* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
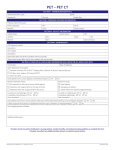
Download Quantification in fluorine-18-fluorodeoxyglucose dedicated breast
Survey
Document related concepts
Transcript
Quantification in fluorine-18-fluorodeoxyglucose dedicated breast
PET/CT
By
Spencer Lawson Bowen
B.S. (University of Washington, Seattle, WA) 2003
Dissertation
Submitted in partial satisfaction of the requirements for the degree of
Doctor of Philosophy
in
Biomedical Engineering
in the
Office of Graduate Studies
of the
University of California
Davis
Approved:
Ramsey D. Badawi, Chair
John M. Boone
Simon R. Cherry
Committee in Charge
2010
-i-
UMI Number: 3427421
All rights reserved
INFORMATION TO ALL USERS
The quality of this reproduction is dependent upon the quality of the copy submitted.
In the unlikely event that the author did not send a complete manuscript
and there are missing pages, these will be noted. Also, if material had to be removed,
a note will indicate the deletion.
UMI 3427421
Copyright 2010 by ProQuest LLC.
All rights reserved. This edition of the work is protected against
unauthorized copying under Title 17, United States Code.
ProQuest LLC
789 East Eisenhower Parkway
P.O. Box 1346
Ann Arbor, MI 48106-1346
Copyright
© 2010 by
Spencer Lawson Bowen
All rights reserved.
Contents
List of Figures . . . .
List of Tables . . . .
Abstract . . . . . . .
List of Abbreviations
Acknowledgments . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
. v
. xi
. xii
. xiv
. xvii
1 Background and Significance
1.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1.2 Theory of Positron Emission Tomography . . . . . . . . . . . . . .
1.3 Theory of X-Ray Computed Tomography . . . . . . . . . . . . . . .
1.4 Theory of Combined PET/CT . . . . . . . . . . . . . . . . . . . . .
1.5 Factors Influencing Image Quantification . . . . . . . . . . . . . . .
1.5.1 Scatter and Attenuation . . . . . . . . . . . . . . . . . . . .
1.5.2 Randoms . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1.5.3 Dead-Time . . . . . . . . . . . . . . . . . . . . . . . . . . .
1.5.4 Subject Motion . . . . . . . . . . . . . . . . . . . . . . . . .
1.6 Methods of Estimating Quantitative Performance for PET Scanners
1.6.1 Estimation of Image SNR as a Function of Count Rates
Using Noise Equivalent Counts Rates . . . . . . . . . . . . .
1.7 Clinical Motivation . . . . . . . . . . . . . . . . . . . . . . . . . . .
1.8 WB PET and PET/CT in the Management of Breast Cancer . . .
1.8.1 Clinical Applications . . . . . . . . . . . . . . . . . . . . . .
1.8.2 Limitations . . . . . . . . . . . . . . . . . . . . . . . . . . .
1.9 Dedicated Breast Positron Emission Imaging . . . . . . . . . . . . .
1.9.1 Positron Emission Mammography . . . . . . . . . . . . . . .
1.9.1.1 Hardware, Acquisition, and Reconstruction . . . .
1.9.1.2 Clinical Trial Results . . . . . . . . . . . . . . . . .
1.9.2 Breast Positron Emission Tomography . . . . . . . . . . . .
1.9.2.1 Hardware, Acquisition, and Reconstruction . . . .
1.10 Current Project . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1.10.1 Aim . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1.10.2 Outline of Dissertation . . . . . . . . . . . . . . . . . . . . .
1
1
2
9
13
14
14
15
16
17
18
2 Dedicated Breast PET/CT Instrumentation
2.1 Introduction . . . . . . . . . . . . . . . . . . .
2.2 Combined System Overview . . . . . . . . . .
2.3 CT System . . . . . . . . . . . . . . . . . . .
2.3.1 Hardware . . . . . . . . . . . . . . . .
2.3.2 Acquisition and Reconstruction . . . .
2.4 PET System . . . . . . . . . . . . . . . . . . .
2.4.1 Hardware . . . . . . . . . . . . . . . .
35
35
36
37
37
37
38
38
-ii-
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
18
19
20
20
22
24
25
25
28
31
31
32
32
32
2.5
2.4.2 Software . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
2.4.3 Acquisition and Reconstruction . . . . . . . . . . . . . . . .
Patient Bed and Positioning Aids . . . . . . . . . . . . . . . . . . .
41
45
47
3 Basic Performance Measurements
48
3.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 48
3.2 Materials and methods . . . . . . . . . . . . . . . . . . . . . . . . . 49
3.2.1 Spatial Resolution for MAP Reconstruction . . . . . . . . . 49
3.2.2 Noise Equivalent Count Rates for a Cylinder Phantom . . . 50
3.2.3 Noise Equivalent Count Rates for an Anthropomorphic Phantom . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 53
3.2.4 Coincidence Photon Detection Sensitivity . . . . . . . . . . . 55
3.2.5 Registration Accuracy . . . . . . . . . . . . . . . . . . . . . 56
3.2.6 Influence of PET on CT . . . . . . . . . . . . . . . . . . . . 59
3.3 Results . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 60
3.3.1 Spatial Resolution for MAP Reconstruction . . . . . . . . . 60
3.3.2 Noise Equivalent Count Rates for a Cylinder Phantom . . . 62
3.3.3 Noise Equivalent Count Rates for an Anthropomorphic Phantom . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 63
3.3.4 Coincidence Photon Detection Sensitivity . . . . . . . . . . . 65
3.3.5 Registration Accuracy . . . . . . . . . . . . . . . . . . . . . 66
3.3.6 Influence of PET on CT . . . . . . . . . . . . . . . . . . . . 67
4 Performance During Patient Imaging
4.1 Introduction . . . . . . . . . . . . . .
4.2 Materials and Methods . . . . . . . .
4.2.1 Patient Trial . . . . . . . . . .
4.2.2 Count Rates Estimations from
4.3 Results . . . . . . . . . . . . . . . . .
4.3.1 Patient Trial . . . . . . . . . .
4.3.2 NECR from Patient Scans . .
4.4 Discussion and Conclusions . . . . .
. . . . . . . .
. . . . . . . .
. . . . . . . .
Patient Scans
. . . . . . . .
. . . . . . . .
. . . . . . . .
. . . . . . . .
.
.
.
.
.
.
.
.
5 Implementation and Validation of Data Corrections
5.1 Introduction . . . . . . . . . . . . . . . . . . . . . . .
5.2 Materials and methods . . . . . . . . . . . . . . . . .
5.2.1 Correction methods. . . . . . . . . . . . . . .
5.2.1.1 Overview . . . . . . . . . . . . . . .
5.2.1.2 Normalization. . . . . . . . . . . . .
5.2.1.3 Dead-time. . . . . . . . . . . . . . .
5.2.1.4 Randoms. . . . . . . . . . . . . . . .
5.2.1.5 Attenuation. . . . . . . . . . . . . .
5.2.1.6 Scatter. . . . . . . . . . . . . . . . .
5.2.2 Validation experiments . . . . . . . . . . . . .
-iii-
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
69
69
70
70
72
74
74
78
79
.
.
.
.
.
.
.
.
.
.
84
84
85
85
85
86
87
89
89
90
92
5.3
5.4
5.2.2.1 General acquisition and data processing.
5.2.2.2 Dead-time and randoms. . . . . . . . . .
5.2.2.3 Attenuation validation. . . . . . . . . . .
5.2.2.4 Scatter. . . . . . . . . . . . . . . . . . .
5.2.2.5 Image uniformity. . . . . . . . . . . . . .
Results . . . . . . . . . . . . . . . . . . . . . . . . . . . .
5.3.1 Dead-time and randoms. . . . . . . . . . . . . . .
5.3.2 Attenuation validation. . . . . . . . . . . . . . . .
5.3.3 Scatter. . . . . . . . . . . . . . . . . . . . . . . .
5.3.4 Image uniformity. . . . . . . . . . . . . . . . . . .
Discussion . . . . . . . . . . . . . . . . . . . . . . . . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
92
93
94
95
96
97
97
100
102
105
107
6 Monte Carlo Simulation Design Study of bPET System Geometries
112
6.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 112
6.2 Materials and methods . . . . . . . . . . . . . . . . . . . . . . . . . 113
6.2.1 Scanner Models . . . . . . . . . . . . . . . . . . . . . . . . . 113
6.2.2 Patient Phantom . . . . . . . . . . . . . . . . . . . . . . . . 115
6.2.3 Simulated System Parameters . . . . . . . . . . . . . . . . . 116
6.2.4 Simulation Parameters and Data Processing . . . . . . . . . 117
6.3 Results . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 117
6.3.1 Comparison of NEC Rates for All Scanners . . . . . . . . . . 117
6.3.2 Comparison of NEC Rates for the Cylindrical Scanner with
Different Breast Sizes . . . . . . . . . . . . . . . . . . . . . . 120
6.3.3 Impact of Activity from Outside the Field of View . . . . . . 121
6.4 Discussion and Conclusion . . . . . . . . . . . . . . . . . . . . . . . 122
7 Future Directions
124
7.1 Improvements in Data Corrections and Quantification . . . . . . . . 124
7.1.1 Minimizing the Effects of the Limited PET Transaxial FOV 124
7.1.2 Attenuation Correction . . . . . . . . . . . . . . . . . . . . . 125
7.2 Studies to Estimate the Influence of Patient Related Factors on
Quantification . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 126
7.2.1 Measuring Breast Motion . . . . . . . . . . . . . . . . . . . 126
7.2.2 Optimizing 18 F-FDG Injection Dose . . . . . . . . . . . . . . 130
7.3 Clinical Utility of Quantitative Metrics in Patient Imaging . . . . . 133
7.3.1 Neoadjuvant Therapy Response Monitoring . . . . . . . . . 133
-iv-
List of Figures
1.1
1.2
1.3
1.4
1.5
2.1
2.2
2.3
Reconstruction of PET emission data with filtered backprojection.
(A) Emission data (double sided arrows) acquired with PET (blue
ring) from a digital phantom. Representation of the radial offset
(r) and the angular offset (φ) used in sinogram space is also shown.
The plane parallel to the ring is known as the transaxial or transverse FOV. The dotted line represents a plumb line through the
center. (B) Representation of the coincidence counts in sinogram
space. (C) Estimation of the original source distribution from FBP
reconstructed images. . . . . . . . . . . . . . . . . . . . . . . . . .
Comparison of 2D and 3D PET imaging, displaying schematics of
scanners along the axial direction. (A) 2D scanner with lead septa
(gray bars) allowing LORs with maximum ring difference of +/−1.
(B) 3D scanner with lead septa only at the axial ends (end-shields)
permitting LORs with all possible ring differences. . . . . . . . . .
Examples of PEM scanner geometries. (a) Dual-head planar detector configuration resembling the geometry of the system in Turkington et al. [1]. (b) Monolithic curved plates (partial ring) geometry
resembling the system in Freifelder et al. [2]. . . . . . . . . . . . .
Reconstruction of PEM emission data with filtered backprojection.
(A) Emission data acquired with PEM from a digital phantom. The
in-plane and out-of-plane directions are defined. (B) Representation
of the coincidence counts in sinogram space. (C) Estimation of the
original source distribution from FBP reconstructed images with
significant blurring in the out-of-plane direction visible. . . . . . .
Examples of bPET scanner geometries. (a) Four-head planar detector configuration resembling the geometry of the system in Raylman et al. [3]. (b) Polygonal detector configuration resembling the
geometry of the system in Furuta et al. [4]. . . . . . . . . . . . . .
.
7
.
8
.
25
.
28
.
31
(A) Schematic depicting DbPET/CT. The object between the PET
detectors shows the approximate position of a subject’s breast during scanning. Orientation of the positioned patient’s coronal (C),
sagittal (S), and axial plane are depicted in the bottom right hand
corner. (B) The PET gantry allows for control of detector height
(vertical arrow), separation distance (horizontal line with end markers), and rotation (curved arrow). . . . . . . . . . . . . . . . . . . .
Schematic of PET electronics used for prompts and randoms data
acquisition (DAQ) trigger generation. For a full description see
section 2.4.1. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Main GUI of the control and acquisition software for the PET component of DbPET/CT. . . . . . . . . . . . . . . . . . . . . . . . . .
-v-
36
39
42
2.4
2.5
2.6
3.1
3.2
3.3
3.4
3.5
3.6
3.7
3.8
GUI for the PET component of DbPET/CT allowing for the specification of acquisitions of desired durations and at specific time
points (left) and the entrance of patient information for Interfile
format output. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43
Schematic of PET acquisition software used for the simultaneous
collection of both prompts and delayed coincidences. Dotted boxes
denote distinct threads. Grey color in buffer denotes data that has
not been read. Functions involved in a process are denoted with
closed parenthesis at the end. . . . . . . . . . . . . . . . . . . . . . 44
Breast positioning system used in DbPET/CT.(A) Photo showing the components of the positioning system, including the clear
polycarbonate cylinder and the black central support base with aluminum connector rod. (B) Display of how ports are accessed by a
technician to more accurately center the patient’s breast in the FOV. 47
Complete anthropomorphic breast phantom used to estimate NECR
values during patient imaging. Volumes representing the brain and
bladder are not shown. In the final configuration the breast compartment was not taped to the torso. . . . . . . . . . . . . . . . .
Extended WB PET patient images (maximum intensity projection)
used to estimate injection activity from anthropomorphic phantom
activity. The outline around the head and torso approximates the
region modeled by the anthropomorphic phantom. . . . . . . . . .
Rates versus phantom activity for a right cylinder phantom as estimated from experimental acquisitions. NECR was estimated for
direct(2R) and variance reduce (1R) randoms subtractions. . . . .
Rates versus estimated injection activity for an anthropomorphic
phantom. NECR was estimated for direct(2R) and variance reduce
(1R) randoms subtractions. . . . . . . . . . . . . . . . . . . . . .
Coincidence photon detection sensitivity measured from translating
a 68 Ge point source axially. . . . . . . . . . . . . . . . . . . . . . .
Accuracy of affine registration between the PET and CT as a function of detector height. Error bars represent the range. . . . . . .
Accuracy of affine registration between the PET and CT as a function of reposition number. Error bars represent the range. . . . .
Influence of PET electronics and activity on CT image quality for
HV off and no activity in the FOV (HV- Act-), PET HV on and no
activity (HV+ Act-), and PET HV on and activity present (HV+
Act+). MTF vs. line pair frequency (left). Image uniformity (mean
and standard deviation bars) as a function of CT coronal slice number (lower magnitude is more posterior) (right). Standard deviation
bars are representative of typical values and are staggered between
imaging scenarios for clarity. . . . . . . . . . . . . . . . . . . . . .
-vi-
.
53
.
54
.
62
.
64
.
66
.
67
.
67
.
68
4.1
4.2
4.3
4.4
4.5
4.6
4.7
5.1
DbPET/CT images from the affected breast of the case 1 subject.
(A) Sagittal tissue section excised from a mastectomy sample of
the case 1 subject’s affected breast with 4 areas (boxes) of histology
performed. (B) Histology tissue slides with magnified regions (right,
corresponding to black boxes) revealed DCIS alone (i-ii), or with
intralymphatic invasion (iii, not shown), and benign tissue (iv).
(C) DbPET/CT, (D) WB PET/CT, and (E) DCE-MR sagittal
image slices corresponding to the tissue section (A). Boxes in the
DbPET/CT image (C) are at locations approximating those in the
tissue section (A). PET images (C and D) were windowed between
0 and 60% maximum image intensity. . . . . . . . . . . . . . . . .
Axial DbPET/CT images from the affected breast of the case 2
subject. Panels from left to right represent the fused images and the
PET alone. Measurement given in the fused image is the distance
between the top of CT and PET FOV. PET images were windowed
between 0 and 75% maximum image intensity. . . . . . . . . . . .
Coronal DbPET/CT images from the affected breast of the case 3
subject. Shown are the CT (A), PET (B), and fused image. Arrow
in (A) denotes a calcification at the approximate location of biopsy
confirmed DCIS. . . . . . . . . . . . . . . . . . . . . . . . . . . .
(A) Pre-contrast CT, (B) fused PET/CT, and (C) contrast subtraction sagittal DbPET/CT images showing the affected breast of
the case 4 subject. Two areas of focal uptake were seen on PET
(B) and on contrast subtraction CT (C) (arrows). (B) The distance
(opposing arrows) between the top of the PET axial FOV (dashed
line) and anterior aspect (solid line) of the pectoralis muscles (dotted line) is shown. (C) The contrast subtraction image is an average
of 7 slices and uses alternative windowing. . . . . . . . . . . . . .
Plot of the STR versus breast volume in the PET FOV for patient scans. Data was fitted with a first order polynomial (–) with
correlation coefficient (R2 ) = 0.72. . . . . . . . . . . . . . . . . . .
Comparison of patient rates with anthropomorphic phantom data
measured from section 3.3.3. (A) Comparison of trues and NECR
and (B) comparison of randoms as a function of estimated injected
activity. Activity for the patient data represents the normalized
injection activity. . . . . . . . . . . . . . . . . . . . . . . . . . . .
.
75
.
76
.
76
.
77
.
77
.
79
.
82
CT based ACF estimation for a patient image set. (a) The original
CT image, (b) the segmentation of (a) to a uniform linear attenuation value and resolution matched to the PET, (c) the registration
of (b) to the PET reference frame and (d) the forward projection of
(c) into sinogram space. The red line in (c) denotes the approximate
coronal slice for which the sinogram in (d) corresponds. . . . . . . .
90
-vii-
5.2
5.3
5.4
5.5
5.6
5.7
Schematic of the MC scatter estimation. Key: t=trues sinogram,
s=scatters sinogram, r =randoms sinogram, AT =attenuation, Iter.=iteration
number. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 91
Phantoms used for the assessment of dead-time and randoms correction accuracy.(a) HDPE right cylinder with line source offset 3.8
cm from the center alone or (b) combined with a uniform filled
cylinder (outer diameter=7.5 cm, height=11.1 cm) placed outside
the FOV. The position of the phantoms with respect to the detector
heads is visible in (b). . . . . . . . . . . . . . . . . . . . . . . . . . 93
Phantoms used for attenuation validation and assessment of accuracy for scatter correction. (a) Schematic of digital phantom used in
attenuation validation, with hot (H), background (B), and cold (C)
compartments. (b) Photograph and (c) schematic of fillable acrylic
phantom used for assessing scatter correction accuracy. Key: OD
= outer diameter, ID= inner diameter. . . . . . . . . . . . . . . . . 94
Accuracy of dead-time and randoms corrections. (a) Trues and scatters versus estimate of average energy windowed singles for incident
rates (Linear-Fit), data fully corrected for dead-time and randoms
(Corrected), and data without any corrections (Uncorrected). (b)
Residual error between incident and fully corrected prompts ROI
for activity inside the FOV alone (Corrected) or with additional
activity OFOV (Corrected w/ OFOV Act.), or with activity inside
the FOV alone and all corrections except LTU E (w/o LTU E Correction). Vertical lines indicate approximate range of singles observed
during patient imaging and error bars show min and max differences
across the axial FOV. . . . . . . . . . . . . . . . . . . . . . . . . . . 98
Ratio histogram of raw to variance reduced randoms for a scan of
an offset uniformly filled cylinder phantom. Displayed as crystal
j + Nr v versus i + Nr u for clarity (see section 5.2.1). . . . . . . . . 100
Accuracy of attenuation correction as determined through MC simulations. (a) Transaxial reconstructed image of the activity distribution with an all air attenuation map (True) depicting position of
line profiles and circular ROI. Comparison of transaxial line profiles
drawn through the (b) background and the (c) hot and cold cylinders of the phantom. (d) Percent difference of background profiles
between the True and AC images. Vertical gray lines on (b)-(d)
represent the transaxial extent of the phantom. . . . . . . . . . . . 101
-viii-
5.8
Scatter correction performance for experimental scans of a phantom with asymmetric activity. (a) Comparison of transaxial line
profiles drawn through the cold and hot cylinders for reconstructed
images with (w/ SC) or without (w/o SC) scatter correction, and
the MC scatter estimate itself (MC S) after two iterations of scatter estimation. (b) Reconstructed transaxial images without scatter
correction and (c) with scatter correction, with display window upper limit = 35% of maximum. Profiles and images were averaged
over 30 axial slices. . . . . . . . . . . . . . . . . . . . . . . . . . . .
5.9 Mean CRCcold as a function of transaxial slice number taken over
the entire length of the cold compartment for a phantom containing asymmetric activity distribution. Results are for images reconstructed with all corrections excluding (w/o SC) or including (w/
SC) scatter correction. The 60th axial slice represents the approximate edge of the cold rod compartment and the warm background.
5.10 Transaxial images of a uniformly filled phantom from a high count
scan. All images were corrected for LT, attenuation, randoms, and
scatter. (a) Images with no normalization applied, (b) geometric
(Ωuivj ) normalization only, and (c) both Ωuivj and detector efficiencies (εui εvj ) applied. Top row: gray scale windowing set to the full
dynamic range. Bottom row: gray scale minimum set to 70% the
image maximum. . . . . . . . . . . . . . . . . . . . . . . . . . . . .
5.11 Assessment of image uniformity after all corrections for a uniformly
filled phantom. (a) Difference of mean annular ROI values, with
respect to the volume mean, taken across the transaxial FOV. Min
and max represent mean ROI values at a given radius across all
images slices, and the CFOV is at an annular radius = 0. (b) Mean
of all voxels covered by annular ROI on a slice-by-slice basis. Min
and max are mean annular ROI values across the transaxial image
plane for a given axial slice. . . . . . . . . . . . . . . . . . . . . . .
5.12 Comparison of transaxial line profiles drawn through reconstructed
images of a uniform cylinder after all corrections. Profiles shown
include an average taken over 41 slices (Mean), and at two different transaxial slice numbers. The transaxial CFOV is at a profile
location of 0. Slice numbers correspond to those in figure 5.11(b). .
6.1
6.2
6.3
103
104
105
106
107
Schematics of the scanner geometries simulated. Systems included a
(A) planar dual-head, (B) cylindrical, (C) split-ring, (D) five-sided
box, and (E) DOI capable cylindrical cameras. . . . . . . . . . . . . 113
Complete geometrical simulation model. The anthropomorphic phantom is composed of the brain, bladder, NCAT, and breast volumes. 114
Overlay of sagittal slices for the small (S), medium (M), and large
(L), sized breasts. The red line denotes the beginning of the axial
FOV for all scanners. . . . . . . . . . . . . . . . . . . . . . . . . . . 114
-ix-
6.4
6.5
6.6
6.7
7.1
NEC rates versus injected activity for the 4 geometries considered
when imaging the medium sized breast phantom. The vertical line
indicates 20 mCi injected dose (typical for 18 F-FDG imaging). Head
separation distances for the split-ring and planar dual-head geometries were 159 mm and 147 mm, respectively. . . . . . . . . . . . . .
NEC rates versus injected activity for the cylindrical (without DOI
capabilities), DOI scanner (cylindrical geometry), and current planar dual-head prototype, with the medium breast phantom. The
DOI scanner does not show peak NEC rates even at injected values
> 50 mCi. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
NEC rates versus injected activity for the cylindrical scanner imaging several breast sizes. Results for the small, medium, and large
sized breast volumes (left). Magnified NEC rates axis for the small
sized breast volume (right). . . . . . . . . . . . . . . . . . . . . . .
