disorders: Anorexia, masked symptoms of hypoglycemia in diabetic patients (See section 4.4 Special Warnings and Special Precautions for Use – Timolol Maleate). Psychiatric Disorders: Behavioral changes and psychic disturbances including, confusion, hallucinations, anxiety, disorientation, nervousness, and memory loss; decreased libido; insomnia; depression and nightmares. Nervous System Disorders: Cerebral ischemia, cerebral vascular accident, dizziness, increase in signs and symptoms of myasthemia gravis (See section 4.4 Special Warnings and Special Precautions for Use – Timolol Maleate), paresthesia, somnolence, headache and syncope. Eye Disorders; Cystoid macular edema; decreased corneal sensitivity; signs and symptoms of ocular irritation (e.g., burning, stinging, itching, tearing, redness), blepharitis, keratitis, vision blurred, dry eyes, corneal erosion, choroidal detachment following filtration surgery (See section 4.4 Special Warnings and Special Precautions for Use – Timolol Maleate); ptosis; and visual disturbances including refractive changes and diplopia. Ear and Labyrinth Disorders: Tinnitus Cardiac Disorders: Arrhythmia, bradycardia, atrioventricular block, congestive heart failure, cardiac arrest, cardiac failure, heart block, palpitation and worsening of angina pectoris (See section 4.4 Special Warnings and Special Precautions for Use – Timolol Maleate). Vascular Disorders: Claudication, cold hands and feet, hypotension, and Raynaud’s phenomenon. Respiratory, Thoracic and Mediastinal Disorders: Bronchospasm (predominatly in patients with pre-existing bronchospastic disease. (See section 4.4 Special Warnings and Special Precautions for Use – Timolol Maleate), cough, dyspnea, nasal congestion, pulmonary edema, and respiratory failure. Gastrointestinal Disorders: Diarrhea, dry mouth, dysgeusia, dyspepsia, nausea, vomiting, abdominal pain and retroperitoneal fibrosis. Skin and Subcutaneous Tissue Disorders: Alopecia, pseudopemphigoid, skin rash and psoriasiform rash or exacerbation of psoriasis. Musculoskeletal and Connective Tissue Disorders: Systemic lupus erythematosus and myalgia. Reproductive System and Breast Disorders: Decreased libido, impotence, sexual dysfunction and Peyronie’s disease. General Disorders and Administration Site Conditions: Asthenia/fatigue, chest pain, and edema. 4.9 Overdosage If overdosage with latanoprost-timolol occurs, treatment should be symptomatic. Information concerning overdose with the individual components is provided below: Latanoprost Apart from ocular irritation and conjunctival hyperemia, no other ocular adverse effects areknown if latanoprost is overdosed. If latanoprost is accidentally ingested the following information may be useful. One 2.5 mL bottle contains 125 micrograms latanoprost. More than 90% is extensively metabolized during the first pass through the liver. Intravenous infusion of 3 mcg/kg in healthy volunteers induced no symptoms but a dose of 5.5 – 10 mcg/kg caused nausea, abdominal pain, dizziness, fatigue, hot flushes and sweating. In patients with moderate bronchial asthma, bronchoconstriction was not induced by latanoprost when applied topically on the eys in a dose of seven times the clinical dose of latanoprost. (See section 5.3 Preclinical Safety Data – Latanoprost:Systemic/Ocular Effects) Timolol Maleate There have been reports of inadvertent overdosage with timolol-maleate ophthalmic solution resulting in systemic effects similar to those seen with systemic beta-adrenergic blocking agents such as dizziness, headache, shortness of breath, bradycardia, bronchospasm, and cardiac arrest. (See section 4.8 Undesirable Effects-Timolol Maleate (Ocular Administration) An in vitro hemodialysis study demonstrated that timolol was readily dialyzed from human plasma or whole blood. A study with renal failure patients demonstrated that timolol was not readily dialyzed. 