* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cataract
Mitochondrial optic neuropathies wikipedia , lookup
Keratoconus wikipedia , lookup
Visual impairment wikipedia , lookup
Vision therapy wikipedia , lookup
Diabetic retinopathy wikipedia , lookup
Contact lens wikipedia , lookup
Corrective lens wikipedia , lookup
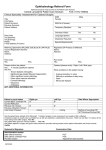
2 Cataract Clinical Definition Punctate (Blue-dot) cataract: A cataract is a clouding of the lens in the eye that affects vision • A hereditary opacity of the eye’s lens. Bright blue dot shaped opacities are irregularly scattered throughout the lens. • The bluish colour is due to the effects of dispersion of light. The visual acuity is not affected. Classification of cataract - - Congenital cataract (or) developmental cataract Acquired cataract Congenital (or) Development cataract Cataract that presents at birth or develops soon after the birth. Causes of Congenital cataract 1. Chromosomal abnormalities - a missing, extra or irregular portion of chromosomal DNA 2. Maternal malnutrition (vitamin –D deficiency) 3. Foetal hypoxia - fetus is deprived of adequate supply of oxygen 4. Drug intake during the pregnancy eg. Corticosteroids Anterior polar cataract - Morphological Types 1. 2. a. b. 3. 4. 5. 6. 7. 8. Blue-dot Cataract Punctate (blue-dot) cataract Anterior polar cataract Pyramidal Reduplicated Posterior polar cataract (Embryonic) nuclear cataract Coronary cataract Coralliform cataract Zonular (lamellar) cataract Total cataract - Soft, Membranous - A hereditary disorder occurring in children, and characterized by lesions with small white milky plaques in the front of the lens. Cloudy vision and near sightedness (myopia) are common. These opacities are stationary and rarely interfere with vision. Posterior polar cataract - This is due to residue of the attachment of hyaloid artery (A branch of the ophthalmic It is contained within the optic stalk of the eye and extends from the optic Coralliform cataract - congenital cataract with round or elongated processes radiating from the center of the lens A R A V I N D E Y E C A R E S Y S T E M 3 Posterior Polar Cataract disc through the vitreous humor to the lens on the posterior lens capsule) on the posterior lens capsule. This is usually dot – like mittendorf’s dot - (small, circular opacity on the posterior lens capsule) and insignificant. Coronary cataract - - A common visual disorder occurring in adults, that usually does not impair vision. Zones of small opacities may occur, varying in color from gray to brown, yellow, red or blue. The opacities are arranged radially in the outer layers of the lens, leaving the center of the eye clear. It does not interfere with vision. Zonular (lamellar) cataract - - It is probably the commonest type of development cataract presenting with visual impairment. It may be inherited through dominant genes, or caused by malnutrition during pregnancy or early infancy - hypovitaminosis – D (deficiency of Lamellar Cataract vitamin D ), hypocalcaemia (presence of low serum calcium levels in the blood ) Rubella Cataract - - - Rubella infection during pregnancy may cause wide-spread ocular and systemic defects. The cataract is originally nuclear and progresses to become total. It is associated with microphthalmos, nystagmus, strabismus, glaucoma, iris hypoplasia (prevents an iris from developing properly) and pigmentary retinopathy (a disorder of the retina characterized by deposits of pigment and increasing loss of vision) Acquired cataract is classified as follows 1. Senile 2. Traumatic - Mechanical - Irradiation - Electric shock 3. Complicated (due to some other ocular disease) Chlorpromazine - used as a tranquillizer, and sedative; Busulfan - used to treat chronic leukemia - abnormal blood cells are produced in the bone marrow. Compassion Apr - June, 2016 4 - - - - - Anterior uveitis High myopia Retinal detachment Retinal pigmentosa Glauokomflecken (gray-white epithelial and anterior cortical lens opacities) 4. Secondary (due to some systemic disease) - Diabetes mellitus - Hypocalcemia 5. Toxic (due to drugs) - Corticosteroids - Chlorpromazine - Miotics (long – acting) - Busulfanb - Amiodarone (used to help keep the heart beating normally in people with life-threatening heart rhythm disorders) - Gold 6. Syndromes associated with cataract - Down’s - (arising from a chromosome defect, causing intellectual impairment and physical abnormalities) - Lowe’s - - - Treacher Collins (a condition that affects the development of bones and other tissues of the face) Wilsons’s disease (too much copper to accumulate in the liver, brain and other vital organs) Fabry’s disease (buildup of a particular type of fat) Senile cataract The aging lens tends to become opaque after the age of 50 years and by the age of 70 over 90% of the population show some evidence of cataract. Senile cataract is divided into two types 1. Cortical or soft cataract (75 – 80%) - begins at the outer portion of the lens, then slowly moves inward. 2. Nuclear or hard cataract (20 – 25%)- forms deep in the central zone (nucleus) of the lens Stages of cataract 1. Stage of lamellar separation (demarcation of cortical fibres owing to their separation by fluid). Difference between cortical & nuclear cataract Cortical Cataract Nuclear Cataract 1. Usually starts at late 50s Tends to occur earlier than cortical 2. Starts with ocular diplopia / polyopia (two or more images) or coloured halos No such symptoms 3. Gives rise to index hypermetropia Gives rise to index myopia 4. Appears greyish and changes to milky Appears yellow, brown or black with white with the maturity of the cataract progression of cataract 5. More chance of lens induced secondary glaucoma A R A V I N D E Y E C A R E S Y S T E M Little chance of lens – induced secondary glaucoma 5 Difference between immature & mature cataract Immature Cataract Mature Cataract A. Symptoms 1. Partial loss of vision Total loss of vision 2. Diplopia / Polyopia White opacity 3. Rainbow halos noticed by the patients or relatives B. Signs 1. Visual acuity Vision reduced to varying degree Vision reduced to hand movement or PL 2. Colour of the lens Grey / greyish white White / pearly white 3. Iris shadow Present Absent 4. Purkinje’s image 3rd image is seen, 4th image may be distorted Only 3rd image is seen, 4th image absent 5. Fundal glow Present Absent 6. Retinoscopy Possible Not possible 7. Spectacles May improve vision Does not improve vision 2. Stage of incipient cataract (the lens of the eye is only slightly opaque, with a clear cortex). 3. Immature stage 4. Mature stage 5. Hypermature stage (the lens proteins have become liquid) Investigations prior to surgery 1. A. History B. Local Investigations - Vision - Perception of light (PL) - Projection of rays (PR) C. Action of pupil D. Slit lamp examination E. Intraocular pressure F. Patency of the lacrimal passage G. Funduscopy 2. Conjunctival swab for culture and sensitivity tests. 3. Calculation of IOL power. 4. Macular function tests 5. Systemic Investigations Surgical techniques in senile cataract: 1. Extra – Capsular Cataract Extraction (ECCE) 2. Intra – Capsular Cataract Extraction (ICCE) 3. Phaco – Emulsification 4. Intraocular lens implantation with any of the first three 5. Glaucoma surgery with any of the first three with or without IOL implantation. 6. Keratoplasty with any of the first three with or without IOL implantation. 7. Keratoplasty with ECCE with IOL implantation termed “Triple Procedure”. Stage of incipient cataract - the lens of the eye is only slightly opaque, with a clear cortex; Hypermature stage - the lens proteins have become liquid Compassion Apr - June, 2016