Maximum intensity projections from the same view of 3D histograms
representing the actual activity distribution (A) and the origin of
received singles (B) from the anthropomorphic phantom. Images
were normalized by the total number of counts. . . . . . . . . . . .
118
119
120
121
Method to increase the transaxial FOV for the PET component of
DbPET/CT. (A) Transaxial viewpoint showing original (dashed)
and 3.2 cm offset centerline (solid). (B) View from the front of a
detector head. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 125
-x-
List of Tables
1.1
1.2
1.3
Description of detectors and geometry for several PEM systems. . .
Summary of clinical trial results for PEM imaging. . . . . . . . . .
Description of detectors and geometry for several bPET systems. . .
27
29
33
2.1
2.2
CT System Characteristics . . . . . . . . . . . . . . . . . . . . . . .
PET System Characteristics . . . . . . . . . . . . . . . . . . . . . .
37
38
3.1
Transverse spatial resolution (mm ± inter-slice σ) estimated from
MAP based reconstructions. . . . . . . . . . . . . . . . . . . . . . .
Axial spatial resolution (mm ± inter-slice σ) estimated from MAP
based reconstructions. . . . . . . . . . . . . . . . . . . . . . . . . .
Peak, and 95% of peak NECR values, with corresponding activities,
for scans of an anthropomporphic phantom. . . . . . . . . . . . . .
64
4.1
4.2
Radiological Interpretation for DbPET/CT Affected Breast Images
NECR Values from Patient Scans . . . . . . . . . . . . . . . . . . .
74
78
5.1
PET performance characteristics of the DbPET/CT scanner during
patient imaging. . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Mean (over all axial slices) and max RMSE (%) taken over singles
rates observed during patient imaging for various combinations of
dead-time and randoms corrections. . . . . . . . . . . . . . . . . .
ROI measurements of activity concentration (intensity/ml) (mean
± inter-axial slice σ) from true and attenuation corrected (AC)
cylinder phantom images. . . . . . . . . . . . . . . . . . . . . . .
Contrast recovery coefficients (CRC)(%) (mean ± inter-transaxial
slice σ) for images of an asymmetric activity distribution with or
without scatter correction. . . . . . . . . . . . . . . . . . . . . . .
3.2
3.3
5.2
5.3
5.4
6.1
6.2
6.3
61
61
.
85
.
99
. 102
. 104
Volume of digital breast phantoms . . . . . . . . . . . . . . . . . . . 115
Simulated NEC rates and scatter fractions for several geometries . . 118
Simulated NEC rates for cylindrical scanner with different breast
sizes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 120
-xi-
Abstract of the Dissertation
Quantification in fluorine-18-fluorodeoxyglucose dedicated breast
PET/CT
Whole body (WB)
18
F-fluorodeoxyglucose (18 F-FDG) positron emission tomogra-
phy (PET) images cellular glucose avidity and has shown clinical utility in breast
cancer staging, restaging, and therapy response assessment. Quantitative and
semiquantitative metrics, most notably the standardized uptake value (SUV), are
integral to such applications. For accurate quantification in PET, images must
have voxel intensities proportional to a corresponding activity concentration in
the subject and are generated by the correction of emission data for count losses,
noise, and the system response.
The combination of WB PET with x-ray computed tomography (CT) in a
single platform (PET/CT) has been shown to have increased utility over either
PET or CT alone for the management of breast cancer. The CT component allows
for the creation of fused images, showing the location of
18
F-FDG uptake on an
anatomical background. With both WB PET and PET/CT, however, detection
and quantification of tracer uptake is significantly reduced when lesions are small
(< 1 cm diameter).
In an effort to improve the performance of PET/CT for primary breast cancer
imaging our group has constructed a hybrid dedicated breast PET/CT scanner,
DbPET/CT. The goal of this research is to characterize and correct for the factors
influencing image quantification in the PET portion of the system, and explore
methods to improve quantification with alternative dedicated breast PET system
-xii-
designs.
As a proof-of-principle study and to measure the magnitude of factors influencing quantification in DbPET/CT imaging we performed a clinical trial with women
highly likely to have breast cancer. Using the system performance results measured
from this clinical trial as a guide, we developed hardware and software emission
data correction schemes and validated these methods with custom performance
measurements. Additionally, we used Monte Carlo simulations with anthropomorphic models to determine quantification trade-offs between alternative dedicated
breast PET geometries.
-xiii-
List of Abbreviations
AC- attenuation correction
ACD- annihilation coincidence detection
ACF- attenuation correction factor
bCT- dedicated breast computed tomography
bPET- dedicated breast positron emission tomography
CC- craniocaudal
CFD- constant fraction discriminator
CFOV- center of the field of view
CM- center of mass
COV- coefficient of variance
CRC- contrast recovery coefficient
CT- computed tomography
DAQ- data acquisition
DbPET/CT- U.C. Davis bPET/CT scanner
DCE-MRI- dynamic contrast enhanced magnetic resonance imaging
DCIS- ductal carcinoma in situ
DOF- degree of freedom
DOI- depth of interaction
18
F-FDG-
18
F-fluorodeoxyglucose
FBP- filtered back projection
FIFO- first in, first out buffer
FORE- Fourier rebinning algorithm
-xiv-
FOV- field of view
FWHM- full-width at half maximum
FWTM- full-width at tenth maximum
GATE- Geant4 Application for Tomographic Emission
GUI- graphical user interface
HU- Hounsfield units
HV- high voltage
HVL- half-value layer
IDC- invasive ductal carcinoma
ILC- invasive lobular carcinoma
LLD- lower level discriminator
LOR- line of response
LSO- lutetium oxyorthosilicate
LT- live-time
LUT- lookup table
MAP- maximum a posteriori
MC- Monte Carlo
MLO- mediolateral oblique
MoCap- optical computational stereo vision motion capture
MRI- magnetic resonance imaging
MTF- modulation transfer function
NECR- noise-equivalent count rate
NIM- nuclear instrumentation module
-xv-
OD- outer diameter
OFOV- out of the field of view
PEM- positron emission mammography
PET- positron emission tomography
PMT- photomultiplier tube
PS-PMT- position-sensitive photomultiplier tube
RMSE- root mean squared error
ROI- region of interest
SF- scatter fraction
SimSET- Simulation System for Emission Tomography
SNR- signal-to-noise ratio
SPECT- single photon emission computed tomography
SSRB- single-slice rebinning algorithm
STR- singles-to-trues ratio
SUV- standardized uptake value
ULD- upper level discriminator
WB- whole-body
-xvi-
Acknowledgments
The completion of my dissertation and doctorate would not have been possible
without the support, collaboration, and guidance of numerous individuals. I would
first like to thank my advisor Professor Ramsey Badawi for providing invaluable
direction in my research, mentoring during the paper writing process, and numerous opportunities to present my work at conferences. It’s been a pleasure and
honor to work with him from the beginning of his time here at U.C. Davis Medical
Center.
I would also like to thank my other dissertation committee members including
Dr. Simon Cherry and Dr. John Boone for invaluable career advice and significantly furthering my understanding in the fields of both PET and CT. Acknowledgments go to members of my qualifying exam committee not already mentioned,
including Dr. Alexander Borowsky and Dr. Jinyi Qi for providing beneficial reviews and suggestions for my research.
I would like to thank current and former members of the Cherry, Qi, Boone,
and Badawi lab groups. The feedback I have received from this group both in
and outside of lab meetings, and the process of learning about the many different
projects being researched in these labs, has instilled in my a depth of understanding
in my own work and molecular imaging as a whole that I doubt I could have
obtained anywhere else.
In the Badawi group I would particularly like to acknowledge Dr. Abhijit
Chaudhari for numerous useful discussions, career guidance, and assistance with
experiments and patient imaging, as well as Felipe Godinez, Andrea Ferrero and
-xvii-
Quan Zeng for technical assistance. In the Qi lab I would like to thank Dr. Lin
Fu for his immense assistance with image reconstruction. Acknowledgments go to
Dr. Yibao Wu in the Cherry group for education of the breast scanner. I would
also like to thank Dr. Nathan Packard, Dr. Kai Yang, and George Burkett in the
Boone group for contributions relating to the breast CT system.
From the UC Davis Medical Center I would like to acknowledge Nikki Emerson,
Sheila Rejano, Tina Luthge, Tashina Hayduk, Naomi Miyao, and John Brock for
assistance with patient scans. Additional thanks go to Dr. Karen Lindfors, Dr.
David Shelton, and Dr. Steve Martinez for contributions to patient imaging.
Finally, I could not have maintained my motivation and commitment to earning my degree without the deep and continual support of my family and friends.
To my parents Valrae and Jerrold Bowen, my brother Nathan Bowen and his family Stephanie, Jude, and Everett, and lastly my girlfriend Caroline Jones, this
dissertation is dedicated to you.
-xviii-
1
Chapter 1
Background and Significance
1.1
Introduction
Medical imaging allows for the noninvasive assessment of physiological processes
and anatomy. Images are generated from spatially localized magnitude measurements of the energy distribution in, or interaction with, tissue of the subject. The
specific energy used and method of detection determines the exact physiological
processes or anatomy that ultimately produce image contrast.
An important component of medical imaging in many clinical applications is
the quantification of image data. More specifically quantification in this instance
refers to the measurement of static or dynamic contrast intensities or linear dimensions. Accurate quantification in medical imaging requires design optimizations
and corrections for physical phenomena, related to the generation, detection, or
interaction of energy with the subject, that influence contrast in a manner that
is not directly due to the primary imaging mechanism. Even with optimal design
tradeoffs and full corrections all medical images suffer from some degree of bias
(displacement from the mean) and variance (uncertainty around the mean) which
2
influences the accuracy and precision, respectively, of quantitative metrics.
Second to cancers of the skin, breast cancers are the most common type of cancer diagnosed for women [5]. Medical imaging is used routinely in the management
of this disease in applications including screening, diagnosis, staging, therapy response monitoring, and restaging [6], and quantitative metrics have a role in several
such applications.
The work presented in this dissertation is concerned with accurate quantification for a dual-modality positron emission tomography and x-ray computed tomography system designed specifically for breast imaging.
1.2
Theory of Positron Emission Tomography
Positron emission tomography (PET) is a highly sensitive nuclear imaging modality capable of delivering quantitative functional information. In a PET study,
the subject to be imaged is injected with a radionuclide labeled molecule (tracer)
that decays largely through positron (β+) emission [7]. The distribution of the
tracer can then be imaged in a process known as annihilation coincidence detection
(ACD) using specialized detectors that encircle the subject [8]. In positron emission, the β+ particle will typically migrate a short distance from the tracer decay
location before interacting with an electron, and producing two back-to-back 511
keV annihilation photons. ACD refers to the process of detecting both of these
photons, in electronic coincidence. All possible coincidences between these two
detectors can then be thought of as forming a line or volume, known as a line or
response (LOR). Using the number of coincidences for all possible LORs, tomographic algorithms can be used to reconstruct images approximating the original
3
distribution of tracer in the subject.
Although many tracers have been developed for PET imaging,
18
F-fluoro-2-
deoxy-D-glucose (18 F-FDG) is the most commonly used clinical tracer [7].
18
F-
FDG is a sugar analog whose physiological uptake is increased for cells with upregulated glycolysis, particularly for cancer cells [9]. For intravenous delivery to
the patient an aqueous solution of 10-20 mCi of 18 F-FDG is injected via a catheter
to an antecubital vein. Once in circulation
18
F-FDG travels into the interstitial
space through simple diffusion and is taken up by cells via transmembrane proteins
(glucose transporters) where it is phosphorylated with hexokinase to form
FDG-6-PO4 . In the phosphorylated form
18
18
F-
F-FDG-6-PO4 is effectively trapped
in the cell and has a very low probability of undergoing the remaining steps of
glycolysis. For breast cancers the increase in
18
F-FDG uptake has largely been
attributed to the upregulation of the glucose transporter GLUT-1 [10]. After ∼2
hours approximately 50% of the administered 18 F-FDG dose is cleared through the
kidneys [11]. Advantages of 18 F-FDG include the relatively long half-life of the 18 F
radionuclide (109.8 minutes) and its application to many disease processes.
Largely from the interaction of the emitted β+ particle with tissue
18
F-FDG
delivers radiation dose the patient. Exposure to low dose ionizing radiation of
the type typically employed in medical imaging can increase the risk of the patient
developing solid cancers and leukemia [12]. For the purposes here we are interested
in the equivalent radiation dose which is defined as the amount of energy absorbed
per a unit mass, weighted by the relative biological damage of the radiation type
used, and is defined in units of sieverts (Sv= 1 J/kg) [7]. For the radiation types
4
typically used in medical imaging, including x-rays, γ rays, electrons, and positrons,
this weighting factor is the lowest possible value and =1. Furthermore, different
tissues are more susceptible to radiation dose than others, and the scaling of the
equivalent dose based on these weights is termed the weighted equivalent dose.
The sum of all weighted equivalent doses for all organs of the body is termed the
effective dose. For WB PET imaging with 10 mCi of
18
F-FDG the effective dose
to the patient has been estimated at ∼ 7 mSv, with the most significant weighted
equivalent dose delivered to the bladder wall [13]. In comparison, the annual
effective dose from background radiation is ≤ 3 mSv for persons in the United
States [12]. The addition of a CT scanner for dual-modality imaging increases the
dose substantially, with effective dose for a 10 mCi injection of
18
F-FDG and a
CT acquisition composed of a topogram (scout scan) and low-dose CT ∼ 25 mSv
(kVp=110-120, mAs=32-60) [13] (see section 1.4).
The detectors in PET systems allow for the detection of 511 keV γ rays from
β+ annihilations. Detector units typically consist of a rectangular block of highly
attenuating inorganic scintillator material coupled to one or more photodetectors.
The scintillator converts the energy absorbed from Compton and photolectric interactions into light pulses which are subsequently converted into electronic pulses
via the photodetectors. The amplitude of electronic pulses is proportional to the
energy deposited in the scintillator, allowing for discrimination of counts based on
energy. For PET, scintillator development focuses on increasing the linear attenuation coefficient for 511 keV photons, improving the amplitude of light output per
a unit of absorbed energy, and reducing the decay time of the light pulse. Scintil-
5
lators that have been used in PET imaging include sodium iodide (NaI), bismuth
germinate (BGO), germanium oxyorthosilicate (GSO), and lutetium oxyorthosilicate (LSO). The photomultiplier tube (PMT) is the most commonly used light
detector and functions by amplifying scintillation photons incident on the window
of the PMT (photocathode) by a factor of > 105 through use of a dynode structure
[8]. Detector units are typically arranged in a polygon (ring) configuration (see
figure 1.1) often with the light detectors positioned facing towards the center of the
polygon. For finer spatial sampling of LORs the scintillator material is partially
or fully segmented into individual crystal (crystal array) elements and read out
with an array of single-channel PMTs or a position-sensitive PMT, respectively.
To minimize attenuation length the long axis of the crystal elements are positioned
roughly parallel to a line pointing towards the center of the scanner. The use of
an additional photodetector on the opposing side of the crystal array [14] or segmentation of the crystals along the long axis of the crystal elements [15] allows for
determination of the depth of interaction (DOI) of the 511 keV photons, which
can significantly improve spatial resolution uniformity in reconstructed images.
Acquisition electronics and software provide positionining, energy windowing
and ACD of events and write data to storage for post-processing. The X-Y positioning of events (plane perpendicular to the long axis of the crystal elements)
in the scintillator array is first performed by taking the ratio of pulse amplitudes
from the separate readout channels of the PMT(s) (Anger logic)[16]. The crystal of interaction is then estimated from crystal position lookup tables (LUTs)
generated from the high count irradiation of the detector with a 511 keV source.
6
Energy windowing is also performed to reduce noise from electronics and external factors, and involves only keeping events between a lower level discriminator
(LLD) and upper level discriminator (ULD). To perform ACD, electronic triggers
of duration τ seconds (coincidence window) are generated for valid singles events
and compared with a logical AND operator. Singles are defined as detected γ
rays by individual detector blocks. Subsequently, singles with triggers that have
an absolute time difference of ≤ τ , such as those generated from the back-to-back
annihilation photons, are defined as prompts. A non-zero coincidence window is
required due to lack of precision in singles trigger generation, known as the timing
resolution, and due to variations in the path length along the LOR of the two
photons (time-of-flight phenomenon), and is typically set at τ ≈ 6 ns for LSO
based detector systems [17, 18]. Due to the use of a non-zero τ there is a singles
rate dependent probability that a coincidence will occur from singles emanating
from separate annihilations, termed randoms (see section 1.5.2). As singles events
between detectors are uncorrelated in time for randoms events, randoms can be
estimated by delaying the singles trigger for one detector before coincidence logic;
a method known as delayed coincidence detection.
Coincidences from a PET acquisition are sorted into histograms, termed sinograms, where each bin represents the number of coincidences for every possible
LOR. Three dimensional images estimating the original activity distribution are
then reconstructed from transformations of the sinogram data. Historically analytical algorithms have been used for PET reconstruction, although iterative methods
are now more commonly employed. In the analytical algorithm, filtered backpro-
7
φ
C
B
A
r
r
Figure 1.1. Reconstruction of PET emission data with filtered backprojection.
(A) Emission data (double sided arrows) acquired with PET (blue ring) from
a digital phantom. Representation of the radial offset (r) and the angular
offset (φ) used in sinogram space is also shown. The plane parallel to the ring
is known as the transaxial or transverse FOV. The dotted line represents a
plumb line through the center. (B) Representation of the coincidence counts in
sinogram space. (C) Estimation of the original source distribution from FBP
reconstructed images.
jection (FBP), each projection (row in sinogram space) is filtered by a kernel,
before values from sinogram bins are assigned to lines of underlying image voxels (backprojected) based on their overlap with the corresponding LOR [19]. The
filtration step normalizes out the impulse response of the backprojection process.
The summation of all backprojections for projections from all φ forms the final
image. Figure 1.1 shows a schematic of sinogram binning and FBP.
Iterative reconstruction methods employ statistical noise models and optimization algorithms to solve the equation:
y = Px
(1.1)
where y is a vector of the emission data for each LOR, P is the system matrix, and
x is a vector of the activity concentration at each image voxel. The system matrix
specifies the probability of detecting a coincidence at each LOR with respect to
8
A
B
Figure 1.2. Comparison of 2D and 3D PET imaging, displaying schematics of
scanners along the axial direction. (A) 2D scanner with lead septa (gray bars)
allowing LORs with maximum ring difference of +/−1. (B) 3D scanner with
lead septa only at the axial ends (end-shields) permitting LORs with all possible
ring differences.
ˆ , represents the final image
each voxel in the image domain. The estimate of x, x
and takes several repeated calculation steps, iterations, to converge to an accurate solution. Iterative methods have several advantages over FBP reconstruction,
including: a relative reduction in image noise, recovery of spatial resolution, and
lower sensitivity to missing projection data [20]. Although the discussion here has
focused on sinograms, commonly projection data is now being saved in list-mode
format: a binary file with an entry for each coincidence event. As many elements
in a sinogram will have 0 counts, list-mode format can reduce data storage space
significantly.
PET systems can acquire LORs between detectors not only in the transaxial
direction (see figure 1.1) but also between detectors along the length of the patient
port (axial direction). Detector elements in the axial direction are termed rings.
Acquisitions where LORs with only minimal ring differences (e.g. +/ − 3) are
allowed are termed 2D scans, where as those allowing LORs with all ring differences, or a slightly reduced subset thereof, are 3D scans. Figure 1.2 depicts both
2D and 3D acquisitions. PET scanners were originally exclusively operated in 2D
9
mode, although WB systems that operate only in 3D mode are becoming common [21, 22]. Systems operating in 3D mode have significantly higher coincidence
photon sensitivity (see section refperformance:materials:sensitivity) compared to
2D scanners, but at the cost of increased susceptibility to noisy events, such as
randoms (see section 1.5), and larger data sets [23].
1.3
Theory of X-Ray Computed Tomography
Due to its ability to produce fast, highly-resolved (<1 mm), and quantitative
anatomical images, x-ray computed tomography (CT) has become one of the most
widely used clinical imaging modalities. For image acquisition the detector and
source rotate around a centrally located subject. At each rotation angle, the projection of the subject onto a detector element represents the temporally integrated
photon flux. The magnitude of this photon integrated measurement (It ) depends
on both the linear attenuation coefficient (µ) of the tissue, and the path length of
tissue (T ) traversed between the source and pixel of interest, and is expressed with
the Beer-Lambert-Bouguer Law as follows:
It = Io exp (−µT )
(1.2)
where Io is the unattenuated integrated flux measurement. The linear attenuation
coefficient accounts for absorption by photoelectric and Compton interactions and
is determined from narrow-beam geometry measurements [24]. For biological tissues of interest and at the x-ray energies typically employed interactions due to
Compton scattering dominate µ. The Compton cross section is proportional to
the density of the tissue (ρ), the atomic number (Z) and inversely proportional
10
to the atomic mass (A). As the ratio of Z/A = 0.5 for several abundant atoms
in organic matter (oxygen, carbon, and nitrogen), the Compton cross section is
mainly influenced by ρ [24]. After calculating the product µT , via (1.2), analytic
reconstruction methods are used to generate 3D image sets where each voxel is
equal to the µ of the tissue segment.
The production of x-ray photons is accomplished by the acceleration of electrons
through a high voltage field. Electrons are generated from a negatively charged
filament (cathode) and collide with the positively charged metal anode, whereby
characteristic and bremsstrahlung x-ray photons are resultant [24]. The maximum
energy of x-ray photons is dependent on the voltage between the cathode and
anode. For example, an 80 kVp tube voltage will result in 80 keV x-rays. The flux
of x-ray photons is determined by the filament current of the cathode. The resulting
energy of the bremsstrahlung x-ray photons is an inverse and continuous function
with respect to the distance between the incident electron and the nucleus, and
as such a broad continuous x-ray spectrum results. Characteristic x-rays originate
from the ionization of inner shell electrons and have a discrete pattern specific to
the anode material. Tungsten anodes (W) are commonly used due to Tungsten’s
high melting point and atomic number (Z=74).
Detectors used in CT convert x-ray fluxes into charge that can be digitized and
processed by a computer. Many current CT scanners employ indirect detectors
composed of a x-ray intensifying screen coupled to a pixelated solid-state photodetector. The intensifying screen converts absorbed x-ray energy into scintillation
light and is often composed of columnar CsI to reduce the light spread of scin-
11
tillations [24]. The photodetector uses thin-film transistors (TFTs) to read out
the integrated charge of individual pixels. Research and commercial efforts have
focused largely on increasing the number of pixel elements (m) along the longitudinal direction of the detector [25]. CT systems using detectors with m > 1
are multi-detector row or 7th generation systems. Use of m detector rows enables
a factor of m increase in acquisition speed compared with single slice systems if
all other parameters are kept constant, or alternatively an m increase in volume
coverage for the same acquisition time. Multi-detector row CT has advantages in
numerous applications involving vascular and cardiac imaging [25]. Along with the
advantages, however, multi-detector row CT can suffer from longitudinal artifacts
due to use of a cone-beam x-ray geometry and an increase in detection of Compton
scattered x-rays [26] which can both reduce quantitative accuracy.