5.0 PHARMACOLOGICAL PROPERTIES 5.1 Pharmacodynamic properties Mechanism of Action Product consists of two components: latanoprost and timolol maleate. These two components decrease elevated intraocular pressure (IOP) by different mechanisms of action and the combined effect results in additional IOP reduction compared to either compound administered alone. Latanoprost The active substance of latanoprost, a prostaglandin F2alpha analogue, is a selective prostanoid FP receptor agonist that reduces the IOP by increasing the outflow of aqueous humour, primarily through the uveoscleral route and also through the trabecular meshwork. Clinical trials have shown that latanoprost has no significant effect on the production of aqueous humour. Latanoprost has not been found to have any effect on the blood-aqueous barrier . Latanoprost has not induced fluorescein leakage in the posterior segment of pseudophalic human eyes during short term treatment. Latanoprost in clinical doses has not been found to have any significant pharmacological effects on the cardiovascular or respiratory system. Timolol Maleate Timolol maleate is a beta-1 and beta-2 (non-selective) adrenergic receptor blocking agent that does not have significant intrinsic sympathomimetic, direct myocardial depressant, or local anesthetic (membrane-stabilizing) activity. Beta-adrenergic receptor blockade reduces cardiac output in both healthy subjects and patients with heart disease. In patients with severe impairment of myocardial function, beta-adrenergic receptor blockade may inhibit the stimulatory effect of the sympathetic nervous system necessary to maintain adequate cardiac function. Beta-adrenergic receptor blockade in the bronchi and bronchioles results in increased airway resistance from unopposed parasympathetic activity. Such an effect in patients with asthma or other bronchospastic conditions is potentially dangerous (See section 4.3 Contraindications and section 4.4 Special Warnings and Special Precautions for Use – Timolol Maleate). Timolol maleate ophthalmic solution, when applied topically on the eye, has the action of reducing elevated as well as normal intraocular pressure, whether or not accompanied by glaucoma. Elevated intraocular pressure is a major risk factor in the pathogenesis of glaucomatous visual field loss. The higher the level of intraocular pressure, the greater the likelihood of glaucomatous visual field loss and optic nerve damage. The precise mechanism of the ocular hypotensive action of timolol maleate is not clearly established at this time. Tonography and fluorophotometry studies in man suggest that its predominant action may be related to reduced aqueous formation. However, in some studies a slight increase in outflow facility was also observed. Clinical Effects: In dose finding studies, latanoprost-timolol maleate produced significantly greater decreases in mean diurnal IOP compared to latanoprost and timolol maleate administered once daily as monotherapy. In two well controlled, double masked six-month clinical studies the IOP reducing effect of latanoprost-timolol maleate was compared with latanoprost and timolol maleate monotherapy in patients with an IOP of at least 25 mm Hg or greater. Following a 2 to 4 week run-in with timolol maleate (mean decrease in IOP from enrollment of 5 mm Hg), additional decreases in mean diurnal IOP of 3.1, 2.0 and 0.6 mm Hg were observed after 6 months of treatment with latanoprost-timolol maleate and latanoprost and timolol maleate (twice daily), respectively. The IOP lowering effect of latanoprost-timolol maleate was maintained in a 6 month open label extension of these studies. Onset of action of latanoprost-timolol maleate is within one hour and maximal effect occurs within six to eight hours. Adequate IOP reducing effect has been shown to be present up to 24 hours post dosage after multiple treatments. 5.2 Pharmacokinetic properties Latanoprost-Timolol Maleate: No pharmacokinetic interactions between latanoprost and timolol maleate were observed, although there was an approximate two-fold increased concentration of the acid of latanoprost in aqueous humour 1 to 4 hours after administration of latanoprost-timolol maleate compared to monotherapy. Latanoprost: Absorption: Latanoprost is absorbed through the cornea where the isopropyl ester prodrug is hydrolyzed to the acid form to become biologically active. Studies in man indicate that the peak concentration in the aqueous humor is reached about two hours after topical administration. Distribution: The distribution volume in humans is 0.16 ± 0.02 L/kg. The acid of latanoprost can be measured in aqueous humor during the first four hours, and in plasma only during the first hour after local administration. Metabolism: Latanoprost, an isopropyl ester prodrug, is hydrolyzed by esterases in the cornea to the biologically active acid. The active acid of latanoprost reaching the systemic circulation is primarily metabolized by the liver to the 1,2-dinor and 1,2,3,4-tetranor metabolites