To remove the dependence of estimated µ values on the particular CT scanner
employed the voxel intensities are typically calibrated to Hounsfield units (CT
numbers), which normalizes linear attenuation coefficients in each voxel (µ (x)) by
that of water (µwater ) as follows:
CT (x) = 1000
µ (x) − µwater
µwater
(1.3)
where CT (x) is the CT number for the voxel specified by vector x. With this
calculation air has a CT number = -1000, water a value = 0, soft tissue has a CT
number range of -300 to -100, and bone a CT number range of 160-1090 [24, 27].
Although x-ray CT as described herein has been defined as an anatomical imaging modality, the use of contrast agents allows for the visualization of functional
processes. Iodinated contrast agents are most commonly used and derive their
12
contrast from the significantly higher atomic number of iodine (Z=53) compared
to atoms typically found in tissue. For iodinated intravascular contrast media
the molecular structure consists of iodine atoms bound to a benzene ring and is
typically nonionic to reduce toxic adverse reactions [28]. Upon intravascular injection the molecules rapidly diffuse into the plasma volume before leakage into the
extra-cellular space whereby they are cleared via passive filtration of the kidneys
[29]. To image the contrast agents, electron beam or multi-slice CT scanners are
used to acquire a tomographic images both before and immediately after contrast
injection. Frequently, the baseline and contrast enhanced images can be compared
directly or after subtraction. Iodinated contrast agents have been found to have
particular utility in oncology. Malignant tumors must undergo angiogenesis to
grow beyond ∼2 mm in size, and the blood vessels generated in the process have
abnormal physiology, including hyperpermeability, which can lead to increased contrast perfusion compared to normal physiological enhancement [29]. Oncological
applications where this technique is used include detection of pulmonary nodules
[30], detection of colorectal polyps [31],and staging, particularly for hepatic masses
[32], among others. An alternative method for using contrast agents with CT, is
dynamic imaging, in which a rapid series of images is taken immediately before
and after contrast injection. By including the abdominal aorta, the blood input
function can be determined and a measurement of perfusion to the area of interest
calculated [29].
13
1.4
Theory of Combined PET/CT
The combination of WB PET with x-ray computed tomography (CT) in a single
platform (PET/CT) has been shown to have increased utility over either PET or
CT alone for several oncological imaging tasks [33]. The CT component allows
for the creation of fused images, showing the location of
18
F-FDG uptake on an
anatomical background, and allows the use of the low-noise x-ray scans for attenuation and scatter corrections (see section 1.5). The first efforts in integrating
emission and x-ray computed tomography systems in a single platform were performed by Lang et al. [34] with the development of a SPECT/CT scanner and the
first combined PET and CT system was introduced by Beyer et al. [35].
For modern systems the PET and CT scanners are separate cameras which
share the patient port and are placed in very close proximity. For acquisition
the patient is positioned and scanned with a scout scan (topogram) by CT to
determine the axial scan range and then imaged by diagnostic or low-dose CT.
The patient bed is moved to the start position and the subject is scanned by
PET (6-10 minutes per a bed position). Combined PET/CT scanners permit
the generation of accurate spatially registered fused images (especially for easily
deformable organs) which gives this platform the following advantages in the clinic
compared to scanning with PET or CT alone: differentiation between normal
physiological and pathological tracer uptake, accurate localization of suspicious
uptake to anatomy, and increased diagnostic information for a given lesion [36].
In addition, the attenuation correction made possible by the CT images allows for
a significant reduction in total scan time compared to prior measured attenuation
14
correction methods.
1.5
1.5.1
Factors Influencing Image Quantification
Scatter and Attenuation
The influence on image quantification by photon scatter and attenuation has been
well characterized for the case of 3D PET. Scattered coincidences are defined as
those for which one or both annihilation photons have undergone a Compton interaction before detection. Consequently, the LOR resulting from a scattered coincidence will often not intersect the positron annihilation location. The magnitude
of scattered events in the field of view (FOV) is related to the amount of material
surrounding the activity, energy window, energy resolution of the detectors, and
dimensions of the scanner [37]. Although the majority of photons are scattered in
the subject, Qi et al. measured as much as 33% inter-crystal scatter in a bPET
camera [38]. Cherry et al. showed that images not corrected for scatter have
increased contrast in areas with attenuation coefficients less than water, and decreased contrast in regions with attenuation greater than water [39]. The structure
of the scatter is of low spatial frequency and correlates little with the distribution
of activity and scattering medium [40].
The attenuation of 511 keV photons from photoelectric or Compton interactions in the tissue of the subject leads to a loss in the number of recorded coincidences. The probability of a detecting a coincidence (P ) from back-to-back
photons traversing a LOR through tissue thickness (T ) is defined as follows:
P = exp (−µ511keV T )
(1.4)
15
where µ511keV is the linear attenuation coefficient in cm−1 of the tissue for 511
keV photons [7]. The µ511keV for biologically relevant tissues is dominated by
losses from Compton interactions and its value ranges from 0.090-0.170 cm−1 [41].
PET images of uniform activity distributions not corrected for attenuation show
a characteristic cupping artifact that is highly dependent on the structure of the
subject. For patient images several trends have been noted for images uncorrected
for attenuation, including artificially high uptake for lesions in the lung, whereas
those in the mediastinal regions are typically lower than actual [42].
1.5.2
Randoms
Accidental, or random, coincidences result from the detection of photons originating from separate annihilations. The rate of randoms can be estimated from the
recorded rate of singles incident on a pair of detectors as:
R = 2τ S1 S2
(1.5)
where τ is the coincidence window and S1 and S2 are the recorded singles rates.
In (1.5) it is assumed that the the probability of singles events occurring in time
is independent for S1 and S2 fluxes. Images not corrected for randoms suffer from
overestimation of activity in the FOV and contain low frequency spatial information that is not highly dependent on the activity distribution [43]. Besides its
dependence on singles rates the magnitude of recorded randoms is dictated largely
by the scanner geometry, shielding, and energy windowing. 3D systems are especially prone to randoms from activity out of the FOV (OFOV). For brain scanning
on the ECAT EXACT3D Spinks et al. showed that the rate of OFOV randoms
was reduced by a factor of 3 using a specialized 24 mm lead septa compared to the
16
case of no shielding [44].
1.5.3
Dead-Time
Dead-time is a well known problem in PET systems and refers to the loss of one
or more singles or coincidence events due to scintillator physics and acquisition
electronics [45]. Since dead-time causes the rate of trues to become non-linear as
a function of activity, significant bias can be introduced into reconstructed images
[46]. In addition, the count losses caused by dead-time reduce the signal-to-noise
ratio (SNR) in reconstructed PET images. Singles count losses are typically more
significant than those of coincidences, due to the higher count-rates involved, and
can also include losses due to pulse pile-up.
Theoretically, dead-time losses fit into two basic models, termed paralyzable
and non-paralyzable. These models relate recorded counts (m) from PET detectors
to events (n) not exposed to dead-time, and have been well characterized [47]. The
two general dead-time models are given as:
m = n · exp (−nτ )
(1.6)
n
1 + nτ
(1.7)
m=
where τ is the characteristic dead-time coefficient and (1.6) and (1.7) are equations
for paralyzable and non-paralyzable dead-time models, respectively. In practice,
the dead-time experienced by detectors or acquisition electronics does not typically
fit these idealized models. To improve dead-time correction accuracy researches
have employed serial [48] and parallel [46] combinations of these ideal models with
varying levels of success.
17
1.5.4
Subject Motion
Both the effective spatial resolution and contrast are decreased as a function of
increased subject motion within the FOV. Measuring head motion in simulated
brain PET scans, Green et al. [49] showed that the effective spatial resolution
(σef f ) of a point source is modeled as:
σef f =
p
2 + σ2 )
(σres
mov
(1.8)
where σres is the reconstructed image resolution of the camera, and σmov is the
standard deviation of the point source motion over time. Lesions that are imaged
typically do not follow a Gaussian profile, so (1.8) acts as only a first order approximation. Motion artifacts are most significant in WB imaging for organs near
or in the thoracic cavity, due to the respiratory cycle [50]. For instance, using
respiratory gating Nehmeh et al. [51] demonstrated a decrease in lesion volume
ranging from 13.8% to 34.6% compared to static acquisitions. In this same study
the maximum standardized uptake value (SUVmax) increased as much as 160%
with gating.
In WB PET studies imaging the breast, positioning of the patient prone has
been found to significantly reduce respiratory motion artifacts [52]. Dynamic contrast enhanced MR has a longer history with imaging the patient in the prone position. Although prone positioning reduces respiratory motion, Hayton et al. [53]
demonstrated that non-rigid breast motion can occur by contraction of the pectoral muscle. In fact, non-rigid breast motion in contrast-enhanced MR requires
either light compression or deformable motion correction algorithms for accurate
data analysis [54].
18
1.6
Methods of Estimating Quantitative Performance for PET Scanners
1.6.1
Estimation of Image SNR as a Function of Count
Rates Using Noise Equivalent Counts Rates
Noise in reconstructed images influences the precision of quantitative measurements, e.g. SUVmax. In order to standardize scanner performance comparisons,
Strother et al. formulated a metric known as the noise equivalent count-rate
(NECR), that is a function of the signal-to-noise ratio (SNR) at the center of
a uniformly filled cylinder [55]. NECR is calculated using only the trues (T), scatter (S), and randoms (R) with LOR that pass though the cylinder, and is given
by:
N ECR =
T2
T + S + kR
(1.9)
where k is =2 assuming delayed randoms subtraction, and close to 1 for variance
reduced randoms subtraction. True events are defined as coincidences from a
pair of back-to-back photons that have not undergone scattering. NECR may be
thought of as the scaled trues giving the same SNR as an image subtracted for
randoms and scatters. Theoretically, NECR∝SNR2 . Using the 3D ordered subset
expectation maximization (OSEM) iterative reconstruction algorithm, Dahlbom
et al. validated this theoretical relationship for a wide range of activities [56].
The NECR model becomes less ideal when significant pile-up occurs, or error is
introduced through normalization and attenuation corrections [57, 58].
3D NECR depends significantly on the scanner geometry. For example Badawi
et al. performed simulations with a modified Zubal phantom and varied the de-
19
tector ring diameter and axial FOV [59]. The results show that for fixed activity
distribution and dead-time model, NECR decreases with larger diameters, but increases as function of the axial FOV. Clinical PET scanners may not follow these
conventions due to the significantly different acquisition electronics implemented.
For instance, current WB scanners with large patient ports and relatively small
axial FOV have peak NECR of 47 kcps (k = 2), where as a dedicated brain scanner
such as the ECAT HRRT, has a peak NECR=45 kcps [17, 60]. PEM and bPET
scanners have been suggested to have significantly lower NECR values. Zhang et
al., simulating a dual head PEM system with energy resolution of 24%, LLD of 450
keV, and coincidence window of 4 ns showed a peak NECR of 25 kcps for imaging
a simplified anthropomorphic phantom [61].
1.7
Clinical Motivation
In 2009 more than 254,000 women in the United States were expected to be diagnosed with breast cancer [5]. Of those diagnosed approximately 19% are expected
to die from the disease in 10 years [62]. The gold standard in the screening and
diagnosis of breast cancer has long been x-ray mammography. In fact, the significant reduction in annual breast cancer mortality in the last decade has been
attributed to improvements in both early detection, largely through x-ray mammography, and treatments. X-ray mammography, however, has been shown to
have significantly decreased sensitivity with increased breast density, as well as
limited ability in the differentiation of benign and malignant lesions [63, 64]. For
instance, it has been shown that 75% of lesions identified by mammography will
be diagnosed as benign after biopsy [6]. The superposition of fibroglandular tissue
20
with a suspicious lesion may explain the reduced detection rates in denser breasts.
Sonography is commonly used in an indeterminate diagnosis, but often with limited success [6]. To increase sensitivity and specificity in breast cancer detection,
researchers have been studying imaging modalities capable of assessing functional,
alone, or in addition to anatomical information. Functional information can include the degree of blood perfusion, metabolic activity, or even gene expression.
Examples of imaging modalities capable of providing functional information are
scintimammography, computed tomography, optical, magnetic resonance imaging
(MRI), and PET [65, 66]. In addition, the use of tomographic instead of planar
imaging may improve sensitivity for denser breasts.
1.8
WB PET and PET/CT in the Management
of Breast Cancer
1.8.1
18
Clinical Applications
F-FDG WB PET has clinical utility in breast cancer staging, restaging, and
therapy response monitoring. In primary systematic (neoadjuvant) chemotherapy
patients with stage II or III breast cancers are treated in an attempt to reduce
tumor volume and allow for the use of breast-conserving surgery [67]. The gold
standard for assessing the response of primary chemotherapy is histopathology
performed at the time of surgery. The absence of residual invasive tumor is defined as a pathologic complete response. As chemotherapy agents can have severe side effects it is important to identify nonresponders after as few courses of
chemotherapy as possible. Change in tumor size is clinically determined between
post-therapy and baseline scans with physical examination, ultrasound, and x-ray
21
mammography, however research suggests that metabolic changes in a tumor (as
determined through
18
F-FDG uptake) can be measured after significantly fewer
treatments than traditional imaging. A study by Rousseau et al. [68] found that
WB PET could identify tumors with pathological response after a single course
of neoadjuvant chemotherapy (sensitivity=61%, specificity=96%, negative predicitive value (NPV)=68%) whereas mammography had limited accuracy (sensitivity=31%, specificity=56%, NPV=45%) even after 6 courses of treatment. The
NPV, defined as the probability of not visualizing the diesease state when it is
absent, is an important metric for primary therapy response as it determines the
ability of a system to detect patients for which the current chemotherapy is not
effective. For staging WB PET has been shown to have a high accuracy for detecting distant metastasis. Mahner et al. [69] measured a sensitivity and specificity
for metastatic disease of 87% and 83%, respectively, for WB PET, versus 43%
and 98%, respectively, for combined results from chest radiography, abdominal
ultrasound, and bone scintigraphy.
Several experimental and clinical applications for the management of breast
cancer with 18 F-FDG WB PET rely on quantitative and semiquantitative metrics.
The measurement commonly employed is the standardized uptake value (SUV)
which is calculated from regions of interest (ROI) drawn on suspicious or known
lesions. Researchers have used the change in SUV between a baseline and posttreatment scan to monitor primary therapy response [70] and a fixed SUV threshold
[52] or a change in SUV between two scans performed after a single injection (dualtime-point WB PET) to detect suspicious lesions [71].
22
Few studies have examined the advantages of
18
F-FDG WB PET/CT in the
management of breast cancer [72–75]. In a retrospective study of 75 patients with
known breast cancer Tatsumi et al. [73] determined if PET/CT improved the
level of diagnostic confidence compared to PET or CT alone. Results showed
that PET/CT increased diagnostic confidence in 60% of patients compared to
PET alone, and significantly improved diagnostic accuracy for cancer detection for
PET/CT compared to CT alone (83% versus 68%). Radan et al. [74] explored the
role of PET/CT compared to contrast-enhanced CT in the assesment of suspected
recurrent breast cancer in a retrospective trial of 46 women. The study found that
combined PET/CT diagnostic sensitivity (85% vs 70%), specificity (76% vs 47%),
and accuracy (81% vs 59%) were all increased compared to results for contrastenhanced CT alone.
1.8.2
Limitations
Diagnostic sensitivity and quantitative accuracy is significantly reduced with WB
PET when imaging lesions that are small. In a study assessing the ability of static
18
F-FDG WB PET to detect lesions in 44 patients with suspected breast cancer
based on a fixed SUVmax threshold of ≥ 2.5, Imbriaco et al. [76] measured a
sensitivity of 75% for lesions >10 mm versus 31% for lesions <10 mm in diameter.
In a trial of 144 patients suspected of breast cancer Avril et al. [64] obtained
similar results, reporting a sensitivity of WB PET for lesions >20 mm of 92%
versus 68% for lesions ≤ 20 mm. This performance deficit has been attributed to
partial voluming, limited photon sensitivity, and attenuation from tissue outside
the breast [77]. For instance, LORs passing through the breast and the torso are
23
subject to as much as ∼ 6 half-value layers (HVL), where as those passing solely
through the diameter of the breast (average diameter=14 cm) undergo ∼ 2 HVL
[77], leading to significant count losses.
Several approaches have been used to increase the diagnostic sensitivity of WB
PET for breast cancer detection. Imaging the patient prone allows for several advantages over supine imaging, including the reduction of chest wall motion during
respiration, reduced attenuation from tissue outside of the breast, and improved
image fusion with bilateral MRI. In a study of 118 patients suspected of breast
cancer Kaida et al. [78] determined that sensitivity and NPV were significantly
improved for prone compared with supine static
18
F-FDG WB PET. Positioning
of the patient prone is done with specialized cushions or pads and has been performed routinely in several clinical trials. Although not restricted to WB PET,
dual-time-point 18 F-FDG imaging has been found to increase the sensitivity of WB
PET for lesions ≤1.0 cm. Researchers have noted that
18
F-FDG uptake increases
several hours after injection for malignancies, while benign or inflammatory tissue
seldom shows such prolonged uptake [71]. As opposed to an SUV threshold from
a static scan, a positive change in SUV between scans performed ∼ 60 and ∼ 100
minutes after
18
F-FDG injection signals a suspicious lesion. In a study examining
the ability of dual-time-point WB PET to detect breast cancer for women with
suspicious lesions, the diagnostic sensitivity of dual-time-point and static imaging
for < 1 cm lesions was estimated at 62% and 31% respectively [76]. Even with
the use of prone and dual-time-point imaging, however, the relative sensitivity of
18
F-FDG WB PET remains low for small lesions, compared to standard imaging
24
methods, and has limited clinical utility in the management of primary breast
cancer.
1.9
Dedicated Breast Positron Emission Imaging
Cameras with detector geometries specific to breast imaging that form reconstructed images from ACD measurements can be generally termed dedicated breast
positron emission imaging systems. The aim in designing these type of scanners is
to increase photon sensitivity and limit partial voluming effects, compared to breast
imaging with WB PET (see section 1.8), by utilizing detectors that are positioned
close to the breast and have significantly higher spatial resolution (lower magnitude) than measured with WB PET systems, respectively. The improvements
employed in dedicated cameras are expected to produce accompanying gains in
detection and quantification of smaller lesions. Furthermore, the increased photon sensitivity may allow for improved imaging performance at lower injection
activities than required for WB PET, thereby reducing the effective radiation dose
delivered to the patient. Potential dedicated breast positron emission imaging applications include local staging, surgical planning, assessment and monitoring of
therapy response, and detection of residual or recurrent disease.
Although there is currently no consensus in the field, we separate dedicated
breast positron emission imaging systems into two categories based on the completeness of angular sampling (φ) acquired in sinogram space. Breast PET (bPET)
cameras acquire fully tomographic scans while positron emission mammography
(PEM) units have limited angular sampling. We define fully tomographic acquisitions as those that meet or nearly meet Orlov’s conditions for a full set of
25
A
B
Figure 1.3. Examples of PEM scanner geometries. (a) Dual-head planar detector configuration resembling the geometry of the system in Turkington et al.
[1]. (b) Monolithic curved plates (partial ring) geometry resembling the system
in Freifelder et al. [2].
projections [79] for at least a single voxel in image space. The result of this difference in angular sampling is that for the same reconstruction method, images
from bPET scanners will exhibit more isotropic resolution than those from PEM
systems. Scanners that are classified as PEM or bPET systems often have unique
differences in detector geometry, hardware, and reconstruction methods. We explore these differences, as well as clinical trial results for PEM systems, in the
following sections.
1.9.1
Positron Emission Mammography
1.9.1.1
Hardware, Acquisition, and Reconstruction
PEM systems generally employ two detector heads and image the breast under
mild compression. Figure 1.3 shows two of the detector geometries employed in
PEM scanners. This class of systems largely resemble x-ray mammography units
in terms of physical footprint, detector geometry, and patient positioning. PEM
detectors typically employ pixellated crystal arrays read out by PS-PMTs and
are arranged in planar heads, although one design incorporates monolithic and
26
curved scintillators [80], and a separate scanner has a partial polygonal detector
geometry [4]. Several scanners have used detectors that can estimate the DOI using
multi-layer crystal elements [4, 81]. Table 1.1 compares the detector configuration
and geometry of several PEM scanners. As PEM systems often do not rotate to
acquire data it is more convenient to describe the FOV with respect to patient
planes, instead of in terms of transaxial and axial dimensions.
For acquisition each breast of the patient is scanned independently by PEM
detectors placed in any one or sequential combination of mediolateral, mediolateral oblique (MLO), and craniocaudal (CC) views, with scan time for each view
∼10 minutes. For imaging, the patient is typically positioned seated and upright,
although a more recent design [83] scans the subject in the prone orientation. The
limited number of projections typically acquired by PEM systems precludes the
use of filtered back projection (FBP) for image reconstruction (figure 1.4). Researchers have instead used both focal plane tomography and iterative methods.
When describing reconstruction methods it is helpful to define a coordinate system with respect to the PEM detectors, where in-plane refers to planes parallel to
and out-of-plane refers to planes perpendicular to the detector faces, respectively
(figure 1.4). In focal plane tomography counts for a given crystal pair are backprojected along the associated LOR and assigned to voxels in a set of 2D in-plane
images. This process is done for all LORs and the results summed to produce
the final image set. For LORs perpendicular to the in-plane all 2D images will
be equivalent, where as oblique LORs will pass through different voxels in the 2D
images based on their angle with respect to the in-plane. For focal plane tomogra-
2.00
18x18x2
PS-PMT
2x2 arrays (1 PMT)
2
5184 cuts
5.5
6.5
Crystal Pitch (mm)
Crystal Array
Photodetector(s)
Detectors/Head
Number Heads
Crystal Number
Anterior-posterior FOV (cm)
Coronal FOV (cm)
28.0
21.0
2
2
45 PMTs
single-channel PMT
NA
20.0
15.0
7260
2
6x8 PMTs
PS-PMT
50x66
3.30
3.00x3.00x10.0
thickness=19 mm
(solid curved plates)
1.85x1.85x6.5
Crystal Size (mm)
NA
LGSO
NaI(Tl)
BGO
Scintillator
Turkington et al. [1]
Freifelder et al. [80]
Thompson et al. [81]
Reference
6.0
16.4
2028
2
2x6
PS-PMT
13x13
NA
2.00x2.00x13.0
LYSO
Luo et al. [82]
Table 1.1. Description of detectors and geometry for several PEM systems.
21.6
10.5
98304
12
1x2
PS-PMT
32x32x4
1.45
1.44x1.44x4.5
LGSO
Furuta et al. [4]
27
28
A
C
B
out-of-plane
in-plane
r
Figure 1.4. Reconstruction of PEM emission data with filtered backprojection.
(A) Emission data acquired with PEM from a digital phantom. The in-plane
and out-of-plane directions are defined. (B) Representation of the coincidence
counts in sinogram space. (C) Estimation of the original source distribution
from FBP reconstructed images with significant blurring in the out-of-plane
direction visible.
phy the out-of-plane position of a given lesion corresponds to the in-plane image
slice where the cross-section of the lesion is smallest. For iterative reconstruction
methods PEM designs have used maximum-likelihood expectation maximization
(MLEM) [82] and the row action maximum likelihood (RAMLA) [2] algorithms.
Regardless of the reconstruction algorithm used, however, resolution in the outof-plane direction is significantly worse than for the in-plane (figure 1.4). Several
PEM systems have the ability to spatially register PEM and x-ray mammography
images into a fused image [81, 84], with the PEM voxel intensities often represented
as a false color scale on top of the linear gray scale of the x-ray mammography
intensities.
1.9.1.2
Clinical Trial Results
The performance of PEM systems during patient imaging has been assessed in
several clinical trials. Table 1.2 summarizes the results of these studies. The purpose of all but one [87] of these clinical trials has been to quantify the diagnostic
29
Table 1.2. Summary of clinical trial results for PEM imaging.
Reference
Patient
Number (n)
Sensitivity
(%)
Specificity
(%)
NPV
(%)
Murthy et al. [85]
14
80
100
67
Levine et al. [84]
16
86
91
91
Rosen et al. [86]
23
86
33
25
Tafra et al. [87]
44
NA
NA
NA
Berg et al. [88]
77
90
86
88
performance of PEM for imaging primary breast cancer in patients with known or
suspicious breast lesions. The study by Rosen et al. [86] measured a significantly
lower specificity and negative predicitve value compared to other PEM trials due
to its use of a patient population having a very high probability of breast cancer
(Breast Imaging Reporting and Data System assessment category 5 [89]), resulting
in few true and false negative cases. Patients were imaged by PEM after injection
of 2-21 mCi of
18
F-FDG and images read by reviewers who had access to results
from x-ray mammography and clinical examination. PEM and x-ray mammography images were reviewed side-by-side [86–88] alone or in combination with fused
results [85, 86]. Both quantitative and semi-quantitative metrics were employed
in these studies, including: SUVs and the difference in normalized counts between
the ipsilateral and contralateral breasts [85]. Sensitivity, specificity, and negative
predictive value (NPV) were found to range from 86-90%, 33-100%, and 25-88%,
respectively. The design of the study by Tafra et al. prevented the calculation of
diagnostic performance values.
The ability of PEM to image cancer was significantly influenced by lesion size,
30
location, and type. Benign lesions types typically classified as false-positives on
PEM included fatty necroses [86, 88] and fibroadenomas [88], while cancerous
tumor types deemed false-negatives varied greatly, but included invasive lobular
carcinoma (ILC) [84, 88], invasive tubular carcinoma [87, 88], invasive ductal carcinoma (IDC) [86, 87], and DCIS [86, 88]. False-negative invasive cancers were
often found to be low or intermediate grade on histology. Lesions positioned close
to the chest wall were missed in several studies [86, 88] and one trial [85] purposely
excluded lesions located too posteriorly to be in the PEM FOV. The dead-space
between the active area of the detectors and casing in combination with the acquisition geometry are reasons cited for the limited chest wall and axillary tail
coverage of current PEM systems.
The results suggest that PEM has significantly higher sensitivity for in situ
lesions and those <1 cm in size than WB PET, although no direct comparison
has been reported. A study by Berg et al. [88] was able to detect 5 of 8 (63%)
invasive cancers <1 cm with PEM and 10 of 11 (91%) DCIS lesions. Tafra et
al. [87] noted the detection of a 4 mm DCIS on PEM that was occult on x-ray
mammography. In comparison, using single-time-point WB PET a sensitivity of
31% was measured for lesions <1 cm in diameter [76]. Although the sensitivity of
PEM for detecting lesions is not expected to be significantly influenced by breast
density as compared to x-ray mammography, studies with
18
F-FDG WB PET
have shown that background uptake is correlated with the ratio of fibroglandular
to adipose tissue [88]. In a clinical trial with PEM the highest mean glandular
SUV was measured at <1.4 [88]. As the SUV threshold (2.5) typically employed
31
B
A
Figure 1.5. Examples of bPET scanner geometries. (a) Four-head planar detector configuration resembling the geometry of the system in Raylman et al. [3].
(b) Polygonal detector configuration resembling the geometry of the system in
Furuta et al. [4].
in differentiating between benign and malignant lesions is signficantly greater than
the maximum recorded glandular uptake, the researchers suggested that breast
density should not influence the performance of PEM in cancer detection [88].
1.9.2
Breast Positron Emission Tomography
1.9.2.1
Hardware, Acquisition, and Reconstruction
In contrast to PEM cameras, bPET scanners have been developed with a range of
detector geometries. Figure 1.5 shows two detector geometries employed in bPET
systems. Detectors employed are similar to those used in PEM systems although
longer crystal elements are generally used in bPET cameras with single-ended
readout detectors. Geometries have included cameras with a rectangular [18, 90]
and polygonal [4, 91] arrangement of detector heads around the CFOV. To acquire
full angular sampling for systems with large inter-detector gaps the gantries of two
scanners allow for rotation in the transaxial FOV [90, 91]. Table 1.3 compares the
32
detector configuration and geometry of several bPET scanners.
For bPET acquisition the patient is typically positioned prone on a specialized
bed, with a single breast hanging pendant through a hole in the table top. In
contrast to PEM systems no immobilization of the patient’s breast is expected to
be required for bPET imaging. As nearly fully angular sampling is acquired for
bPET systems the same reconstruction methods used in WB PET imaging can
be employed. Iterative reconstruction methods have been typically chosen over
FBP due to improved SNR at low counts and reduced artifacts with rectangular
geometries. There have been no patient trials, before the work present in this
dissertation, assessing bPET systems in the detection of breast cancer.
1.10
Current Project
1.10.1
Aim
Our group has constructed a combined and dedicated breast PET/CT scanner.
The goal of this research is to characterize and correct for the factors influencing
image quantification in the PET portion of the system, and explore methods to
improve quantification with alternative bPET system designs.
1.10.2
Outline of Dissertation
The content of this dissertation is separated into seven chapters. In Chapter 1
we have presented background material fundamental to the research presented in
later chapters. Chapter 2 presents a description of the dedicated breast PET/CT
scanner focusing on components implemented by the author. Chapter 3 explores
performance measurements for the PET component that are not related to data
corrections methods. In Chapter 4 the radiological interpretation and system per-
PS-PMT
4x3 PS-PMTs
7x7
single-channel PMT
10x6 arrays
(7x11 PMTs)
NA
8x8
Front: 8x8 PIN PD array
Back: single-channel PMT
3x2
4
rectangle
1536
8.2x6.0
5.0
static
Crystal Pitch (mm)
Crystal Array
Photodetector(s)
Detectors/Head
Number Heads
Head Arrangement
Crystal Number
Transaxial FOV (cm)
Axial FOV (cm)
Acquisition Motion
rotational
21.0
54.0
38016
polygon
12
2.70
2.68x2.68x18.0
3.00x3.00x30.0
Crystal Size (mm)
rotational
15.0
15.0
27648
rectangle
4
96x72
2.10
2.00x2.00x15.0
LYSO
BGO
LSO
Scintillator
Raylman et al. [90]
Li et al. [91]
Wang et al. [18]
Reference
static
15.6
18.3
147456
polygon
12
1x3
PS-PMT
32x32x4
1.45
1.44x1.44x4.5
LGSO
Furuta et al. [4]
Table 1.3. Description of detectors and geometry for several bPET systems.
rotational
18.0
16.0
6144
planar
2
8x12
Front: 4x3 element APD
Back: 4x3 element APD
4x3
2.30
2.00x2.00x20.0
LYSO:Ce
Abreu et al. [83]
33
34
formance of a proof-of-principle patient trial with the dedicated PET/CT scanner
are covered. Chapter 5 presents the validation and performance of data correction schemes implemented to produce quantitative bPET images. In Chapter 6
Monte Carlo (MC) simulations are used to determine the performance of alternative bPET detector geometries. Chapter 7 discusses future research studies for the
dedicated breast PET/CT system.
35
Chapter 2
Dedicated Breast PET/CT
Instrumentation
2.1
Introduction
The UC Davis dedicated breast scanner, herein referred to as DbPET/CT, consists
of a dual-head bPET camera and multi-detector row x-ray dedicated breast CT
(bCT) integrated into a single gantry. The bCT is a second generation system,
nicknamed Bodega, and was developed exclusively by Boone et al. [92]. Construction of the PET component was initiated by Doshi et al. [93]. The implementation
of data correction methods for the PET component requires the addition of several
software and hardware components, including: the ability to simultaneously collect prompts and delayed coincidences and estimate system dead-time. In addition,
system improvements are needed for the safe and reliable imaging of patients by
the combined scanner. The following chapter outlines the complete DbPET/CT
system with emphasis on the components developed for the research discussed in
this dissertation.
36
A
CT detector
PET detectors
X-ray tube
S
A
C
B
Figure 2.1. (A) Schematic depicting DbPET/CT. The object between the PET
detectors shows the approximate position of a subject’s breast during scanning.
Orientation of the positioned patient’s coronal (C), sagittal (S), and axial plane
are depicted in the bottom right hand corner. (B) The PET gantry allows for
control of detector height (vertical arrow), separation distance (horizontal line
with end markers), and rotation (curved arrow).
2.2
Combined System Overview
A schematic of DbPET/CT is shown in figure 2.1A. For imaging, the subject is
positioned prone with a single pendant breast hanging into the scanner’s field
of view (FOV). In contrast to WB PET/CT the DbPET/CT transaxial FOV is
parallel and the axial FOV perpendicular to the coronal plane (see figure 2.1A).
37
Table 2.1. CT System Characteristics
Component
X-ray tube
Detector
Characteristic
Focal spot:
Water cooled W anode, beryllium window
0.4 x 0.4 mm
0.3 mm Cu added filtration
1000 Watts (i.e. max mA at 80 kVp=12.5 mA)
Material: indirect detection (CsI scintillator) thin film transistor
Active area: 40 x 30 cm
Native pixel matrix: 2048 x 1536
Native pixel size: 0.194 x 0.194 mm
2 x 2 pixel binned matrix: 1024 x 768
Frame rate: 30 frames per second at 2 x 2 binning
Data are adapted from [96]
2.3
2.3.1
CT System
Hardware
The CT component is composed of a CsI flat panel detector (PaxScan 4030CB,
Varian Medical Systems, Palo Alto, CA), a tungsten target x-ray tube (Comet
AG) and a custom made rotational gantry (see figure 2.1A). Characteristics of
the system are given in table 2.1. Performance results of an earlier breast CT
prototype with similar characteristics [94], as well as results from a patient trial
[95] have been reported.
2.3.2
Acquisition and Reconstruction
The CT system acquires a total of 500 projections taken over 16.6 seconds with a
continuous rotation over 360 degrees. Tube current is adjusted to deliver the same
dose as 2-view mammography (range for patient imaging= 2.5-7.3 mA), based on
the percent glandularity and size of a given breast [97], while tube voltage is fixed
38
Table 2.2. PET System Characteristics
Parameter
Value
Crystal size (mm)
3 x 3 x 20
Crystals array
81 (9 x 9)
Crystal pitch (mm)
3.3
No. of detector blocks
16 (4 x 4)
FOV (cm)
11.9 (axial + transaxial)
Lines or response
12962
at 80 kVp.
CT data are reconstructed with the Feldkamp [98] algorithm and normalized to
Hounsfield units (HU). An image volume is composed of a number (N) of coronal
images with a voxel matrix of 512 x 512 x N, with N set to contain a given
breast length. For patient imaging the voxel dimensions range from 0.2-0.4 mm
transaxially, and 0.2-0.3 mm axially.
2.4
2.4.1
PET System
Hardware
The PET component utilizes lutetium oxyorthosilicate (LSO) based detector modules arranged into two square flat panel heads. Table 2.2 summarizes the key parameters of the camera. Each single-ended readout detector module is composed
of a crystal array coupled to a position-sensitive photomultiplier tube (R5900-C8,
Hamamatsu Photonics K.K., Japan) via an optical fiber bundle [93]. As the active
area of the PS-PMT is less than its physical envelope, the optical fiber bundle increases inter-detector packing fraction significantly compared to directly coupling
the crystal array to the PS-PMT.
39
Singles NIM
Detector
Head 1
Pre-Amp
Signals
x4
CFD
S1c
Coincidence
Logic
Logic Unit
Generate τ =6 ns
PC
Coincidence
Logic
32 ns Delay
Detector
Head 2
Pre-Amp
Signals
x4
CFD
Rc
Randoms
DAQ
S2c
Logic Unit
Generate τ =6 ns
Pc
Prompts
DAQ
Figure 2.2. Schematic of PET electronics used for prompts and randoms data
acquisition (DAQ) trigger generation. For a full description see section 2.4.1.
Electronics are able to simultaneously acquire both prompts and delayed coincidences. A schematic of the electronics largely involved in trigger generation is
shown in figure 2.2. Starting from the top left, the pre-amp signals from PS-PMT
detectors are multiplexed with a resistive network down to a total of 4 signals for
each detector head. The 4 pre-amp signals are summed with a quad linear fanin/fan-out module (428F, LeCroy, Chestnut Ridge, NY) and fed into a constant
fraction discriminator (CFD). Singles triggers (τ =6 ns) are generated for both
heads and run through coincidence logic with no offset for prompts trigger generation using four input majority logic units (754, Phillips Scientific, Mahwah, NJ).
For delayed coincidence trigger generation the singles triggers from one head are delayed by 32 ns before coincidence logic. NIM triggers are converted to TTL pulses
via a quad gate/delay generator (794, Phillips Scientific, Mahwah, NJ) and fed to
separate data acquisition (DAQ) boards (PD2-MFS-2M/14, United Electronic Industries, Inc., Walpole, MA) for prompts and delayed coincidence acquisition. The
40
PD2-MFS-2M/14 boards have been well characterized by Judenhofer et al. [99] for
γ ray detection and are capable of sampling data with high linearity (∼99%) and at
reasonable dead-time at expected coincidence rates (50% event loss at 230 kHz).
Before digitization coincidences are integrated with a custom fast spectroscopy
amplifier using CR-RC shaping with time constant of 80 ns [100] and split with an
octal linear fan-in/fan-out module (748, Phillips Scientific, Mahwah, NJ) to allows
for simultaneous prompts and delayed coincidence acquisition for each channel.
The complete data acquisition is controlled with a personal computer (PC). For
dead-time estimation and correction and to optimize DAQ parameters as a function of coincidence rates (see section 2.4.2) computer controlled dual-counter and
timer modules (994, Ortec, Oak Ridge, TN) are used to estimate rates of singles
for both heads (S c ), prompts (P c ) and delayed coincidences (Rc ). The counter
modules are controlled via RS-232 connections with the host PC and estimate the
average rates for each step in an acquisition.
PET heads are mounted on a custom built gantry that allows three degrees of
freedom and shielding (see figure 2.1B). Detector rotation around the center FOV,
separation distance, and height are all adjusted by individual computer controlled
drives. Photon sensitivity can be maximized for a given breast by minimizing detector separation distance. The detector height adjustment allows for the distance
between the top of the PET heads and patient chest wall to be minimized while
still allowing space for rotational clearance. To aid in patient positioning a handcontroller allows independent control of all drives. For shielding from x-rays 3 mm
thick lead plates cover the front of PET heads during CT scanning and line 4 sides
41
(excluding the back and front) of each PET head. The total distance between
the crystal arrays and top of the PET head is 0.9 cm. In addition, in order to
prevent irradiation of the PET detectors by the x-ray tube, a simple logic circuit
was produced to communicate to the CT system when the PET detectors are fully
homed and behind protective lead shielding.
2.4.2
Software
The in-house produced acquisition software was programmed in Lab Windows/CVI
(National Instruments, Austin, TX) and is designed for both phantom experiments
and patient scans. The software was modified from an existing application developed by Judenhofer et al. [99]. For the sake of extended normalization or deadtime scans, the software permits automatic acquisition at specified time points and
durations. Position of the detector heads can be fully controlled and monitored
through the interface, which is particularly important for patient scans. Furthermore, signal lights indicate that the PET system is indeed homed before a CT scan
begins. For archival, reconstruction, and data correction purposes, raw list-mode
data can be generated with Interfile format headers [101]. A list-mode file is generated for each angle, in the step-and-shoot acquisition, and these data files contain
binary headers which record acquisition times, count rates, and gantry positioning
information. Figures 2.3 and 2.4 show examples of the PET acquisition interface
GUI.
The acquisition software was modified to simultaneously acquire both prompts
and delayed coincidences via the use of multiple write threads. The previous software implementation allowed for synchronous acquisition with two DAQ boards,
42
Figure 2.3. Main GUI of the control and acquisition software for the PET
component of DbPET/CT.
however, as the rates of prompts and delayed coincidences typically vary significantly, the ability of the program to acquire data asynchronously was required.
Figure 2.5 depicts a schematic of the functions and pseudocode used in simultaneous acquisition. Data is transfered from the DAQ first in, first out (FIFO) memory
to circular buffers, located in virtual memory on the acquisition PC, independently
43
Figure 2.4. GUI for the PET component of DbPET/CT allowing for the specification of acquisitions of desired durations and at specific time points (left)
and the entrance of patient information for Interfile format output.
for the two acquisition boards. Data is written at the head end pointer and read
from the tail end pointer of the circular buffer, respectively. A frame of data is
defined as the amount of samples between two frame markers. When the head
of the data reaches a frame marker an event is handled by the AInEventProcessing() function and at the most all data frames in a circular buffer are transfered
to thread safe queues. Simultaneously, separate threads of the ThreadFileWriteMult() function write data samples half a frame at a time (ScanSize) to files on on
the hard drive until the acquisition is finished. Prompts and delayed coincidences
are written to separate binary data files. Acquisition is finished when a specified
number of samples is reached (n) or the specified acquisition time expires. A single
internal timer is maintained to determine if the specified acquisition time has been
reached, and if so, acquisition with the DAQ is terminated. As event processing for
44
DAQ
Prompts
Randoms
Acquisition PC
Circular Buffers
Head
Frame Marker
Thread Safe Queue
AInEventProcessing( )
ThreadFileWriteMult( )
if (time over) {
acquisition is done}
if (# samples > 0){
write ScanSize0 samples
}else
{repeat or break if acquisition is
done }
Thread Safe Queue
if (time over) {
acquisition is done}
if (# samples > 0){
write ScanSize1 samples
}else
{repeat or break if acquisition is
done }
Output File 1
Output File 0
ScanSize0
ScanSize0
0
n
ScanSize1
ScanSize1
0
n
Figure 2.5. Schematic of PET acquisition software used for the simultaneous collection of both prompts and delayed coincidences. Dotted boxes denote distinct
threads. Grey color in buffer denotes data that has not been read. Functions
involved in a process are denoted with closed parenthesis at the end.
the DAQ are controlled by independent threads the actual amount of acquisition
time has been found to vary from the user specified time and between the boards
themselves. If the head passes the tail pointer in the circular buffer an overflow
error occurs and the acquisition terminates. Conversely, if the head pointer fails to
pass a frame marker during an acquisition than no data is recorded. The number
of frames and size of the frames can be adjusted based on count rate to avoid both
scenarios using the computer controlled counters discussed in figure 2.2.
45
2.4.3
Acquisition and Reconstruction
PET heads are positioned then rotated in step-and-shoot motion (40 steps) over
180◦ . Acquisition time for the PET is user defined, but is typically 10 minutes
per a breast.
Raw voltage measurements from the 4 channels of each detector head for a
coincidence event are converted to a crystal identification number (ID) and energy
in post-processing. The first step in this process is to calculate the X-Y position
of a coincidence event in detector heads 0 and 1 using Anger logic as follows:
X0 =
V0 + B0
(V0 + B0 ) + (V1 + B1 )
(2.1)
Y0 =
V3 + B3
(V2 + B2 ) + (V3 + B3 )
(2.2)
X1 =
V4 + B4
(V4 + B4 ) + (V5 + B5 )
(2.3)
Y1 =
V7 + B7
(V6 + B6 ) + (V7 + B7 )
(2.4)
where V0 -V3 and V4 -V7 are the digitized voltage measurements recorded from the
spectroscopy amplifier, and B0 -B3 and B4 -B7 the baseline corrections for detector
heads 0 and 1, respectively. The baseline corrections are required due to baseline
wandering likely stemming from the DC-coupled octal linear fan-in/fan-out NIM
module (see section 2.4.1). The analog position measurements are converted to
discrete positions (P 0 ) on a 512 x 512 image matrix as follows
P 0 = int (P (N umP ixels − 1) + 0.5)
(2.5)
where P is the analog position (X0 ,X1 , etc.), N umP ixels is the number of pixels of
one dimension of the square matrix, and the int operator rounds the analog value
46
to the nearest integer. Baseline correction factors are estimated automatically
by determinining the voltage at the position of maximum change for a voltage
histogram of all events on a channel by channel basis. Baseline correction factors
are then manually refined by visually inspecting the alignment of peaks in a flood
histogram with the crystal lookup table (LUT).
Calculation of the crystal ID number is performed by matching the discrete
flood position (P 0 ) with a known crystal through a crystal LUT. Generation of
the crystal lookup table itself is performed from a high count singles flood using
the methods of Chaudhari et al. [102]. After the crystal ID number is known,
coincidence data are passed through a 350-650 keV energy window. The energy
window values are calculated on a crystal-by-crystal basis from a high count singles
acquisition through a method which involves: 1) estimating the channel number
of the 511 keV photopeak position, 2) scaling the photopeak position to determine
the lower level (LLD) and upper level discriminator (ULD) values (assuming that
digitized channel number varies linearly with absorbed photon energy). Information for each coincidence event is then written to list-mode format, where each
entry records the crystal position in order of head 0 and head 1, each in 16 bits.
Data are reconstructed with a fully 3D maximum a posteriori (MAP)[103] based
algorithm into an image of 108 x 108 x 36 voxels of dimension 1.1 x 1.1 x 3.3 mm
(transaxial sampling = 1.1 mm). The MAP reconstruction uses a sparse system
matrix that accounts for crystal solid angle and attenuation length and uses symmetries in the system geometry to further reduce memory requirements. Geometric
efficiency variations caused by gaps between the crystals are not accounted for in
47
B
A
Figure 2.6. Breast positioning system used in DbPET/CT.(A) Photo showing
the components of the positioning system, including the clear polycarbonate
cylinder and the black central support base with aluminum connector rod. (B)
Display of how ports are accessed by a technician to more accurately center the
patient’s breast in the FOV.
the current implementation.
2.5
Patient Bed and Positioning Aids
Placement of the patient’s breast in the scanner FOV is handled by the patient
bed and breast positioning system. With the custom bed, a sloped steel table top
allows the patient to comfortably bend at the hips, while a carbon fiber support
and Naugahyde cover (Uniroyal Engineered Products LLC, Stoughton, WI) surrounding the aperture in the table top, permit the patient to sink under her own
weight. The combination of these elements allows the anterior aspect of the patient to be positioned significantly farther into the top of the scanner’s axial FOV
than if a flat and rigid table were used. As the transaxial PET FOV (11.9 cm) is
less than the average breast diameter (14.0 cm) [104] a breast positioning system
(composed of a clear polycarbonate cylinder with ports for technician access) is
used to center the patient’s breast (figure 2.6).