via fatty acid β-oxidation. Excretion: The elimination of the acid of latanoprost from human plasma is rapid (t1/2 =17 min) after both intravenous and topical administration. Systemic clearance is approximately 7 mL/min/kg. Following hepatic β-oxidation, the metabolites are mainly eliminated via the kidneys. Approximately 88% and 98% of the administered dose is recovered in the urine after topical and intravenous dosing, respectively. Timolol Maleate: The maximum concentration of timolol maleate in the aqueous humor is reached about one hour after topical administration of eye drops. Part of the dose is absorbed systemically and a maximum plasma concentration of 1 ng/ml is reached 10 to 20 minutes after topical administration of one eye drop to each eye once daily (300 micrograms/day). The half-life of timolol maleate in plasma is about six hours. Timolol maleate is extensively metabolized in the liver. The metabolites are excreted in the urine together with some unchanged timolol maleate. 5.3 Preclinical safety data The ocular and systemic safety profile of the individual components is well established. No adverse ocular or systemic effects were seen in rabbits treated topically with the fixed combination or with concomitantly administered latanoprost and timolol ophthalmic solutions. Safety pharmacology, genotoxicity and carcinogenicity studies with each of the components revealed no special hazards for humans. Latanoprost did not affect corneal wound healing in the rabbit eye, whereas timolol inhibited the process in the rabbit and the monkey eye when administered more frequently than once a day. Latanoprost: Systemic/Ocular Effects: The ocular as well as systemic toxicity of latanoprost has been investigated in several animal species. Generally, latanoprost is well tolerated with a safety margin between clinical ocular dose and systemic toxicity of at least 1000 times. High doses of latanoprost, approximately 100 times the clinical dose/kg body weight, administered intravenously to unanesthetized monkeys have been shown to increase the respiration rate probably reflecting bronchoconstriction of short duration. In monkeys, latanoprost has been infused intravenously in doses of up to 500 mcg/kg without major effects on the cardiovascular system. In animal studies, latanoprost has not been found to have sensitizing properties. In the eye, no toxic effects have been detected with doses of up to 100 micrograms/eye/day in rabbits or monkeys (clinical dose is approximately 1.5 micrograms/eye/day). Latanoprost has no or negligible effects on the intraocular blood circulation when used at the clinical dose and studied in monkeys. In chronic ocular toxicity studies, administration of latanoprost 6 micrograms/eye/day has also been shown to induce increased palpebral fissure. This effect is reversible and occurs at doses above the clinical dose level. The effect has not been seen in humans. Carcinogenesis: Carcinogenicity studies in mice and rats were negative. Mutagenesis: Latanoprost was found negative in reverse mutation tests in bacteria, gene mutation in mouse lymphoma and mouse micronucleus test. Chromosome aberrations were observed in vitro with human lymphocytes. Similar effects were observed with prostaglandin F2α, a naturally occurring prostaglandin, and indicates that this is a class effect Additional mutagenicity studies on in vitro/in vivo unscheduled DNA synthesis in rats were negative and indicate that latanoprost does not have mutagenic potency. Impairment of Fertility: Latanoprost has not been found to have any effect on male or female fertility in animal studies. In the embryotoxicity study in rats, no embryotoxicity was observed at intravenous doses (5, 50 and 250 micrograms/kg/day) of latanoprost. However, latanoprost induced embryolethal effects in rabbits at doses of 5 micrograms/kg/day and above. Latanoprost has been shown to cause embryofetal toxicity in rabbits characterized by increased incidences of late resorption and abortion and reduced fetal weight when given in intravenous doses approximately 100 times the human dose. Teratogenesis: No teratogenic potential has been detected. Timolol Maleate: Carcinogenesis: In a two-year study of timolol maleate administered orally to rats, there was a statistically significant increase in the incidence of adrenal pheochromocytomas in male rats administered 300 mg/kg/day (approximately 42,000 times the systemic exposure following the