48
Chapter 3
Basic Performance Measurements
3.1
Introduction
Although standards exist for estimating quantitative accuracy during patient imaging with WB PET, no standard is currently available for bPET or PEM. Custom
performance tests, specific to the scanning and patient geometries employed in
dedicated positron emission scanners, have been examined. Researchers estimated
the influence of activity from outside the field of view (FOV) on contrast recovery
for PEM [105] or lesion visibility with bPET [2] using an anthropomorphic torso
phantom, uniformity and noise at the edge of the in-plane FOV with line source
measurements for PEM [82] and contrast recovery as a function of cross-plane
position using spheres in a compressible saline bag for PEM [82]. The NEMA
standards have been adapted for measuring breast positron emission imaging performance. Luo et al. [106] used the NU 4-2008 small animal PET standard [107]
directly for a PEM system, while the method for estimating noise equivalent count
rates (NECR) and the scatter fraction in the NU 2-2001 [108] guideline was modified for use with a bPET scanner [3]. We aim to characterize the performance of
49
DbPET/CT, largely in the absence of data corrections, using custom phantoms
and methods. We calculate the MAP based spatial resolution, NECR values for
an ideal and patient imaging scenario, coincidence photon detection sensitivity,
accuracy of the spatial registration between the PET and CT components, and
influence of the PET component on CT performance. This work was detailed by
Wu et al. [100].
3.2
3.2.1
Materials and methods
Spatial Resolution for MAP Reconstruction
For purposes of comparison WB PET standards (NU 2-2001)[108] advise estimating spatial resolution from images of a line source in air reconstructed with
FBP after single-slice rebinning (SSRB). Spatial resolution was estimated from
MAP in addition to FBP reconstructed images, as MAP is expected to be the
primary reconstruction algorithm for patient imaging with DbPET/CT. A fillable
right cylinder phantom (outer diameter=4.4 cm) with a centrally placed glass line
source (outer diameter=0.8 mm) was filled with a total of 430 µCi of
18
F-FDG,
at the start of imaging, with the concentration ratio between the line source and
fillable cylinder ≈400:1. As MAP implementations contain a non-negativity constraint, use of a line source in air can bias resolution estimates artificially high
(lower magnitude) [109]. Resolution bias is prevented by using the line source in
a warm background phantom employed in this study.
The phantom was arranged with the long axis either parallel or perpendicular
to the rotational axis of the scanner and imaged with tomographic acquisitions
for a total of 400 seconds by DbPET/CT (head separation=20.0 cm) at several
50
radial and axial offsets for each orientation. Raw data was converted to list-mode
using an energy window of 350-650 keV and reconstructed with MAP for a total of 15 iterations using a hyperparameter of the Gibbs prior (β) set to 10−08 .
Resolution was estimated according to the NU 2-2001 standard [108] from images
reconstructed with voxel sizes of 1.13x1.13x3.40 mm for transverse measurements
and voxel sizes of 3.40x3.40x0.56 mm for axial measurements. Briefly, line profiles
were measured using MATLAB
®(The MathWorks, Inc., Natick, MA), the back-
ground subtracted, and the maximum pixel intensity analytically determined from
a fit of a parabola to the three highest intensity points. The full-width at half
maximum (FWHM) and full-width at tenth maximum (FWTM) were estimated
by interpolating between the data points immediately surrounding 50% and 10%
of the maximum intensity value on either side. Different voxel sizes for the reconstructed images were chosen to maximize spatial sampling in the measurement
dimensions.
3.2.2
Noise Equivalent Count Rates for a Cylinder Phantom
Optimal noise equivalent count-rates (NECR) were estimated by scanning a cylinder phantom without the presence of OFOV activity. The right cylinder phantom
(outer diameter=7.5 cm, height=11.1 cm) was filled with 0.8 mCi at the start
of imaging, placed at the CFOV, and scanned with tomographic acquisitions by
DbPET/CT (scan time=30 seconds per a step, detector separation=20.6 cm) for
a total of ∼12 half lives. Prompts and randoms data was converted to list-mode
using a 350-650 keV energy window.
51
An important step in estimating the true count rate (T ) for use in the NECR
metric, is the calculation of the scatter fraction (SF ). Using the NEMA NU 22001 standard [108] SF is calculated from sinograms acquired from a line source
positioned off center in a solid right circular cylinder. Ideally, the offset of the line
source phantom should produce the same SF as a uniformly filled cylinder with dimensions equal to the solid phantom. As the dimensions of the NEMA NU 2-2001
solid cylinder phantom (diameter=20 cm, length=70 cm) are not representative
of average breast sizes, and a cylinder phantom with correct line source offset for
breast positron emission imaging SF estimation had not been developed, we chose
to estimate SF via a Monte Carlo (MC) simulation using GATE [110]. We did not
account for scatter from OFOV as this has been shown to have a negligible influence
on the total scatter fraction for bPET systems [38]. The phantom was modeled as
an analytic plastic right cylinder (outer diameter=7.2 cm, inner diameter=6.9 cm)
with a water center for the attenuation map, and a right cylinder with dimensions
of the water center representing the activity map. The activity distribution was
assumed uniformly distributed. The simulation geometry described in section 6.2
was used to model DbPET/CT, but with a simplified electronics chain that assumed an energy resolution of 25% at 511 keV, energy windowing of 350-650 keV,
and no losses due to dead-time or pile-up. A total of 475,000 energy thresholded
trues+scatters (S) were acquired from a simulation of the cylinder phantom at a
single projection angle and the SF calculated as follows:
SF =
X
ij
mij Sij
Tij + mij Sij
(3.1)
where counts are summed for crystal pairs defined by the LOR between crystals
52
i and j, and mij is a binary histogram mask defining the interior of the cylinder
phantom such that only scatters with LORs that pass through the phantom are
included in the calculation of SF . To generate mij for the simulation geometry a
voxelized representation of the analytic cylinder phantom was created and forward
projected into sinogram space using the Siddon algorithm [111]. As the cylindrical
phantom was positioned at the center of the FOV the scatter fraction for each
projection angle is constant and = SF .
Using the experimental prompts (pijθ ), randoms (rijθ ) for a given acquisition,
and the SF estimate, NECR rates were calculated as follows:
X
(pijθ − fθ rijθ ) meijθ
(3.2)
X
rijθ meijθ
(3.3)
pijθ meijθ
(3.4)
P
( θ Tθ )2
P
NECR = P
θ Pθ + (k − 1)
θ Rθ
(3.5)
Tθ = (1 − SF )
ij
Rθ = fθ
ij
Pθ =
X
ij
1
∆t
where Tθ , Rθ , and Pθ are the integrated counts per a projection step (θ) for trues,
randoms, and prompts, respectively, fθ adjust the randoms to have the same deadtime as the prompts data (see section 5.2.1.4), ∆t is the acquisition time, and meijθ
is the histogram mask for the experimental data. For direct or variance reduced
randoms subtraction k was set to 2, or 1, respectively. NECR was calculated for
all acquisitions and the phantom activity for a given acquisition was determined
as in [108].
53
Figure 3.1. Complete anthropomorphic breast phantom used to estimate NECR
values during patient imaging. Volumes representing the brain and bladder are
not shown. In the final configuration the breast compartment was not taped to
the torso.
3.2.3
Noise Equivalent Count Rates for an Anthropomorphic Phantom
NECR values during patient imaging and as a function of injection activity were
estimated with an anthropomorphic phantom. The full phantom consisted of an
anthropomorphic torso phantom (Radiology Support Devices Inc., Long Beach,
CA.)[112] composed of tissue-equivalent material with compartments representing
the lungs, liver, and thoracic cavity, a fillable right cylinder for modeling the prone
breast (see section 3.2.2), and fillable volumes representing the brain (volume=600
mL) and bladder (volume=550 mL). The complete phantom, excluding the brain
and bladder volumes, is shown in figure 3.1. The compartments were filled with
a total of 5.4 mCi
18
F-FDG, at the start of imaging with concentration ratios
54
Figure 3.2. Extended WB PET patient images (maximum intensity projection)
used to estimate injection activity from anthropomorphic phantom activity.
The outline around the head and torso approximates the region modeled by the
anthropomorphic phantom.
for the breast:torso:liver:lung:brain:bladder set to 1:2:5:0:10:20, respectively. Concentration ratios represented the average SUVs from a total of 17 female patient
scans. For acquisition the RSD torso phantom was positioned lengthwise on top
of the scanner gantry, with the brain and bladder compartments placed cranial
and caudal to the torso phantom, respectively. For ease in positioning, the breast
phantom was placed on the support column at the center of the FOV (CFOV).
Tomographic acquisitions (detector separation=20.6 cm) were acquired over a total of ∼13 half-lives with scan time doubled ∼ every half-life to improve counting
statistics at lower activities. Experimental prompts and randoms, in combination
with a MC estimated SF , were used to calculate NECR as in section 3.2.2. For
the MC based scatter fraction estimation the source and attenuation distributions
for the RSD torso phantom, bladder, and brain volumes were not included.
Conversion of the activity in the full anthropomorphic phantom (Ap ) to an
estimate of the injection activity (Ai ) was performed via extended WB PET scans.
Images from a total of two female
18
F-FDG WB PET studies were analyzed for
which the axial FOV included the full length of each patient. Figure 3.2 shows
55
a maximum intensity projection for one of the extended WB PET images. Total
activity in a typical patient was calculated by scaling the total phantom activity
by the average ratio (W ) of the sum of voxels for the complete patient PET images
to those in the head, torso, and bladder. For the two WB PET patient data sets
W = 1.39. Total injection activity (Ai ) was estimated as follows:
Ai = Ap · W exp(−λ ∗ 60)1.25
where λ is the decay constant for
18
(3.6)
F, an hour of uptake time is assumed, and
the factor of 1.25 accounts for 20% excretion during uptake. More recent studies,
however, have measured the % injected dose (%ID) excreted at 7-8% after 60
minutes [113].
3.2.4
Coincidence Photon Detection Sensitivity
The probability of recording a coincidence from a positron annihilation is defined as
the coincidence photon detection sensitivity (abbreviated as photon sensitivity).
Photon sensitivity depends on the solid angle of the detectors and the energy
windowing employed and should be estimated from acquisitions with negligible
count losses from dead-time, attenuation, and pile-up, and at low randoms and
scatters rates. We employed a method based on [18] for the estimation presented
here.
Photon sensitivity was estimated by translating a
68
Ge point source (activ-
ity=20 µCi, active diameter≈ 1 mm) across the complete axial FOV in 5 mm
increments using computer controlled stepping motors. A total of two stages were
used, with the travel of one stage arranged parallel to the rotational axis of the
scanner and other positioned parallel to the transaxial plane and the detector faces.
56
The stage with travel in the transaxial plane was used to accurately position the
point source at the transaxial CFOV. Static acquisition were used, with scan time
per a source position set to 5 minutes and detector separation =20.6 cm (crystal
face-to-face). To account for the background from 176 Lu, singles were acquired with
no source in the FOV for a total of 185 minutes. Data was converted to list-mode
with a 350-650 keV energy window and prompts rates computed. Sensitivity as a
function of the detector height (s(h)) was calculated as follows:
s (h) =
P (h) − R (h) − BLSO
Ac
(3.7)
where P (h) is the prompts, R(h) the randoms, and BLSO the correlated LSO
background in the prompts window rate.
3.2.5
Registration Accuracy
An important component for multimodality imaging systems is the ability to accurately spatially register images from the separate scanners into a single reference
frame. Differences in the observed FOV, spatial sampling, and orientation between
the imaging systems necessitates registration for ease in fused image interpretation, quantitative corrections, or computer aided detection. We have used an affine
transform to register reconstructed PET volumes to the CT and vice versa. The
affine transform is defined as a set of linear transforms and a translation which
maintains the ratio of distances and the collinearity between points. Possible linear
transforms include rotation, scaling, and shearing (defined as the preservation of
parallel planes, but the movement of the planes with respect to each other). For
DbPET/CT only a subset of these transforms were found to be important, and the
complete registration of the CT to the PET reference frame in <3 was described
57
generally as:
x0 CT = RSxCT + t
(3.8)
where xCT and x0 CT are vectors of x,y, and z coordinates with respect to the
CT and PET reference frames, respectively, R the rotation matrix, S the scaling
matrix, and t the translation vector. Both the rotation and translation matrices
are defined using the conventions of the registration software, RView [114], with
R set as follows:
cos(−θy ) cos(−θz )
R = sin(θx ) sin(−θy ) cos(−θz )−cos(θx ) sin(−θz )
cos(θx ) sin(−θy ) cos(−θz )+sin(θx ) sin(−θz )
cos(−θy ) sin(−θz )
− sin(−θy )
sin(θx ) sin(−θy ) sin(−θz )+cos(θx ) cos(−θz )
(3.9)
sin(θx ) cos(−θy )
cos(θx ) sin(−θy ) sin(−θz )−sin(θx ) cos(−θz )
cos(θx ) cos(−θy )
where θx , θy , and θz are the angles of rotation around the x, y, and z axis, respectively. Components for scaling (S) and translation (t) were defined as follows:
sx 0 0
S = 0 sy 0
0 0 sz
tx
t = −ty
−tz + tCT
(3.10)
(3.11)
where sx , sy , and sz in (3.10) are scaling values and tx , ty , and tz in (3.11) translation values for the x, y, and z axis, respectively. For DbPET/CT an isotropic
scaling was assumed such that sx = sy = sz . In (3.11) tCT adjusts for the z offset
between centers of the CT images used for registration parameter estimation and
58
a given acquisition. To reduce memory consumption the number of coronal image
slices was set to the minimum required to fully contain a given breast, leading to
the variation in CT image centers. For implementation the algorithm was coded in
C using the GNU libraries. As a transformed coordinate, x0 CT for the case or registering CT to the PET reference frame, will typically 6= the coordinate of a voxel
center, an interpolation scheme is required for registration. Trilinear interpolation
is significantly more accurate than nearest-neighbor interpolation and was used for
the registration method presented here.
Registration accuracy between the PET and CT components was assessed using
a phantom containing 4 refillable spheres with inner diameter (ID) = 5 mm (Data
Spectrum Corporation, Hillsborough, NC) arranged at several heights and filled
with FDG and iodine contrast (5.0% by volume). The phantom was fixed at
the center of the transaxial FOV and imaged once by CT. To examine registration
accuracy as a function of detector position, PET acquisitions (time = 12.5 minutes,
head separation= 262 mm) were performed at 6 detector heights at intervals of
13.4 mm. PET images from the lowest (0 mm) and highest heights were manually
registered with an affine transform to the CT images by qualitatively aligning
corresponding sphere center of masses using RView [114]. The scaling factor (s) in
(3.10) was determined by measuring the distances between spheres in the CT and
PET images. Values in the transformation matrices, describing the registration,
between the bottom (b) and top (t) heights were assumed to vary linearly as a
function of detector height and were described by parametric equations, defined
59
as follows:
tx = ttx − tbx (h/∆steps ) + tbx
(3.12)
ty = tty − tby (h/∆steps ) + tby
(3.13)
tz = ttz − tbz (h/∆steps ) + tbz
(3.14)
θx = θxt − θxb (h/∆steps ) + θxb
(3.15)
θy = θyt − θyb (h/∆steps ) + θyb
(3.16)
θz = θzt − θzb (h/∆steps ) + θzb
(3.17)
where h is the detector height in steps, ∆steps is the steps between the bottom and
top detector heights used in registration calibration, and remaining parameters
correspond to those given in (3.9) and (3.11).
Repositioning accuracy of the gantry was assessed by imaging the 4 sphere
phantom a total of 7 times, parking and then repositioning the scanner in between
acquisitions. PET images for the single height were registered to CT using the
parametric equations calculated in the detector position study. Error in registration was quantified by computing the Euclidian distance between sphere center of
masses (CM) in the PET and CT imaging domains.
3.2.6
Influence of PET on CT
The effect of the PET electronics and/or activity on CT image quality was quantified. The influence of the CT component on the PET has been reported previously
[100], and found that the background count-rate was significantly increased, and
peak-to-valley ratio in the flood histograms decreased, from the afterglow of the
LSO crystals after irradiation with scattered x-rays. Use of 3 mm lead plates,
60
particularly on the face of the detectors, was found to significantly reduce the degrading effects of the CT system on the PET component and are incorporated in
the current gantry (see section 2.4). A plastic refillable jar (ID=14 cm) and 70
µm thick nickel-chromium wire arranged perpendicular to the scanner’s transaxial
FOV were scanned by CT in 3 different configurations in this order: (1) jar filled
with water only and with the PET high-voltage (HV) off, (2) jar filled with water
only and with the PET HV on, and (3) jar filled with 259 MBq of FDG, at the
start of imaging, and with PET HV on. From the reconstructed CT images, the
modulation transfer function (MTF) was estimated from the wire as previously
described [94]. To estimate image uniformity individual circular regions of interest (ROI) (diameter = 12 cm) were drawn on coronal image slices, centered on
the cylinder, for slices spanning the scanner’s axial FOV. The mean and standard
deviation of voxel HU for each ROI were computed.
3.3
3.3.1
Results
Spatial Resolution for MAP Reconstruction
Tables 3.1 and 3.2 show the resolution measurements for the phantom arranged
parallel or perpendicular to the rotational axis of the scanner, respectively. Resolution measurements were taken for 11 profiles along the length of the line source
for each orientation. Average FWHM (FWTM) radial, tangential, and axial resolutions were 2.7 (5.5), 2.6 (7.1), and 2.2 (5.1) mm, respectively. For transverse
resolution measurements (table 3.1) radial and tangential FWHM resolutions had
minimal change at offset source positions, although a large increase was measured
for the tangential FWTM value. Axial resolution values were found not to depend
61
Table 3.1. Transverse spatial resolution (mm ± inter-slice σ) estimated from
MAP based reconstructions.
Offset from center (mm)
X Y
Radial (mm)
FWHM
FWTM
Tangential (mm)
FWHM
FWTM
0
0
2.7 ± 0.1
5.5 ± 0.3
2.7 ± 0.1
6.3 ± 0.4
47
0
2.7 ± 0.1
5.6 ± 0.2
2.5 ± 0.1
8.0 ± 1.2
Table 3.2. Axial spatial resolution (mm ± inter-slice σ) estimated from MAP
based reconstructions.
Offset from center (mm)
X Z
Axial (mm)
FWHM
FWTM
4
7
2.2 ± 0.1
5.4 ± 0.3
38
7
2.1 ± 0.1
5.2 ± 0.3
40
30
2.5 ± 0.1
4.9 ± 0.1
strongly on the line source position. Using OSEM reconstruction to estimate spatial resolution for two commercial dual-head PET scanners Schelper et al. [115]
found that although radial resolution was not sensitive to the radial position, tangential and axial resolution were found to degrade with radial offset. For an uncollimated dual-head PET scanner axial FWHM values were consistently less than
radial or tangential values [116], which agrees with the resolution measurements
for DbPET/CT. The reason for the significantly improved axial versus transverese
resolution measurements is not known.
It is important to note that the results presented here represent the resolutions
from high count scans. With patient imaging we have used a higher β value
(≈ 10−02 ) to improve SNR, and the resolutions in this scenario are expected to be
degraded compared to those presented in tables 3.1 and 3.2 [109]. Measurement
62
50
Prompts
Trues
Scatters
Randoms
NECR (1R)
NECR (2R)
45
40
Rates (kcps)
35
30
25
20
15
10
5
0
0
0.1
0.2
0.3
0.4
0.5
0.6
Phantom activity (mCi)
0.7
0.8
0.9
1
Figure 3.3. Rates versus phantom activity for a right cylinder phantom as
estimated from experimental acquisitions. NECR was estimated for direct(2R)
and variance reduce (1R) randoms subtractions.
of FWHM and FWTM values for reconstructions with β = 10−02 for the line
source data acquired here would not produce resolution values observed during
patient imaging due to the significant difference in count densities between the
phantom data and typical patient scans, as the point spread function has an inverse
relationship with count density for the same β for MAP [117].
3.3.2
Noise Equivalent Count Rates for a Cylinder Phantom
Count rates as a function of activity for a cylinder phantom are shown in figure
3.3. From the MC simulation scatter fraction (SF ) was measured at 23.5%. Using
63
a variance reduced randoms estimate (1R)(k = 1) was found to minimally increase
NECR, with the largest gains at phantom activities above those at peak NECR.
Peak NECR was 19.3 kcps and 18.6 kcps for variance reduced and direct randoms
subtraction, respectively, and occurred at a phantom activity of 318 µCi in both
instances. The randoms fraction at peak NECR was 4.2%, explaining the limited
sensitivity of NECR values to the randoms subtraction method employed.
NECR has been estimated for several other bPET and PEM systems using
different protocols from the one utilized here. Using a custom cylinder with offset
line source and the NEMA NU 2-2001 standard [108] Raylman et al. [3] measured
a peak NECR of ≈9 kcps for a four-headed bPET scanner. For the PEM system
from Naviscan, Luo et al. [106] calculated a peak NECR of 10.6 kcps via the NU
4-2008 small animal PET standard [107]. It is important to note that comparison
of NECR measurements between bPET and PEM systems is confounded by the
large variation in the phantom dimensions employed, and it can not be assumed
that DbPET/CT achieves ∼2x the NECR of the scanners cited here. Additionally,
it is expected that the addition of activity OFOV will lead to significantly lower
NECR values.
3.3.3
Noise Equivalent Count Rates for an Anthropomorphic Phantom
Count rate results from the anthropomorphic phantom study are shown in figure
3.4. The sudden dip in the randoms rates at ∼11 mCi was likely the result of
noise in the DAQ board acquisition time estimation. Peak NECR values and corresponding injection activities are given in table 3.3. Use of a variance reduced
64
35
Prompts
Trues
Scatters
Randoms
NECR (1R)
NECR (2R)
30
Rates (kcps)
25
20
15
10
5
0
0
2
4
6
8
10
Injection activity (mCi)
12
14
16
Figure 3.4. Rates versus estimated injection activity for an anthropomorphic
phantom. NECR was estimated for direct(2R) and variance reduce (1R) randoms subtractions.
Table 3.3. Peak, and 95% of peak NECR values, with corresponding activities,
for scans of an anthropomporphic phantom.
Randoms
Subtraction (k)
NECR (kcps)
Peak 95% of Peak
Injection Activity (mCi)
Peak 95% of Peak
Direct (2)
12.0
10.8
3.9
2.7
Variance Reduced (1)
12.8
11.6
5.2
2.9
randoms estimate (1R) increased peak NECR by only 7% compared to direct randoms subtraction (2R), while the activity at peak NECR increased 33%. Plots
of NECR values, as a function of injected activity, (figure 3.3) typically present
with characteristically broad and flat peaks. Consequently, it is possible to use
65
a significantly lower injection activiity than that corresponding to peak NECR,
thereby reducing radiation dose delivered to the patient while only marginally degrading system count rate capabilities. Based on emperical measurements Watson
et al. [57] suggested the optimal injection activity is that which delivers 95% of
the peak SNR. We estimated the activity at 95% of the peak SNR assuming that
√
SN R = N ECR, for equal unit time measurements. Activity at 95% of the peak
SNR was 44% less than activity at peak SNR, while the differential in NECR values was 1.2 kcps, for the case with variance reduced randoms subtraction (table
3.3). Randoms fraction at peak NECR was 8.7% and 5.7% for the 1R and 2R
cases, respectively, with the MC estimated SF =24%.
In terms of patient imaging, these results suggest that the randoms fraction may
not significantly influence NECR values for DbPET/CT. The reduction in peak
NECR values for the anthropomorphic phantom, in comparison with measurements
done with only activity in the FOV (see section 3.3.2), may be due largely to count
losses from front-end dead-time and pile-up.
3.3.4
Coincidence Photon Detection Sensitivity
The complete sensitivity profile as a function of detector height is shown in figure
3.5. Consistent with the sensitivity profile of fully 3D PET systems, sensitivity is
maximized with the source at the CFOV and decreases monotonically as the source
is moved towards the axial extremes. As the PET axial FOV is 11.9 cm, the counts
at absolute axial positions >6 cm are due mainly from scattered coincidences. Peak
sensitivity, after all corrections, was measured at 1.64%. Average dead-time across
all source positions was 7% (maximum dead-time=10%) and the average randoms
66
2
Sensitivity (%)
1.5
1
0.5
0
−6
−4
−2
0
2
Axial Position (cm)
4
6
Figure 3.5. Coincidence photon detection sensitivity measured from translating
a 68 Ge point source axially.
fraction was <1% of the rate of trues + scatters. Sensitivity without correcting for
randoms or LSO background was measured at 1.66%, suggesting that the influence
on sensitivity was not significant for these noise sources.
3.3.5
Registration Accuracy
Examining registration accuracy as a function of detector position the largest Euclidian distance between the CM of a single sphere (0.34 mm) occurs at a detector
height= 67.2 mm (figure 3.6). Average error for all 4 spheres over all heights is
0.16±0.08 mm. CM error does not significantly increase from the minimum average error (0.14 mm) as a function of vertical offset. For the repositioning study the
average error for all 4 spheres across all repositions is 0.20±0.10 mm, as shown in
figure 3.7. Only registration error at the 5th reposition (0.43±0.17) is significantly
greater (p=0.004) than the total average.
67
0.4
Euclidian Distance (mm)
0.35
0.3
0.25
0.2
0.15
0.1
0.05
0
0
10
20
30
40
50
60
Vertical Detector Height (mm)
70
Figure 3.6. Accuracy of affine registration between the PET and CT as a
function of detector height. Error bars represent the range.
0.8
Euclidian Distance (mm)
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
-1
0
1
2
3
4
5
6
7
Reposition Number
Figure 3.7. Accuracy of affine registration between the PET and CT as a
function of reposition number. Error bars represent the range.
3.3.6
Influence of PET on CT
Figure 3.8(left) shows the influence of the PET component on the MTF of the
CT. The MTF curve computed with only PET HV on (HV+ Act-) does not differ
significantly with the water only scan (HV- Act-). The MTF with HV on and
68
HV− Act−
HV+ Act−
HV+ Act+
MTF
0.8
0.6
0.4
0.2
0
0
0.2
0.4
0.6
0.8
f (1/mm)
1.0
1.2
150
Voxel intensity (HU)
1.0
100
50
0
−50
0
100
200
Coronal slice number
300
Figure 3.8. Influence of PET electronics and activity on CT image quality for
HV off and no activity in the FOV (HV- Act-), PET HV on and no activity
(HV+ Act-), and PET HV on and activity present (HV+ Act+). MTF vs. line
pair frequency (left). Image uniformity (mean and standard deviation bars)
as a function of CT coronal slice number (lower magnitude is more posterior)
(right). Standard deviation bars are representative of typical values and are
staggered between imaging scenarios for clarity.
activity (HV+ Act+) differs by at most 0.074 from the other imaging scenarios
(frequency=0.33 mm−1 ). The difference is likely insignificant, and may be attributed to the subtle variation of image artifacts induced by slight motion of the
uniform cylinder during activity filling.
Figure 3.8(right) shows how CT image uniformity is affected by the PET component. Differences in mean HU between the water only scan and acquisitions
with PET HV (HV+ Act-) and activity (HV+ Act+) are not significantly greater
than the interscan HU fluctuations measured on the CT component alone.
69
Chapter 4
Performance During Patient
Imaging
4.1
Introduction
Although several clinical trials have examined the diagnostic accuracy of 18 F-FDG
PEM for detecting lesions for women highly likely to have breast cancer (see section
1.9.1.2) there have been no studies, to our knowledge, of bPET performance during
patient imaging. Based on prior phantom measurements (see chapter 3) and bCT
imaging studies [104] we hypothesize that DbPET/CT may have distinct limitations for patient imaging which may reduce the system’s ability to detect cancer.
In terms of patient related issues, it is not clear if the subject can tolerate prone
positioning for an extended time period, or if significant motion of the patient’s
breast may occur during the PET acquisition. Additionally, the PET scanner’s
transaxial FOV (12 cm) is significantly less than the average breast diameter (∼ 14
cm), which may cause image artifacts due to incomplete radial sampling. Furthermore, the multiplexed detector readout of the PET component is especially prone
to front-end dead-time count losses, which may reduce SNR in reconstructed pa-
70
tient images. In this study we perform a patient trial with DbPET/CT to gain an
initial understanding of how aforementioned limitations may influence radiological
interpretation of images and system performance. Results from this study were
published by Bowen et al. [118].
4.2
4.2.1
Materials and Methods
Patient Trial
A clinical trial is currently being conducted with DbPET/CT involving women
with a high probability of having breast cancer (BI-RADS category 5) as determined through mammography [89]. Currently, we have imaged a total of 7 breasts
from 4 patients (1 subject underwent a prior mastectomy). This and related protocols have been approved by the UC Davis Medical Center institutional review
board and require written consent of the subject. Eligible subjects are 35-80 years
old (range of study subjects: 49-70 years old), have not had a recent breast biopsy,
and are not pregnant or diabetic. Before injection with FDG (range: 174-477
MBq), subjects fasted for >4 hours and were checked with a finger-stick test to
ensure normal blood glucose levels (<200 mg/dL). Patients were asked to void
their bladder before positioning on the scanner with the affected breast in the
FOV first, unless otherwise noted. A CT scan was performed with the patient
coached to perform end expiration breath holding. The technologist then used
the hand-controller to position the PET heads as close as possible to the patient’s
chest wall. The patient was advised to breathe normally and scanned for 12.5 minutes by PET (average uptake time=81 minutes, range=73-89 minutes). Patients
were then repositioned for unaffected breast imaging. PET and CT images were
71
processed and reconstructed as in section 2. For this study, reconstructed PET
data were corrected for center of rotation offset and geometrical efficiency factors.
Randoms subtraction, scatter, attenuation, and dead-time corrections were not
implemented. All patient images presented are windowed between -450 to 250 HU
for CT, and 0 to 95% maximum image intensity for PET, unless otherwise noted.
Additionally, dedicated CT images represent an average of 3 slices in the plane
displayed.
For one subject a modified protocol was used for DbPET/CT imaging with
intravenous CT contrast agent. Scanning proceeded as follows: imaging of the
unaffected breast as detailed above, scanning of the affected breast with PET,
and scanning with CT before and 35 seconds after injection of 100 cc of iodixanol
(320 mgI/ml) (Visipaque 320, GE Healthcare, Waukesha, WI) with a power injector (Mark V Plus, Medrad, Warrendale, PA). A contrast subtraction image was
produced by subtracting pre- and post-contrast CT scans rigidly registered with
RView [114].
Subjects underwent additional imaging tests as part of their standard workup.
The suspicion of multifocal or multicentric disease, or inconclusive findings on
mammography (BI-RADS category 0), prompted 3 subjects to undergo bilateral
dynamic contrast enhanced magnetic resonance (DCE-MR) imaging. One subject
suspected of distant spread was scanned prone on WB PET/CT (Discovery ST,
GE Healthcare, Waukesha, WI) (acquisition time= 5 min per bed) with images
reconstructed by the manufacture’s software as follows: PET) OSEM (2 iterations,
30 subsets) with voxels of size 5.1 x 5.1 x 3.3 mm, and CT) voxels of size 1.0 x 1.0
72
x 3.7 mm.
An effort was made to spatially register tomographic images with histological
findings. A mastectomy sample was cut by hand in sagittal slices (slice thickness 5 mm) and photographic images were obtained for each slice. Histology was
performed at several locations on a slice with suspicious lesions. For comparison,
DbPET/CT, DCE-MR, and WB PET/CT sagittal slices were selected qualitatively based on the similarity of fibroglandular structure with the tissue section.
Sagittal sections were aligned unaltered (i.e. without corrections for soft tissue
deformation or rigid rotations of the breast).
For DbPET/CT image interpretation one board certified radiologist specializing in breast imaging reviewed only the CT images, while a second radiologist
with expertise in nuclear medicine reviewed the fused image sets (the CT was used
only as an anatomical reference and a final interpretation was made based on the
PET image). Readers had access to all prior breast exams and images from mammography, DCE-MRI, and WB PET, if available, including the interpretation of
the dedicated CT images in the case of the fused image reader. Based on qualitative metrics each reader determined if suspicious lesions (positive) were present on
DbPET/CT images, and if so, correlated these findings with histopathology.
4.2.2
Count Rates Estimations from Patient Scans
Noise equivalent count rates (NECR) were estimated from patient scans [55]. To
only include randoms (estimated from delayed coincidences) and scatters with
lines of response (between crystal i and j) passing through breast tissue at a given
projection angle (θ), a binary histogram mask (mijθ ) defining the interior of each
73
breast was generated from patient PET images [57]. The scatter fraction (sfθ )
was estimated using the Monte Carlo simulation software GATE [110]. A digital
breast phantom of each patient’s breast was composed of both an activity and
attenuation map estimated from the original patient PET images. Activity from
outside the FOV (e.g. patient torso) was not included as this was not expected to
have significant contribution on the total scatter fraction [38]. Integral counts for
trues (Tθ ), randoms (Rθ ), and prompts (Pθ ) and NECR values were calculated as
follows:
Tθ = (1 − sfθ )
X
(pijθ − rijθ ) mijθ
(4.1)
ij
Rθ =
X
rijθ mijθ
(4.2)
pijθ mijθ
(4.3)
P
( θ Tθ ) 2
P
NECR = P
θ Rθ
θ Pθ + (k − 1)
(4.4)
ij
Pθ =
X
ij
1
∆t
where pijθ and rijθ are prompts and randoms counts, and ∆t is the total acquisition
time. In equation (4.4) k=2 or k=1 for direct or variance reduced randoms subtraction, respectively. For each patient, the injection dose of FDG was normalized
to a value that would give the same initial total activity in the patient after a 60
min uptake, as the actual average activity present during the scan as previously
described [57].
To assess the relative contribution of randoms as a function of breast volume
the energy qualified singles to trues ratio (STR) was computed for patient scans.
The STR is a surrogate for the randoms fraction with the advantage that it does
74
Table 4.1. Radiological Interpretation for DbPET/CT Affected Breast Images
Case Number
1
2
3
4
Cancer Type
invasive mammary
DCIS
invasive lobular
DCIS
invasive ductal
CT Positive
Yes
No
No
Yes
Yes
PET Positive
Yes
Yes
Yes
No
Yes
not depend on activity in the FOV. As energy was not recorded for singles, events
falling in the 350-650 keV window were estimated by scaling recorded singles by
the square root of the ratio of windowed to non-windowed randoms. In addition,
both singles and trues were dead-time corrected to account for differences in the
system count-rate response.
4.3
4.3.1
Results
Patient Trial
Table 4.1 summarizes the radiological interpretation of DbPET/CT images from
the patient trial. For patient case 2 an earlier iteration of the patient bed limited
the volume of breast tissue visible on CT such that the invasive lobular carcinoma
was above the top of the CT axial FOV (figure 4.3). In case 3 the CT component
was able to visualize calcifications representative of DCIS, but the PET images
were not interpretable due to inaccurate registration, likely due to patient motion
(figure 4.4). Patient cases 1 and 4 are discussed below.
Figure 4.1 shows DbPET/CT images for the case 1 subject’s affected breast.
The 49 year old patient presented with a palpable 23 mm irregular focal mass
at the 8 o’clock position, as seen on mammography. The axial fused image (see
figure 4.1A) shows 3 separate areas of focal uptake visible on PET overlaying
75
A
B
Figure 4.1. (A) Axial and (B) coronal DbPET/CT images from the affected
breast of the case 1 subject. Panels from left to right represent CT, PET, and
fused images.
fibroglandular tissue as visualized by CT.
Figure 4.2A shows a tissue section excised from the mastectomy sample of the
case 1 subject. Histology results in figure 4.2B obtained at several locations on the
tissue section show a band of DCIS superior to a benign region of fibroglandular
tissue. Figure 4.2C shows a fused sagittal DbPET/CT image corresponding to the
tissue section. Areas of increased uptake on PET overlay malignancies (boxes i-iii)
while a region with uptake not significantly above background (box iv) overlays
benign tissue. No indications of DCIS were visible on the CT images alone (see
table 4.1). Figure 4.2D shows a sagittal image from a WB PET/CT acquisition
(tube voltage= 140 kVp, injection activity= 466 MBq, uptake time= 76 min) obtained 29 days after imaging with DbPET/CT. The fused image from DbPET/CT
(figure 4.2C) shows qualitatively improved resolution compared to WB PET/CT
(figure 4.2D) for both the PET and CT components. Regions of increased contrast
76
B
A
i
C
D
E
i
i
ii
iii
iii
ii
ii
iv
iv
iv
Figure 4.2. (A) Sagittal tissue section excised from a mastectomy sample of the
case 1 subject’s affected breast with 4 areas (boxes) of histology performed. (B)
Histology tissue slides with magnified regions (right, corresponding to black
boxes) revealed DCIS alone (i-ii), or with intralymphatic invasion (iii, not
shown), and benign tissue (iv). (C) DbPET/CT, (D) WB PET/CT, and (E)
DCE-MR sagittal image slices corresponding to the tissue section (A). Boxes
in the DbPET/CT image (C) are at locations approximating those in the tissue section (A). PET images (C and D) were windowed between 0 and 60%
maximum image intensity.
2.6 cm
Figure 4.3. Axial DbPET/CT images from the affected breast of the case 2
subject. Panels from left to right represent the fused images and the PET
alone. Measurement given in the fused image is the distance between the top of
CT and PET FOV. PET images were windowed between 0 and 75% maximum
image intensity.
visible on DbPET/CT (figure 4.2C) correlated well with those seen on DCE-MR
(see figure 4.2).
Figures 4.5A and B show CT and fused sagittal images, respectively, of the
affected breast of the case 4 subject. The 66 year old patient presented with a
20 mm spiculated mass at 10 o’clock (posterior third) as seen on mammography.
77
A
B
C
Figure 4.4. Coronal DbPET/CT images from the affected breast of the case
3 subject. Shown are the CT (A), PET (B), and fused image. Arrow in (A)
denotes a calcification at the approximate location of biopsy confirmed DCIS.
A
B
8 mm
C
150
HU
0
Figure 4.5. (A) Pre-contrast CT, (B) fused PET/CT, and (C) contrast subtraction sagittal DbPET/CT images showing the affected breast of the case
4 subject. Two areas of focal uptake were seen on PET (B) and on contrast
subtraction CT (C) (arrows). (B) The distance (opposing arrows) between the
top of the PET axial FOV (dashed line) and anterior aspect (solid line) of the
pectoralis muscles (dotted line) is shown. (C) The contrast subtraction image
is an average of 7 slices and uses alternative windowing.
The fused image (see 4.5B) shows two areas of focal uptake anterior and posterior on PET, determined by biopsy to be multifocal cancer (see table 4.1). The
78
Table 4.2. NECR Values from Patient Scans
Breast Number*
1A
1U
2A
2U
3A
4A
4U
Normalized Injection Activity (MBq)
196
157
324
270
382
118
145
Singles (kcps)†
296
207
492
412
536
195
232
NECR (k=1) (cps)
1474
793
154
145
107
400
503
NECR (k=2) (cps)
1247
668
94
89
61
323
401
Scatter Fraction (%)
30
21
15
10
17
25
25
Breast Volume in PET FOV (cm3 )
1077
532
204
185
391
965
1001
*
Case number followed by the breast scanned: affected (A) or unaffected (U).
†
Dead-time corrected, energy windowed (350-650 keV) and averaged over projections and detector heads.
Detector separation was 20.6 cm for cases 1 and 2, and 26.3 cm for cases 3 and 4.
proximity of the top of the PET axial FOV with respect to the case 4 subject’s
pectoralis muscles is also visualized in Figure 4.5B. Figure 4.5C shows the CT
contrast subtraction image.
4.3.2
NECR from Patient Scans
Table 4.2 shows NECR values estimated from patient scans. Average NECR (k=1)
was 511 cps (range: 107-1474 cps) with the largest NECR for the affected breast
of patient case 1 (breast number=1A) (trues=2575 cps, randoms=819 cps). The
results show the scatter fraction to be significantly correlated with breast volume
in the FOV (R2=0.92 for linear fit). In addition, subtraction with a variance
reduced randoms estimate (k=1) increases NECR by up to 75% (average for all
breasts=41.3%), compared to direct subtraction (k=2), for the breast imaged with
the largest normalized injection activity (breast number=3A). Figure 4.6 shows
79
1,000
Singles:Trues
800
600
400
200
0
0
200
400
600
800 1,000 1,200
Breast volume (cm3)
Figure 4.6. Plot of the STR versus breast volume in the PET FOV for patient scans. Data was fitted with a first order polynomial (–) with correlation
coefficient (R2 ) = 0.72.
the STR plotted as a function of breast volume. The largest STR was for breast
number=3A (ratio=722), while the smallest was for breast number=1A (ratio=92).
4.4
Discussion and Conclusions
Scanning of the uncompressed breast with DbPET/CT can produce fully 3D images that accurately show the size, extent, and location of biopsy-confirmed breast
cancer. For case 1 invasive carcinomas were visible adjacent to a breast implant
(see figure 4.1). Implants may reduce the sensitivity of mammography even with
the use of implant displacement views ([119]). In this same patient, features presenting on the functional and anatomical images from DbPET/CT correlated well
with histological results and gross anatomy, respectively (see figure 4.2). The histological correlation for case 1, along with the radiological interpretation (table
4.1) of cases 1, 2, and 4 (figure 4.5) suggest that PET images can be accurately
registered to the CT during human imaging; however, in case 3 registration appeared degraded due to subject motion. Use of a specialized breathing protocol
80
for breast imaging, improvements in the patient bed and mild compression could
all potentially reduce registration error.
For patient case 1 DbPET/CT was shown to have qualitatively improved visualization of DCIS (figure 4.2) compared with a commercial WB PET/CT scanner
(Fig. 4D). A patient trial with PEM [88] measured a sensitivity for DCIS (91%) significantly higher than values typically reported for WB PET. A known limitation in
our comparison was the method used for registering tomographic image slices (WB
PET/CT, MR, or DbPET/CT) to the tissue section. Sagittal slices were aligned
unaltered based on qualitative matching resulting in visibly reduced spatial correlation. Other factors potentially biasing the inter-modality comparison include
differences in acquisition parameters, count rates, reconstruction algorithms, and
correction methods. Nevertheless, we believe that the increased resolution of the
dedicated versus WB scanner for both the PET (average FWHM for WB= 6.4
mm, dedicated= 3.7 mm)[60, 100] and CT (average resolvable line-pairs for WB=
0.7 mm-1, dedicated= 1.1 mm-1)[94, 120] results in an appreciable improvement in
lesion visualization for a patient that was scanned with typical clinical acquisition
protocols.
Besides providing anatomical reference the CT component of DbPET/CT increases the overall system functionality compared with breast PET alone. In case
4 the combination of increased x-ray density with FDG uptake or iodine contrast
(figure 4.5) accurately localized a suspicious lesion that was originally occult on
screening mammography. While iodinated contrast and FDG have high spatial correlation in this case, the kinetics of the two tracers are regulated by independent
81
physiological processes (angiogenesis for iodinated contrast vs. glucose metabolic
rate for FDG), such that differences in iodinated contrast and FDG uptake could
potentially improve reader confidence or quantitative measures for a given lesion.
The CT component may also improve the utility of recently developed robotic
biopsy devices [95, 116]. Fused 3D DbPET/CT images would allow for accurate
needle placement while the CT, operating in low-dose fluoroscopy mode, could
provide real-time needle guidance.
NECR values from patient scanning (table 4.2) are influenced significantly by
breast volume in the scanner FOV. In contrast to WB PET systems the randoms
fraction for the dedicated PET scanner, as estimated by the STR (figure 4.6), is
inversely related to the volume of tissue in the FOV [57]. This inverse relationship
supports predictions that image noise for prone dedicated breast PET scanners
may be significantly influenced by activity from out of the FOV [61]. The large
magnitude of singles flux from the brain, torso, or bladder dominates any increase
in singles with breast volume. Loss of trues from self attenuation does not appear
to play a significant role due to the relatively small range of breast dimensions
compared with the torso. Assuming relatively constant singles flux, the randoms
fraction declines more rapidly than the scatter fraction increases as a function of
breast volume, and all other things being equal, NECR is greater for larger breasts.
The method of estimating scatter fraction from patient scans using MC simulations had some limitations. For example, in several instances the breast volume
exceeded the transaxial FOV of the PET component, potentially leading to an
underestimation of the true SF. In addition, differences in scatter fraction were
82
20
4
A
10
Anthro Trues
Patient Trues
Anthro NECR
Patient NECR
5
0
Randoms (kcps)
Rates (kcps)
15
0
2
4
6
8
Injected Activity (mCi)
10
B
Anthro
Patient
3
2
1
0
0
2
4
6
8
Injected activity (mCi)
10
Figure 4.7. Comparison of patient rates with anthropomorphic phantom data
measured from section 3.3.3. (A) Comparison of trues and NECR and (B)
comparison of randoms as a function of estimated injected activity. Activity for
the patient data represents the normalized injection activity.
measured for breasts with comparable volumes (observe 2A and 2U in table 4.2).
These SF differences were likely due to the spatial distribution of breast tissue
within the PET FOV, and do not necessarily represent a discrepancy in the simulation method itself, as suggested by the strong correlation between SF and breast
volume.
Rates estimated from patient data were found to significantly underestimate results from the anthropomorphic experiments in section 3.3.3. Figure 4.7 compares
trues and randoms rates, and NECR between the patient and anthropomorphic
phantom. Over a comparable injection activity range trues rates from the anthropomorphic phantom experiment were a factor of ∼17 the patient trues, while for
the same range anthropomorphic randoms were a factor of ∼3 the patient randoms. This analysis suggests that the significant bias in NECR values for the
anthropomorphic phantom results compared to the patient study is largely from
the overestimation of trues in the phantom experiments. Use of an alternative
83
breast phantom than the cylinder used in section 3.3.3 or a reduced activity concentration, with respect to the OFOV activity compartments, may improve the
correlation between the phantom model and patient data.
Some limitations exist for patient imaging with the current DbPET/CT. Chest
wall and breast axillary tail coverage of both modalities is restricted due to the
geometrical constraints inherent with prone imaging. With the current bed setup
the top of the axial FOV for the CT can be positioned closer to the chest wall than
for the PET; a 20 mm difference was measured in one patient (see figure 4.5). We
note that chest wall coverage limitations are likely worse for rotational systems,
however, in two clinical imaging studies with PEM false negatives were reported
when lesions were above the scanner axial FOV [86, 88].