maximum recommended human ophthalmic dose). Similar differences were not observed in rats administered oral doses equivalent to approximately 14,000 times the maximum recommended human ophthalmic dose. In a lifetime oral study in mice, there were statistically significant increases in the incidence of benign and malignant pulmonary tumors, benign uterine polyps and mammary adenocarcinomas in female mice at 500 mg/kg/day, (approximately 71,000 times the systemic exposure following the maximum recommended human ophthalmic dose), but not at 5 or 50 mg/kg/day (approximately 700 or 7,000, respectively, times the systemic exposure following the maximum recommended human ophthalmic dose). In a subsequent study in female mice, in which postmortem examinations were limited to the uterus and the lungs, a statistically significant increase in the incidence of pulmonary tumors was again observed at 500 mg/kg/day. The increased occurrence of mammary adenocarcinomas was associated with elevations in serum prolactin which occurred in female mice administered oral timolol maleate at 500 mg/kg/day, but not at doses of 5 or 50 mg/kg/day. An increased incidence of mammary adenocarcinomas in rodents has been associated with administration of several other therapeutic agents that elevate serum prolactin, but no correlation between serum prolactin levels and mammary tumors has been established in humans. Mutagenesis: Timolol maleate was devoid of mutagenic potential when tested in vivo (mouse) in the micronucleus test and cytogenetic assay (doses up to 800 mg/kg) and in vitro in a neoplastic cell transformation assay (up to 100 mcg/mL). In Ames tests the highest concentrations of timolol maleate employed, 5,000 or 10,000 mcg/plate, were associated with statistically significant elevations of revertants observed with tester strain TA100 (in seven replicate assays), but not in the remaining three strains. In the assays with tester strain TA100, no consistent dose response relationship was observed, and the ratio of test to control revertants did not reach 2. A ratio of 2 is usually considered the criterion for a positive Ames test. Impairment of Fertility: Reproduction and fertility studies in rats demonstrated no adverse effect on male or female fertility at doses up to 21,000 times the systemic exposure following the maximum recommended human ophthalmic dose. Teratogenesis: Teratogenicity studies with timolol maleate in mice, rats, and rabbits at oral doses up to 50 mg/kg/day (7,000 times the systemic exposure following the maximum recommended human ophthalmic dose) demonstrated no evidence of fetal malformations. Although delayed fetal ossification was observed at this dose in rats, there were no adverse effects on postnatal development of offspring. Doses of 1000 mg/kg/day (142,000 times the systemic exposure following the maximum recommended human ophthalmic dose) were maternotoxic in mice and resulted in an increased number of fetal resorptions. Increased fetal resorptions were also seen in rabbits at doses of 14,000 times the systemic exposure following the maximum recommended human ophthalmic dose, in this case without apparent maternotoxicity. 6.0 PHARMACEUTICAL PARTICULARS 6.1 Shelf life Please see outer package for the expiry date of the product. 6.2 Storage Store unopened bottle(s) under refrigeration at 2° – 8°C (36°F to 46°F). After first opening the container,store at or below 25° (77°F) and use within four weeks. . Protect from light. 6.3 Availability Xalacom 50 mcg/5 mg per 5 mL Ophthalmic Solution: Clear and colorless solution free of visible particulates. Each bottle contains 2.5 mL eye drop solution corresponding to approximately 80 drops. CAUTION: Foods, Drugs, Devices and Cosmetics Act prohibits dispensing without prescription. Manufactured by: Pharmacia NV/SA, Puurs, Belgium Imported by: Pfizer, Inc. 23rd Floor, Ayala Life-FGU Center 6811 Ayala Avenue Makati City, Philippines Reference No.: CDS ver 3.0 Reference Date: November 2011 Revision No.: 2 Revision Date: 21 November 2011 REFERENCES: 1. Akingbehin T, Raj PS. Ophthalmic topical beta-adrenergic blocking agents: review of ocular systemic adverse effects. J. Toxicol. Cut. & Ocular Toxicol. 1990; 9:131-147. 2. Alm A, Widnergård I, Kjellgren D, et al. Latanoprost administered once daily caused a maintained reduction of intraocular pressure in glaucoma patients treated concomitantly with timolol. Br J Ophthalmol. 1995; 79:12-16. 3. Alm A, Anheller J-E, Kaponen T. Intraocular pressure lowering effect and side effects of PhXA41. A four-week dose titration study. Pharmacia report L411 G018 (CTN 91PG03). 29 November 1991. Published as: Alm A, Villumsen J, Törnquist P, et al. Intraocular pressure reducing effect of PhXA41 in ocular hypertensive patients - a one month study. Ophthalmology. 1993; 100:1312-17. 4. Almegard B, Asenblad N-G, Almbrand B. A 6-month, randomized, doublemasked comparison of fixed combination of latanoprost and timolol with the individual components, continuing into a 6-month, open-label safety study of fixed combination in patients with glaucoma or ocular hypertension. A multicenter study in the United States. Pharmacia & Upjohn study report c0013532 (96TIPG005), 5 November 1999. 5. Anheller J-E, Kaponen T, Stjernschantz J. A six-month, randomized, doublemasked comparison of PhXA41 to timolol in patients with open-angle glaucoma or ocular hypertension. A multi-centre study in the United Kingdom. Pharmacia & Upjohn AB report 9400243 (CTN 9200PG005), 3 March 1995. Published as: Watson P, Stjernschantz J. The Latanoprost Study Group. A six- month, randomized, double-masked study comparing latanoprost with timolol in openangle glaucoma and ocular hypertension. Ophthalmology. 1996; 103:126-137. 6. Backman C, Asenblad N-G, Almbrand B. A 6-month, randomized, doublemasked comparison of fixed combination of latanoprost and timolol with the individual components, continuing into a 6- month, open-label safety study of fixed combination in patients with glaucoma or ocular hypertension. A multicenter study in Germany. Pharmacia & Upjohn Study Report c0013595 (96TIPG004), 5 November 1999. 7. Backman C, Eriksson G, Hedman K, Alm A. Comparison of fixed-ratio combinations of latanoprost (PhXA41) and timolol: a randomized, 3-parallel group, double-masked, multi-center study in patients with open angle glaucoma or ocular hypertension. Pharmacia AB report 9400634 (CTN 93TIPG001), 29 August 1996. 8. Clinical Overview: Latanoprost CDS update 7 July 2011, 11 Aug 2011. 9. Clinical Overview: Xalatan latanoprost CDS CO supporting HKeratitis update to CDS October 2010. 10. Clinical Overview: Xalacom CDS Revision for Use with Beta Blockers. Sep 27, 2011 11. Data on file: Pharmacia & Upjohn report c0003751, c0008232 (CTN9400PG034), CTN 9600PG053, L411 G016 (CTN 91PG04), 9200027, 9200137, 9300279, 9300281, 9300280, 9300280, 9500332, 9700314, 9700335, 9600070, 9700285, 9700331, 9800066, 9810452 12. Diggory P, Cassel-Brown, A, Vail A, Abbey LM, Hillman JS. Avoiding unsuspected respiratory side-effects of topical timolol with cardioselective or sympathomimetic agents. Lancet. 1995; 345:1604-1606. 13. Eckman I, Lindquist H, Pettersson H. Safety and efficacy evaluation of up to 2 years treatment with latanoprost in patients with open-angle glaucoma or ocular hypertension in Scandinavia. A 6-month randomized, double-masked, multicentre study (CTN 9200PG006) followed by an 18-month open-label period (CTN 9200PG009). Pharmacia & Upjohn AB report 9500333, 23 April 1997. Accepted for publication: Alm A, Widengård I. Latanoprost: Experience of 2-year treatment in Scandinavia. Acta Ophthalmol Scand. 14. Eckman I, Lindquist H, Pettersson H. Safety and efficacy evaluation of up to oneyear treatment with latanoprost of patients with primary open-angle glaucoma or ocular hypertension. A 6-month randomized, double-masked, multi-centre study (CTN 9200PG004) followed by a 6-month open-label period (CTN 9200PG010) in the USA. Pharmacia and Upjohn AB report 9500334. 21 October 1996. Published as: Camras CB, Was MB, Ritch R, et al. Latanoprost treatment for glaucoma: Effects after 1 year and of switching from timolol. Am J Ophthalmol. 1998; 26:390-9. 15. Herndon L, Asrani S, Williams G, Challa P, Lee P. Paradoxical Intraocular Pressure Elevation after Combined Therapy with Latanoprost and Bimatoprost. Am. J Ophthalmol. In press. 16. Hughes J, McDermott J, Schoenfelder J. A long-term open study of safety of latanoprost as adjunctive therapy in glaucoma patients with uncontrolled intraocular pressure. A multi-center study in Sweden, Great Briatin, the Netherlands, Australia, and Belgium. Pharmacia report 9400PG034. 21 May 2002. 