84
Chapter 5
Implementation and Validation of
Data Corrections
5.1
Introduction
Based on the results of the clinical trial described in chapter 4 we determined
what factors are expected to most significantly influence image quantification for
DbPET/CT. Table 5.1 summarizes the operating conditions measured during patient scanning. Results suggest that attenuation (based on the breast diameter)
dominates image bias for the median sized breast, although randoms can significantly degrade contrast at higher activities and smaller breast volumes. The scatter
fraction range observed lies substantially below the range typically measured with
WB PET [57], while count losses from dead-time were significant and may be attributed to the large contribution of singles flux from outside the FOV (OFOV)
combined with the multiplexed detector readout of the electronics. Using the operating conditions from patient imaging as a guide, we developed data correction
schemes and validated these methods with custom performance measurements for
DbPET/CT.
85
Table 5.1. PET performance characteristics of the DbPET/CT scanner during
patient imaging.
Metric
Scatter
Fraction (%)
Randoms
Fraction (%)
System
Dead Time (%)
Singles
(kcps)
Breast
Diameter (cm)a
Min
10.0
22.2
18.7
195.1
10.1
Max
30.0
296.8
45.1
535.6
18.1
Median
21.4
33.9
28.8
295.6
14.0
a
Represents min and max for 95% range [104]
5.2
Materials and methods
5.2.1
Correction methods.
5.2.1.1
Overview
An estimate of the relative activity (ˆ
auivjθ ) for a LOR formed by transaxial crystal
element i and ring u in detector head 1 and crystal j and ring v in detector head
2 at detector angle θ for DbPET/CT is given by:
a
ˆuivjθ ∝ [puivjθ − rˆuivjθ − sˆuivjθ (εui εvj )] ACFuivjθ Dθ (LTθ εui εvj Ωuivj )−1
(5.1)
where puivjθ is the sinogram of prompts, rˆuivjθ and sˆuivjθ estimates of the randoms
and scatter sinograms, respectively, εui εvj the product of detector efficiency factors, Ωuivj the geometric efficiency factors, ACFuivjθ the attenuation correction
factors, Dθ the inter-projection decay correction terms, and LTθ the system livetime factors. Using the decay constant of
18
F (λ=109.8 minutes) Dθ is calculated
as follows:
Dθ = exp(λ · (tθ − t0 )
(5.2)
where tθ and t0 are the mean projection times for the acquisition at rotation angle
θ and the starting acquisition angle, respectively. Estimation of the remaining
86
correction terms is discussed in the proceeding text. For a discussion of the phenomena that require each of the corrections see section 1.5.
5.2.1.2
Normalization.
A component based method is used to compute normalization factors for individual
LORs. Geometric efficiencies (Ωuivj ), which account for solid angle coverage and
crystal attenuation path length, are estimated with a Monte Carlo (MC) simulation
using SimSET [121]. The MC model of the scanner accounts for coherent scatter
in the detectors, air gaps between crystals, and assumes an energy resolution of
25% at 511 keV [100]. A high count simulation of a plane source is executed, with
the detector heads at a single angular position parallel to the source, and only true
coincidences (those not undergoing scatter in the object) falling in a 350-650 keV
energy window are recorded. To reduce simulation time and/or reduce variance
in the geometric efficiences the symmetries of the planar detector geometry are
exploited. All Ωuivj with the same ring (Dr = u − v) and transaxial crystal
difference (Dt = i − j) are averaged resulting in a noise reduction factor of:
NLOR = (Nr − |Dr |) (Nt − |Dt |)
(5.3)
where Nr and Nt are the number of rings and transaxial crystal elements, respectively. In addition, transaxial (for i 6= j) and axial (for u 6= v) symmetries can be
applied resulting in a total noise reduction factor of up to 4NLOR . For the PET
component of DbPET/CT, with Nr = Nt = 36, a maximum reduction factor of
4900 is achieved. In (5.3) it is assumed that Dr and Dt are proportional to physical distances between crystal elements. Inter detector dead space is minimized
via optical fiber bundles [122] and the crystal pitch is assumed 3.3 mm through-
87
out. The product of detector efficiencies (εui εvj ) are estimated from a high count
experimental acquisition of a uniformly filled plane source for the detector heads
at a single angular position parallel to the source. Raw prompts are corrected for
Ωuivj , path length through the source, and attenuation before variance reduction
using the fully 3D Casey method [123].
For all experiments for which normalization was applied, Ωuivj were calculated from a simulation resulting in a variance equivalent of 513 million recorded
trues (≈300 counts/LOR) before application of the variance reduction methods
discussed previously. Computation of εui εvj was performed from a scan of an 18
mm thick plane phantom (total acquisition time=820 minutes) with a maximum
initial activity of 141 µCi (18 F-FDG) resulting in a total of 233 million prompts.
5.2.1.3
Dead-time.
Live-time (LT) for energy windowed prompts is computed on a projection-byprojection basis using a multi-component model based on [46]. The total system
LT is estimated as follows:
LTθ = LTU T S1iθ , S2iθ · LTU E S1iθ + S2iθ · LTD (Pθc )
(5.4)
where S1iθ and S2iθ are the incident singles rates on heads 1 and 2, respectively,
Pθc is the prompts rate recorded by the NIM counters, and LTU T , LTU E and LTD
model dead-time losses due to trigger induced pile-up, energy related pile-up, and
the coincidence DAQ, respectively. All rates represent those before energy windowing, and are only influenced by the voltage trigger threshold of the constant
fraction discriminator (CFD). The inability of DbPET/CT electronics to acquire
energy information for singles before coincidence detection has led to the use of
88
a multi-component model for dead-time and pile-up count losses. Dead-time due
to overlapping trigger pulses alone (loss of one or more counts) is modeled by
LTU T while count losses due to both overlapping trigger pulses combined with a
summation of energy greater than the upper level discriminator (ULD) (loss of
two or more counts) are accounted for by LTU E . Equations for the individual LT
components are as follows:
LTU T S1iθ , S2iθ = exp −τS1 S1iθ − τS2 S2iθ
(5.5)
LTU E S1iθ + S2iθ = exp−τU E S1iθ + S2iθ
(5.6)
LTD (Pθc ) = (1 + τD Pθc )−1
(5.7)
where τS1 , τS2 , τU E and τD are characteristic dead-time coefficients.
Coefficients τS1 , τS2 , and τD were estimated in [100] and are equal to 141 ns,
150 ns, and 3.51 µs, respectively. Estimation of τU E was accomplished by scanning
a right cylinder phantom (OD=7.5 cm, height=11.1 cm) filled uniformly with 18 FFDG (initial activity = 1.0 mCi) periodically over the course of 18 half-lives.
Energy windowed prompts rates recorded from the DAQ (Ptwd ) as a function of
acquisition time (t) were corrected as follows:
0
ˆ t LTD (P c ) · LTU T S1i , S2i −1
Ptwi = Ptwd − R
t
t
t
(5.8)
0
where P wi is the rate of energy windowed trues and scatters with all dead-time
ˆ t is the rate of the corrected randoms as estimated
corrections except LTU E and R
in (5.9). Incident energy windowed prompts (Ptwi ) were estimated by fitting a
0
linear line to Ptwi as a function of S1it + S2it at a low activity range. A value of
0
103 ns for τU E was calculated by fitting (5.6) to the ratio of Ptwi over Ptwi as a
89
function of S1it + S2it .
5.2.1.4
Randoms.
Patient imaging results have shown that variance reduced randoms subtraction
can increase NECR by up to 75% (average=41%)[118]. Variance reduced randoms
sinograms (ˆ
ruivjθ ) are estimated from delayed coincidences on a projection-byprojection basis with:
P
rˆuivjθ =
w,x ruiwxθ
P P
w,x
P
y,z ryzvjθ
y,z ryzwxθ
!
LTD (Pθc )
LTD (Rθc )
∆tP,θ
∆tR,θ
(5.9)
where ruivjθ is the raw energy windowed delayed coincidences, Rθc is the randoms
rate recorded by the delayed coincidence NIM counter, and ∆tP,θ and ∆tR,θ are the
acquisition times for a step recorded by the prompts and randoms DAQ, respectively. The first term on the right-hand side of (5.9) performs variance reduction on
delayed coincidences using the fully 3D implementation of the Casey and Hoffman
method [123]. The amount of variance reduction is related to the number of LORs
summed over. For the results presented here the limits were set to include all
crystals in both detector heads. In (5.9) two correction terms are used to account
for the differences caused by acquiring prompts and randoms on separate DAQ
boards (see figure 2.2). The middle term on the right-hand side of (5.9) adjusts
the recorded randoms to exhibit the same dead-time as the prompts, while the
last ratio accounts for the slight variations between the user specified and recorded
(∆tP and ∆tR ) acquisition times for each DAQ board.
5.2.1.5
Attenuation.
Attenuation correction factors (ACF) are calculated with a CT based segmentation
method based on [124]. Figure 5.1 shows the process for ACF estimation using a
90
(a)
(b)
(c)
(d)
Figure 5.1. CT based ACF estimation for a patient image set. (a) The original
CT image, (b) the segmentation of (a) to a uniform linear attenuation value
and resolution matched to the PET, (c) the registration of (b) to the PET
reference frame and (d) the forward projection of (c) into sinogram space. The
red line in (c) denotes the approximate coronal slice for which the sinogram in
(d) corresponds.
patient data set. CT images are segmented with an intensity based method into
air and tissue compartments, with tissue assigned a uniform linear attenuation
coefficient (µ511keV ). Segmentation intensity thresholds were specified by the user
in this study. To match the average resolution of the PET image the segmented
CT image volume is convolved with a 3D Gaussian blurring kernel (643 voxels)
with full width at half maximum (FWHM) set to 3.3 mm. Blurred images are
registered and downsampled to PET with an a priori computed affine transform
and trilinear interpolation [118]. As the CT transaxial FOV ( 20 cm) is significantly
greater than that of the PET (12 cm), registered images are padded to match the
X-Y (transaxial plane) dimensions of the CT, minimizing potential artefacts from
breast tissue outside the PET FOV. ACF are computed by forward projecting the
segmented images into PET sinogram space with an implementation of the Siddon
algorithm [111].
5.2.1.6
Scatter.
Scatter (ˆ
suivjθ ) is estimated in full 3D using the Monte Carlo (MC) simulation software SimSET [121] (see section 5.2.1.2 for a description of the simulation model).
91
Iterate
Correct for
LT, r and ε
Experimental
t+s
Correct for
Ω, AT
Reconstruct
True Emission
Estimate Image
Segmented
Attenuation
Image
SimSET Simulation
Experimental
Prompts
if(Iter.>1)
Correct for s
Radial Blur
Simulation s
Simulation t
and s
Run Short
Simulation
s Estimate
Scale
Simulation s
Run
Extended
Simulation
Estimate
Decays
Figure 5.2. Schematic of the MC scatter estimation. Key: t=trues sinogram,
s=scatters sinogram, r =randoms sinogram, AT =attenuation, Iter.=iteration
number.
Figure 5.2 shows a schematic of the complete scatter estimation method. For the
MC portion of the scatter algorithm the attenuation map is estimated from the segmented CT image as in section 5.2.1.5. MC correction methods are inherently more
computationally expensive compared to analytic, dual-energy, convolution, or tail
fitting approaches, and as such suffer from a computation time versus noise tradeoff. Optimally, simulation time, or total number of decays, should be adjusted on
an acquisition-by-acquisition basis such that the noise of the scatter estimate is
significantly less than the noise of the experimental scatter data. We propose the
following equation for estimating the number of decays (Df ) to simulate based on
the coefficient of variance (COV) of the experimental sinogram:
Df = Di SF
COVsˆM Ci
f · COVp−ˆr
2
(5.10)
where Di is the number of decays used in a short simulation (see figure 5.2),
COVsˆM Ci the COV for the scatter sinogram of the short simulation, COVp−ˆr the
92
COV for the experimental trues and scatters, SF the scatter fraction for the acquisition as estimated from the short simulation, and f the factor that determines the
reduction in COV for the scatter estimate with respect to the experimental data.
The COV estimates represent the average value over all θ for all LORs passing
through the object as determined through the ACF. The MC scatter estimation
can be run iteratively producing a progressively more accurate scatter estimate as
a function of the iteration number. At the end of each iteration sˆuivjθ is computed
C
by radially blurring the MC scatter sinogram (sM
uivjθ ) with a user specified Gaussian
kernel and scaling the result to match the experimental data as follows:
P
sˆuivjθ =
(puivjθ − rˆuivjθ ) (LTθ εui εvj )−1 M C
P MC
sˆuivjθ
C
tuivjθ + sM
uivjθ
(5.11)
C
MC
where sˆM
uivjθ is the radially blurred MC scatter, tuivjθ the MC trues, puivjθ the
experimental prompts sinograms, and the summations are over the complete sinogram space. The argument of the summation in the numerator of (5.11) is equal
2
to COVp−ˆ
r in (5.10). To reduce computation time the code has been written such
that multiple MC simulations can be run in parallel.
5.2.2
Validation experiments
5.2.2.1
General acquisition and data processing.
All data were acquired, or simulated, with a detector separation distance (crystal
face-to-face) of 26.3 cm. PET prompts and delayed list-mode data were subject
to a 350-650 keV energy window (crystal-by-crystal basis). For reconstruction 2D
filtered back projection was used after either single-slice rebinning (SSRB) [125] or
Fourier rebinning (FORE) [126] . Maximum ring difference for SSRB and FORE
was set to 35, with FORE radial frequency (wlim ), angular frequency (klim ), and
93
(a)
(b)
Figure 5.3. Phantoms used for the assessment of dead-time and randoms correction accuracy.(a) HDPE right cylinder with line source offset 3.8 cm from the
center alone or (b) combined with a uniform filled cylinder (outer diameter=7.5
cm, height=11.1 cm) placed outside the FOV. The position of the phantoms
with respect to the detector heads is visible in (b).
ring difference (δlim ) limits all equal to 5. All correction and measurement code
was written in C/C++ and MATLAB
5.2.2.2
®(The MathWorks, Inc., Natick, MA).
Dead-time and randoms.
Count-rate linearity, after correcting for dead-time and randoms, was assessed with
a solid high density polyethylene (HDPE) right cylinder (OD=10.2 cm) with offset
line source, as shown in figure 5.3(a). The phantom was filled with
18
F-FDG and
scanned by PET with 20 minute acquisitions (25 minute duty cycle) for 10 halflives (initial activity= 0.5 mCi). As only the open energy windowed singles rates
are recorded (S1c and S2c ) and used for correction in (5.6) and (5.5), LTU E factors
may have reduced accuracy if the energy distribution of singles around the ULD
varies for a given value of S1c + S2c (e.g. through a significantly different source
distribution than used for τU E estimation). This potential inaccuracy was tested
by imaging the HDPE cylinder as positioned previously with a uniformly filled jar
placed OFOV (total initial activity= 1.0 mCi)(ratio of activity=1:1) as shown in
94
ID=1.9 cm
7.0 cm
C
H
B
H
C
11.0 cm
10.9 cm
OD=8.9 cm
B
ID=8.9 cm
ID=2.0 cm
(a)
(b)
(c)
Figure 5.4. Phantoms used for attenuation validation and assessment of accuracy for scatter correction. (a) Schematic of digital phantom used in attenuation
validation, with hot (H), background (B), and cold (C) compartments. (b) Photograph and (c) schematic of fillable acrylic phantom used for assessing scatter
correction accuracy. Key: OD = outer diameter, ID= inner diameter.
figure 5.3(b). Images were reconstructed after SSRB with data sets uncorrected or
corrected for combinations of dead-time and randoms and residual error between
incident and corrected counts was calculated based on [108].
Bias after randoms variance reduction was estimated using the methods of
Badawi et al. [127]. Data was acquired from a uniformly filled jar placed off center
as in section 5.2.2.5 and randoms were saved both unprocessed and with variance
reduction applied (using only the he first term on the right-hand side of (5.9)).
Sinograms (histograms) were separately summed across all projection angles (θ)
and the ratio of the raw and variance reduced summed histograms calculated. The
percent coefficient of variation was calculated for the ratio sinogram both before
and after median smoothing with a 16x16 kernel.
5.2.2.3
Attenuation validation.
Accuracy of the CT based attenuation correction method was calculated with a
MC simulation of DbPET/CT using SimSET. The purpose of this experiment was
95
solely to validate the correction code. Performance of the attenuation correction
with experimental data was assessed in section 5.2.2.5. The simulation model
was the same as that used for normalization (see section 5.2.1.2). High count
acquisitions were simulated for a right cylinder phantom with an activity map
consisting of uniform background (B), hot (H) and cold (C) rod compartments and
attenuation map of solely air or uniform water filled background. Figure 5.4(a)
depicts a schematic of the simulated activity distribution. Concentration ratios
were set at 4.8:1:0 for H:B:C. ACF estimation was performed with the voxelized
water filled attenuation map as input and only true events (those not undergoing
Compton scatter in the phantom) reconstructed. To compare reconstructed images
of the air (ground truth) and water filled phantoms, profiles were drawn and ROI
analysis performed on the rods and background.
5.2.2.4
Scatter.
The accuracy of the scatter and attenuation corrections was assessed using a water
filled cylindrical acrylic phantom containing hot rod (H), cold rod (C), and background compartments (B). Figure 5.4(b) and (c) depict the custom made scatter
phantom which was based on [128] and allows for an asymmetric distribution of
activity both transaxially and axially. The scatter phantom was filled with 0.3
mCi of 18 F-FDG, offset transaxially by 1 cm, and scanned by PET with 20 minute
acquisitions (25 minute duty cycle) for 5 half-lives and by CT (tube voltage=80
kVp, tube current=7.0 mA). The activity concentration ratios were set as follows
H:B:C= 5:1:0. The background compartment was partially filled and the phantom
inverted such that all activity was within the FOV of the scanner. CT images
96
were segmented into regions with linear attenuation coefficients of air, water, and
acrylic and ACF calculated as in section 5.2.1.5. Scatter correction was performed
for a total of 3 iterations on sinograms summed over all acquisitions. For a qualitative assessment of scatter correction accuracy, profiles were drawn through the
rods and background of images reconstructed after FORE with or without scatter
correction as well as the scatter estimate itself. Bias after scatter correction was
estimated by drawing ROI on the rods and background of reconstructed images
and calculating contrast recovery coefficients (CRC) for the cold (CRCcold ) and
hot (CRChot ) rods as follows:
CC
CB
(CH /CB − 1)
=
R−1
CRCcold = 1 −
CRChot
(5.12)
(5.13)
where CC , CH and CB are values for the cold, hot rod, and background ROI,
respectively, and R is the expected activity concentration ratio between the hot
rod and and background compartments.
5.2.2.5
Image uniformity.
Quantification of artefacts induced by normalization and image uniformity after
all corrections was performed with a high count scan of a fillable right cylinder
phantom, as shown in figure 5.3(b). The phantom was centered axially and offset
1.5 cm transaxially in the FOV and scanned by PET with 20 minute acquisitions
(25 minute duty cycle) for a total acquisition time of 20 hours. The phantom was
filled with a total of 13 injection doses to maximize recorded counts and the range
of activity in the phantom (80-320 µCi) during imaging was chosen such that global
singles rates summed for both heads was within the limits observed during patient
97
imaging (see table 5.1). Raw data was fully corrected and reconstructed with FBP
after FORE. Transaxial and axial uniformity was qualitatively assessed by drawing
profiles through the reconstructed images. Image uniformity was estimated by
drawing concentric semi-annular ROI with center of rotation set at the center of
the PET FOV. The angular position and central angle subtended by each semiannular ROI was adjusted such that ROI were entirely within the phantom, as
determined by a larger circular ROI (diameter=6.0 cm) centered transaxially on
the phantom.
5.3
5.3.1
Results
Dead-time and randoms.
Incident event rates, as a function of singles, were estimated on a slice-by-slice
basis from linear fits of values from ROI (diameter = 9.6 cm) drawn on a total of
61 transaxial slices. Images were corrected for both randoms and combinations of
the live-time models in section 5.2.1.3 and linear fitting was done over 6 sequential
acquisitions with singles rates (averaged over detector heads and acquisitions) ≥
minimum observed during patient imaging (table 5.1). Figure 5.5(a) compares
the incident event coincidences (Linear-Fit), averaged over all image slices, with
corrected or uncorrected data as a function of singles. Count-rates for data without randoms or dead-time corrections greatly underestimated incident count-rates.
Figure 5.5(b) assesses the contribution of the individual components in the LT
model in (5.4) to the residual error as a function of singles. When no LTU E correction was applied (w/o LTU E Correction) a maximum residual error of -20.1% was
recorded at a singles rate (457 kcps) approaching the maximum observed during
98
300
Linear Fit
Corrected
Uncorrected
Trues Rates (kcps)
250
200
150
100
50
0
0
100
200
300
400
Average Singles (kcps)
(a)
500
600
500
600
10
5
Difference (%)
0
-5
-10
-15
Corrected
-20
Corrected w/ OFOV Act.
-25
w/o LTUE Correction
-30
0
100
200
300
400
Average Singles (kcps)
(b)
Figure 5.5. Accuracy of dead-time and randoms corrections. (a) Trues and
scatters versus estimate of average energy windowed singles for incident rates
(Linear-Fit), data fully corrected for dead-time and randoms (Corrected), and
data without any corrections (Uncorrected). (b) Residual error between incident
and fully corrected prompts ROI for activity inside the FOV alone (Corrected)
or with additional activity OFOV (Corrected w/ OFOV Act.), or with activity
inside the FOV alone and all corrections except LTU E (w/o LTU E Correction).
Vertical lines indicate approximate range of singles observed during patient
imaging and error bars show min and max differences across the axial FOV.
99
Table 5.2. Mean (over all axial slices) and max RMSE (%) taken over singles
rates observed during patient imaging for various combinations of dead-time
and randoms corrections.
Metric
Uncorrected
Corrected
Corrected
w/ OFOV Act.
w/o LTU E Correction
(Energy related pile-up)
Mean
27.6
2.0
1.3
9.8
Max
30.9
4.9
3.6
14.0
patient imaging, compared with a value of -10.1% at the same singles rate for the
case of full LT correction (Corrected). The accuracy of the LT model for different
activity distributions is also examined in figure 5.5(b). Including activity OFOV
(Corrected w/ OFOV Act.) was found to not increase residual error over the case of
activity in the FOV alone (Corrected). Regardless of the LT correction employed,
or the activity distribution used, the range of residual error values increased as a
function of singles rates due largely to the underestimation of ROI for transaxial
slices at both extremes of the axial FOV. Table 5.2 compares root mean square
error (RMSE) averaged over singles observed during patient imaging. A maximum
RMSE of 4.9% was measured for data fully corrected for dead-time and randoms
versus 30.9% for data with no corrections.
Figure 5.6 shows a ratio histogram of raw to variance reduced randoms that
allows the qualitative assessment of bias due to the variance reduction algorithm.
In the case of no bias the ratio histogram would contain only Poisson noise and
no structure. Several high intensity vertical and horizontal bands are visible due
to crystals with very low efficiency. The COV of all elements in figure 5.6 should
≈ the noise from Poisson statistics alone in the raw randoms set if negligible bias
is introduced by the variance reduction method. Estimated COV for the raw
100
Figure 5.6. Ratio histogram of raw to variance reduced randoms for a scan of
an offset uniformly filled cylinder phantom. Displayed as crystal j + Nr v versus
i + Nr u for clarity (see section 5.2.1).
randoms histogram was 17.2% (average of 34 counts per a bin) and 22.1% for the
ratio histogram, suggesting that some bias is introduced by the 3D Casey and
Hoffman algorithm. Not including columns and rows in the ratio histogram with
sums ≤ 5% the mean (total of 9 bands), reduces the COV of the ratio histogram
to 17.5%. Low frequency bias was estimated by computing the COV of figure 5.6
after smoothing, and was = 2.1%.