17. Integrated Summary of Safety (ISS), NDA 21-219 18. Johansson M, Alm A, Kaponen T, Stjernschantz, J. A 6-month, randomized, double-masked comparison of latanoprost (PhXA41) with timolol in patients with open-angle glaucoma or ocular hypertension. A multi-centre study in Scandinavia. Pharmacia & Upjohn AB report 9400194 (CTN 9200PG006), 3 March 1995. Published as: Alm A, Stjernschantz J. The Scandinavian Latanoprost Study Group. Effects on intraocular pressure and side effects of 0.005% latanoprost applied once daily, evening or morning. A comparison with timolol. Ophthalmology. 1995; 102:1743-1752. 19. Johnstone MA, Hypertrichosis and increased pigmentation of eyelashes and adjacent hair in the region of the ipsilateral eyelids of patients treated with unilateral topical latanoprost. Am J Ophthalm 1997; 124: 544-547. 20. Kabi Pharmacia report L411 S034, L411 S035, L411 S036, L411 S037. 21. Kook M, Lee, K. Increased Eyelid Pigmentation Associated With Use of Latanoprost. Am. J Ophthalmol, 2000; 129(6):804-806. 22. Larsson, LI, Johanhsson, M, Asenblad, N-G, and Almbrand, B. Diurnal intraocular pressure after single-dose administration of the fixed combination latanoprost 0.005% and timolol 0.5% in ocular hypertensive patients. A randomized, double-masked placebo controlled single-center study. Pharmacia & Upjohn report c0010132 (CTN 97TIPG007). 9 December 1998. 23. Larsson LI, Johanhsson M, Asenblad N-G, and Almbrand B. Diurnal intraocular pressure after repeated administration of the fixed combination latanoprost 0.005% and timolol 0.5% in ocular hypertensives. A placebo controlled, singlecenter, cross-over study. Pharmacia & Upjohn report 0010372 (CTN 97TIPG008), 9 December 1998. 24. Lederer C and Harold R. Drop size of commercial glaucoma medications. Am J Ophthalmol. 1986; 101:691-694. 25. Lemp MA, Wolfley DE. The lacrimal apparatus. In: Hart WM, ed. Physiology of the Eye. St. Louis: Mosby; 1992:18-28. 26. Linkewich JA, Herling IM. Bradycardia and congestive heart failure associated with ocular timolol maleate. Am J Hosp Pharm. 1981 May; 38:699-700. 27. Martindale. The Extra Pharmacopoeia. Thirty-first edition, London Royal Pharmaceutical Society; 1996:830-831, 954. 28. Mauger TF, Craig EL, eds. Havener’s Ocular Pharmacology. St. Louis: Mosby; 1994:27-32. 29. Munroe WP, Rindone JP, Kershner RM. Systemic side effects associated with the ophthalmic administration of timolol. Drug. Intell Clin Pharm. 1985; 19:85-89. 30. Nagasubramian S, Sheth GP, Hitchings RA, Stjernschantz J. Intraocular pressure reducing effect of PhXA41 in ocular hypertension. A comparison of dose regimens. Ophthalmology. 1993; 100:1305-1311. 31. Periodic Safety Update Report for Xalatan, Pharmacia & Upjohn Corporate Pharmacovigilance, CPV, 6 Dec 1997- 5 Jun 1999. 32. Parkhede U, Kaponen T, Stjernschantz J. A 6-month, randomized, doublemasked comparison of latanoprost (PhXA41) with timolol in patients with open angle-glaucoma or ocular hypertension. A multi-center study in the United States. Pharmacia & Upjohn AB report 9400369 (CTN 9200PG004), 23 March 1995. Published as: Camras CB. The United States Latanoprost Study Group. Comparison of latanoprost and timolol in patients with ocular hypertension and glaucoma. A six-month, masked, multi-center trial in the United States. Ophthalmology. 1996; 103:138-147. 33. Reference to medical practice. 34. Report by Pharmacia & Upjohn Global Drug Surveillance: Supportive Document for the Revision of the Core Data Sheet (CDS) for XALATAN Eye Drops/Latanoprost Eye Drops, 21 April 2000 (Amended 7 July 2000). 35. Rulo AH, Greve EL, and Hoyng PF. Additive effect of latanoprost, a prostaglandin F2α analogue, and timolol in patients with elevated intraocular pressure. Br J Ophthalmol. 1994; 78; 899-902. 36. Soll DB. Evaluation of timolol in chronic open-angle glaucoma. Once a day vs. twice a day. Arch Ophthalmol. 1980; 98:2178-2181. 37. Timoptic® 0.25% and 0.5% (timolol maleate ophthalmic solution) United States Package Insert. Issued September 2002. Merck & Co., Inc. Whitehouse Station, NJ 08889, USA. 38. Wand M, Ritch R, Isbey, Jr E, Zimmerman T. Latanoprost and Periocular Skin Color Changes. Arch Ophthalmol. 2001; 119:614-615. 39. Worldwide Labeling safety report: 06Dec04. 40. Xalatan, Safety Update 4 Jul 1997, 20 Feb 1997, 6 Jun 1997-5 Dec 1997. 41. Xu K-P, Tsubota K. Correlation of tar clearance rate and fluorophotometric assessment of tear turnover. Br. J. Ophthalmol. 1995;79:1042-1045. 42. Yalon M, Urinowsky E, Rothkoff L, Treister G, Blumenthal M. Frequency of timolol administration. Am J Ophthalmol. 1981; 92:526-529 43. Zimmerman TJ, Kaufman HE. Timolol dose response and duration of action. Arch Ophthalmol. 1977; 95:605-607.