5.3.2
Attenuation validation.
Figure 5.7 shows the performance analysis of the calculated attenuation correction
(AC) method. Images were reconstructed after FORE from simulation data with a
variance equivalent of 203 million recorded trues. Line profiles were generated by
averaging voxel intensities from ROI (thickness=3.4 mm, axial depth=51 slices)
101
25
Counts (arb. units)
20
(a)
Counts (arb. units)
80
60
True
w/o AC
w/ AC
40
20
0
-50 -40 -30 -20 -10 0 10 20 30 40 50
Profile Location (mm)
(c)
Difference (%)
100
15
10
True
w/o AC
w/ AC
5
0
-50 -40 -30 -20 -10 0 10 20 30 40 50
Profile Location (mm)
(b)
5
4
3
2
1
0
-1
-2
-3
-4
-5
-50 -40 -30 -20 -10 0 10 20 30 40 50
Profile Location (mm)
(d)
Figure 5.7. Accuracy of attenuation correction as determined through MC simulations. (a) Transaxial reconstructed image of the activity distribution with
an all air attenuation map (True) depicting position of line profiles and circular
ROI. Comparison of transaxial line profiles drawn through the (b) background
and the (c) hot and cold cylinders of the phantom. (d) Percent difference of
background profiles between the True and AC images. Vertical gray lines on
(b)-(d) represent the transaxial extent of the phantom.
drawn through background and cylinder compartments. Profiles for images with
AC (w/ AC) agree well with those taken from reconstructed images of simulations
using an attenuation map solely of air (True), as shown in figure 5.7(b) and (c).
Figure 5.7(d) shows that the difference between the True and AC images for line
102
Table 5.3. ROI measurements of activity concentration (intensity/ml) (mean ±
inter-axial slice σ) from true and attenuation corrected (AC) cylinder phantom
images.
Method
Hot Rod
Cold Rod
Background
True (Air attenuation map)
33.30 ± 0.37
−0.13 ± 0.15
6.82 ± 0.04
w/ AC
33.53 ± 0.36
−0.14 ± 0.16
6.87 ± 0.06
profiles of the background segment was a maximum of -3.2% at the edge of the
transaxial extent of the phantom, with RMSE over the complete extent of the
phantom measured at 1.3%. Table 5.3 shows the activity concentration calculated
from 10 mm diameter ROI drawn on a total of 51 transaxial slices for AC and
True images for the hot rod, cold rod, and background regions. The difference
between AC and True ROI mean values was less than 4% of the background for
all compartments.
5.3.3
Scatter.
Figure 5.8 shows the performance of the MC based scatter correction on high
count data (total prompts = 174 million) acquired from a phantom with asymmetric activity distribution. For the scatter correction, radial blurring of the scatter sinogram was performed with a Gaussian with FWHM = 22.9 mm, and the
desired COV of the blurred scatter sinogram with respect to the experimental
data (f ) set to 0.25 (see (5.10)). Figure 5.8(a) shows 1.7 mm thick line profiles
drawn through the center of hot and cold rod compartments for data corrected
or uncorrected for scatter, and the MC scatter estimate itself (ˆ
suivjθ ). Agreement
between sˆuivjθ and the cold regions of the phantom for the image without scatter
correction is excellent. A qualitative decrease in cold rod compartment residue
103
Counts (arb. units)
100
w/o SC
MC S
w/ SC
80
60
(b)
40
20
0
-60
-40
-20
0
20
40
Profile Location (mm)
(a)
60
(c)
Figure 5.8. Scatter correction performance for experimental scans of a phantom with asymmetric activity. (a) Comparison of transaxial line profiles drawn
through the cold and hot cylinders for reconstructed images with (w/ SC) or
without (w/o SC) scatter correction, and the MC scatter estimate itself (MC S)
after two iterations of scatter estimation. (b) Reconstructed transaxial images
without scatter correction and (c) with scatter correction, with display window
upper limit = 35% of maximum. Profiles and images were averaged over 30
axial slices.
is visible in reconstructed transaxial images, as shown in figures 5.8(b) and (c).
Table 5.4 lists the cold (CRCcold ) and hot (CRChot ) CRC values for images with
or without scatter correction, and as a function of the scatter estimate iteration
number. Values were estimated from 3.4 mm diameter ROI, with 1 each on the
cold and hot rod compartments and 6 arranged on the background, over a total
of 30 transaxial slices. Scatter correction significantly improved both CRCcold and
CRChot , although residual error was larger for the hot rod compartment. Contrast
recovery was optimal after a total of 2 iterations for the scatter estimate, although
not significantly compared to results after 1 iteration. Figure 5.9 shows CRCcold
as a function of transaxial slice number. Values were estimated as in table 5.4
104
Table 5.4. Contrast recovery coefficients (CRC)(%) (mean ± inter-transaxial
slice σ) for images of an asymmetric activity distribution with or without scatter
correction.
Method
CRCcold
CRChot
w/o SC
76.2 ± 2.9
72.1 ± 2.8
w/ SC, iteration 1
97.3 ± 3.0
90.4 ± 2.7
w/ SC, iteration 2
98.3 ± 3.2
91.7 ± 2.9
w/ SC, iteration 3
97.1 ± 2.9
90.5 ± 2.7
110
CRCcold (%)
100
90
80
70
60
w/ SC
w/o SC
0
20
40
Transaxial Slice Number
60
Figure 5.9. Mean CRCcold as a function of transaxial slice number taken over
the entire length of the cold compartment for a phantom containing asymmetric
activity distribution. Results are for images reconstructed with all corrections
excluding (w/o SC) or including (w/ SC) scatter correction. The 60th axial
slice represents the approximate edge of the cold rod compartment and the
warm background.
but the number of transaxial slices examined was extended to cover the complete
cold rod compartment. Average CRCcold across this extended axial range was
95.2 ± 4.8%, with a trend of decreasing contrast recovery for transaxial slices closer
to the boundary seperating the cold rod and uniformly filled compartments.
105
(a)
(b)
(c)
Figure 5.10. Transaxial images of a uniformly filled phantom from a high count
scan. All images were corrected for LT, attenuation, randoms, and scatter. (a)
Images with no normalization applied, (b) geometric (Ωuivj ) normalization only,
and (c) both Ωuivj and detector efficiencies (εui εvj ) applied. Top row: gray scale
windowing set to the full dynamic range. Bottom row: gray scale minimum set
to 70% the image maximum.
5.3.4
Image uniformity.
Reconstructed images for a high count acquisition (total prompts = 1.8 billion)
of a uniformly filled phantom are shown in figure 5.10. The images are an average of 41 axial slices and were processed with different levels of normalization.
Qualitatively, normalization for detector efficiency factors (εui εvj ) (figure 5.10(c))
was found to significantly improve image uniformity over correction for geometric efficiencies (Ωuivj ) alone (figure 5.10(b)), with reference to the instance of no
normalization (figure 5.10(a)). The range of εui εvj was 0.06-2.58 versus 0.64-1.09
for Ωuivj . After all corrections were applied a low frequency, low magnitude, con-
106
10
10
5
Difference (%)
Difference (%)
5
0
-5
Max
Mean
Min
-10
-15
Max
Mean
Min
0
10
20
30
Annular Radius (mm)
(a)
0
-5
-10
40
-15
20
30
40
50
Transaxial Slice Number
(b)
Figure 5.11. Assessment of image uniformity after all corrections for a uniformly
filled phantom. (a) Difference of mean annular ROI values, with respect to the
volume mean, taken across the transaxial FOV. Min and max represent mean
ROI values at a given radius across all images slices, and the CFOV is at an
annular radius = 0. (b) Mean of all voxels covered by annular ROI on a sliceby-slice basis. Min and max are mean annular ROI values across the transaxial
image plane for a given axial slice.
centric ring and cold spot artefact, with center at the CFOV, were visible. To
quantify the magnitude of the ring artefact on transaxial and axial uniformity a
total of 8 concentric semi-annular ROI (ring thickness= 5 mm), centered at the
CFOV, were drawn on transaxial images. Figure 5.11(a) shows that ROI bias, with
respect to the volume mean, was the greatest absolute magnitude (-10.2%) closest
to the CFOV. The change in the annular ROI values as a function of transaxial
slice number is depicted in figure 5.11(b). The difference of the ROI at the CFOV
with respect to the volume mean was found to increase at larger transaxial slice
numbers. Mean RMSE across all transaxial slices was 2.5%. A further analysis of
the ring artefacts was performed by drawing 3.4 mm thick line profiles vertically
through the transaxial CFOV at several transaxial slice positions, as shown in figure 5.12. Consistent with the annular ROI results in figure 5.11(b) the cold spot
60
107
30
Counts (arb. units)
25
20
15
10
Mean
Slice 25
Slice 50
5
0
-30 -20 -10 0 10 20 30 40 50 60
Profile Location (mm)
Figure 5.12. Comparison of transaxial line profiles drawn through reconstructed
images of a uniform cylinder after all corrections. Profiles shown include an average taken over 41 slices (Mean), and at two different transaxial slice numbers.
The transaxial CFOV is at a profile location of 0. Slice numbers correspond to
those in figure 5.11(b).
artefact at the CFOV increases with respect to the volume mean at several higher
transaxial slice numbers. The line profiles in figure 5.12 also show, qualitatively,
the experimental accuracy of the attenuation correction method. Artefacts characteristic of displacement or dimension mismatches between the true and assumed
attenuation media are visible [129].
5.4
Discussion
The performance of multi-component LT and variance reduced randoms corrections was assessed as a function of singles rates and source distributions. RMSE
measured over singles rates observed during patient imaging was found to not increase with the addition of activity placed OFOV (table 5.2). This finding suggests
that the relationship between counter based singles rates (S1c and S2c ) and energy related pile-up losses, as estimated by LTU E , is not sensitive to the source
distribution. The range of residual errors over the axial length of the phantom
108
were found to increase significantly as a function of the singles rate (figure 5.5(b)),
due largely to the deficit in ROI values at the axial extremes of the FOV. Pile-up
effects have been shown to preferentially misposition events towards the center
of the detector block in a count-rate dependent manner [130]. The multiplexed
large area detector readout used in DbPET/CT, in combination with acquisition
electronics that lack pile-up prevention circuitry, makes this system particularly
susceptible to such pile-up effects.
For compatibility with the MC scatter estimation a segmentation based attenuation correction was used in the analysis presented here. However, for patient imaging there is no technical reason why a scaling approach [42], in which Hounsfield
units (HU) are directly converted to µ511keV , could not be employed. Scaling methods have been shown to have reduced accuracy when using contrast-enhanced CT,
and preliminary results suggest that breast CT with contrast-enhancement may
offer superior detection of smaller in situ lesions compared to breast CT without
contrast, and may offer equivalent diagnostic information to contrast-enhanced
MRI [92]. Inaccuracies in ACF estimation due to contrast, however, are most severe for thoracic imaging and have not been shown to be significant for regions
imaged elsewhere in the body, such as the breast [131]. A limitation when using the CT for attenuation correction, regardless of the method, is the potential
spatial mismatch between PET and CT images. Accuracy of ACF estimation has
been shown to be most sensitive to inaccurate registration between emission and
attenuation maps [129]. For a clinical trial of 4 patients with DbPET/CT, in
which no immobilization of the breast was used, one set of PET images was not
109
interpretable due to misregistration between the PET and CT [118]. Segmenting
the reconstructed PET volume instead of the CT implicitly reduces this problem,
however mild compression of the breast is another potential solution and we plan
on implementing an immobilization scheme in the near future. Furthermore, it
is expected that the larger transaxial FOV (20 vs. 12 cm) and the significantly
higher SNR of images from the CT compared with the PET, will allow for more
accurate segmentation of the breast volume for DbPET/CT.
Performance of a MC based scatter correction method was explored for data
acquired from a phantom with asymmetric activity distribution. Both CRCcold
and CRChot mean residual error were <9% after 2 iterations, with CRChot underestimation significantly greater than CRCcold . Studies using an alternative MC
implementation [132] and a single-scatter simulation (SSS) approach [133] with
similar phantoms have measured comparable residual error, although not necessarily biased towards increased CRChot . Possible explanations for the CRChot
underestimation measured in this study include the partial voluming of the acrylic
hot rod compartment wall, lack of position-dependent energy resolution modeling
for blocks in the MC simulation, pile-up induced spatial redistribution of events,
and the presence of residual error from the randoms correction. Additionally we
noticed a trend of decreased CRCcold as a function of transaxial slice number. This
downard trend was not significantly changed by the size or placement of the cold
cylinder ROIs or choice of background ROIs in the CRCcold calculation, and its
ultimate cause is unkown. We note, however, that CRCcold averaged over the full
length of the cold cylinder was ≤ to values from the literature [132, 133].
110
The scatter estimation code used here has not been fully optimized for computation time. Using the COV scaling approach (see section 5.2.1.6) with f =0.1,
for a 12.5 minute patient breast scan, time per iteration on a cluster with 2.7 GHz
Core2 Duo Processors (Intel Corporation, Santa Clare, CA) was ≈11 minutes,
with <1 minute of overhead to condtion data before iterating. We have used importance sampling techniques [134] to improve MC simulation efficiency, although
we expect computation time to be further reduced with coarser attenuation map
sampling and parallelization of acquisitions in the simulation environment itself.
Although we chose a MC implementation, the optimal scatter correction for
bPET imaging requires further study. The large fraction of the PET FOV occupied
by the breast might significantly limit the accuracy of tail fitting approaches [40]
and the performance of dual energy window methods [128] could be reduced by the
relatively low energy resolution (25%) of DbPET/CT and the large range of breast
dimensions [118]. A known limitation of MC and SSS methods is an inability to
account for activity from OFOV that is not directly imaged by both PET and
CT. The scanner and prone patient positioning geometry used in DbPET/CT
inherently limits the ability to acquire emission measurements for tissue outside of
the breast, and OFOV activity was not accounted for in this MC implementation.
Simulation studies, however, have revealed that the contribution to the total SF
from OFOV activity is expected to be negligible [38].
Several artefacts were evident in images of a uniform cylinder even after normalization for geometric and detector efficiency factors. Most visible was a low
magnitude concentric ring pattern (figure 5.10), which has been noted previously
111
[135, 136]. For a rotating dual-head PET system Conti et al [137] found this
type of artefact to be significantly reduced in both the transaxial and axial directions by using count-rate-matched normalization coefficients. Average singles
rates for the phantom scans used in detector efficiency calculation and estimation
of image uniformity were 92 kcps (average dead-time=11%) and 285 kcps (average dead-time=38%), respectively, indicating that inadequate count-rate-matching
may have been a degrading factor. The mispositioning of events due to pile-up was
suspected in the axial direction for the performance assessment of dead-time and
randoms corrections, and may explain the concentric ring pattern observed here.
A cold spot at the transaxial CFOV was also observed. For FBP the CFOV is the
most sensitive transaxial position to systematic errors between the estimated and
actual normalization coefficients. The MC estimated geometric efficiency factors
(Ωuivj ) used here were not corrected with experimental measurements for potential
systematic differences with actual Ωuivj factors, as in [138], potentially contributing
to this artefact.
112
Chapter 6
Monte Carlo Simulation Design
Study of bPET System
Geometries
6.1
Introduction
The high out of field of view (FOV) activity and relatively low tumor to background
uptake ratio associated with
18
F-FDG dedicated breast PET imaging mandate a
system that has a high geometrical sensitivity to trues, while at the same time
being optimized for the wide variability in patient breast size [77, 139]. Results
from patient imaging and MC simulations [139] have revealed that NECR with a
variance reduced randoms estimate range from 100-1500 cps. The combination of
improved solid angle and electronics, with lower susceptibility to dead-time, are
expected to significantly improve NECR values. In this study we use Monte Carlo
simulations to explore the performance of a range of detector geometries for the
PET component of a dedicated breast PET/CT system imaging anthropomorphic
models possessing different breast sizes. Performance is assessed with NECR [55]
and scatter fraction estimates. This work was presented by Bowen et al. [140].
A
120 mm
113
C
B
206 mm
12
0m
180 mm
m
180 mm
E
D
210 m
m
120 mm
206 mm
167 mm
Figure 6.1. Schematics of the scanner geometries simulated. Systems included
a (A) planar dual-head, (B) cylindrical, (C) split-ring, (D) five-sided box, and
(E) DOI capable cylindrical cameras.
6.2
6.2.1
Materials and methods
Scanner Models
The LSO detector for our current prototype system has a 9x9 array of 3 mm x 3
mm x 20 mm crystals, and is coupled to a position-sensitive photomultiplier tube
(PS-PMT) via a tapered fiber light guide [93]. A simplified version of this detector
block unit (not including a PMT and containing a box shaped vs. tapered light
guide) was modeled and used to compose the following geometries: cylindrical (22
detectors per ring and 6 detectors axially), split-ring (7 detectors transaxially per
a head, having the same radius of curvature as the cylindrical system), five-sided
box (4 sectors of 4 axial x 7 transaxial detector blocks each and a bottom sector
of 7x7 blocks), and a planar dual-head system geometrically similar to the current
prototype (4x4 detectors per head) (see figure 6.1(A) through (D)). The separation
distance between the heads of both the split-ring and planar dual-head system were
114
Gantry
Brain
NCAT
Bladder
Breast
PET Camera
Figure 6.2. Complete geometrical simulation model. The anthropomorphic
phantom is composed of the brain, bladder, NCAT, and breast volumes.
S
M
50 mm
L
Figure 6.3. Overlay of sagittal slices for the small (S), medium (M), and large
(L), sized breasts. The red line denotes the beginning of the axial FOV for all
scanners.
varied according to the breast size simulated.
An additional scanner type based on the cylindrical geometry, but with different detector units capable of depth of interaction (DOI) measurements, was also
modeled. The detector unit, currently being tested in our lab, implements a dual
ended read-out scheme with a 14 mm x 14 mm avalanche photodiode (APD) in
front and a single channel PMT in the rear of an LSO block (9x9 array of 1.5 mm
115
Table 6.1. Volume of digital breast phantoms
Breast Size
Volume in PET FOV (cm3 )
large
707.4
medium
562.6
small
27.4
x 1.5 mm x 20 mm crystals with a pitch of 1.57 mm). From these detectors we
obtained a DOI resolution of 3.7 mm, timing resolution of 2.2 nsec, and energy
resolution of 13.6% at 511 keV. The simulated detectors only contained the LSO
block and 80 mm thick section of Plexiglas, representative of the PMT coupled to
the back. The modeled camera consisted of 38 detectors per a ring and 10 axially,
with an axial modular pitch of 17 mm (figure 6.1(E)). Scanner geometries were
inserted in a simplified PET/CT gantry. Gantry elements included reflect those
that contribute significantly to recorded counts, which are limited to the patient
bed and supporting steel side walls (Fig. 2).
6.2.2
Patient Phantom
The anthropomorphic model consisted of the NCAT phantom [141] with one of
3 volumes representing the breast appended to the left chest wall (figure 6.2).
The breast phantoms themselves were selected from 69 dedicated breast CT image
sets, and were chosen to represent the range of volumes and dimensions observed
in this sample population (figure 6.3). These breast phantoms were deemed large,
medium, and small according to their relative volume in the PET scanner FOV
(table 6.1). Additionally, a cylinder and sphere were added to represent the brain
and bladder, respectively (figure 6.2). For consistency with previous work [139],
116
the distance from the base of the breast model to the top of the field of view was
set to 2 cm.
18
F-FDG uptake in the torso phantom was assumed normal and set to values
measured by Ramos et al. [142]. In particular, the activity concentration ratio
of muscle:breast:brain:bladder was placed at 1:1:5:20. Total activity concentration
was equivalent to an injected activity range of 2 to 30 mCi, assuming a patient
mass of 70 kg with 20% tracer excretion and a 1 hour uptake period. For the DOI
scanner, an additional injected activity of 55 mCi was simulated to explore the
possibility of utilizing short-lived tracers for blood flow imaging.
6.2.3
Simulated System Parameters
System parameters were the same for all geometries, except the DOI capable system, and assumed a global energy resolution of 25% at 511 keV, with readout at
the block level. Singles events were passed through a trigger value of 120 keV,
representing that of the CFD, before being exposed to the front-end dead-time
(paralysable, characteristic time = 256 ns). A system-wide lower energy level discriminator (LLD) of 350 keV was implemented. The coincidence time window
was set to 2τ = 7.5 ns, and coincidence dead-time was applied (non-paralysable,
characteristic time = 256 ns). An upper energy level discriminator (ULD) of 650
keV was imposed in post-processing. These parameters were derived from those
we considered practical if Siemens HRRT acquisition electronics were implemented
with readout at the block level.
The DOI capable system used the same general processing scheme as the other
systems, only with a modified energy resolution of 14% at 511 keV, a paralyzable
117
dead-time of 160 nsec and non-paralyzable dead-time of 100 nsec, an LLD of 450
keV, and a coincidence window of 6 nsec. Additionally, the ULD was set to 620
keV. These parameters were derived from those we considered practical if Siemens
Cardinal acquisition electronics were implemented with readout at the block level.
The DOI capable system as a whole represents a practical implementation of the
cylindrical scanner with state of the art detector modules and electronics. All
detectors were assumed to have perfect timing resolution and uniform detector
efficiencies.
6.2.4
Simulation Parameters and Data Processing
Monte Carlo simulations were performed using GATE [110]. Sources were modeled
as back-to-back 511 keV photons with positron range and acollinearity neglected.
Rayleigh scattering, secondary electrons, x-rays, and delta-rays were also not considered. Data was processed via ROOT (CERN open source software for processing
GATE data) and Matlab (the Mathworks, Natick, MA). For calculations, singles
were deemed only those events qualified by the CFD trigger. Random and scatter rates were calculated solely for events with LORs passing through the breast
phantom and NEC rates were calculated via the 1R formulation (i.e., assuming
the availability of a low-variance estimate for random coincidences). Rates were
plotted as a function of injected activity.
6.3
6.3.1
Results
Comparison of NEC Rates for All Scanners
Figure 6.4 shows NEC rates as a function of injected activity for all non-DOI
scanner types when imaging the medium sized breast. For injection activities > 5
118
NEC Rate (kcps)
50
Cylindrical
Split-Ring
Five-Sided Box
Planar Dual-Head
40
30
20
10
0
0
5
10
15
20
25
30
35
Injected Activity (mCi)
Figure 6.4. NEC rates versus injected activity for the 4 geometries considered
when imaging the medium sized breast phantom. The vertical line indicates 20
mCi injected dose (typical for 18 F-FDG imaging). Head separation distances
for the split-ring and planar dual-head geometries were 159 mm and 147 mm,
respectively.
Table 6.2. Simulated NEC rates and scatter fractions for several geometries
Geometry
NEC (kcps) at 20 mCi
Scatter Fraction (%)
Cylindrical
32.4
28
Split-Ring
26.7
28
Five-Sided Box
27.3
25
Planar Dual-Head
10.5
24
Results are for the medium breast phantom.
mCi the cylindrical scanner produced higher NEC rates than the other geometries.
For instance, at an injection activity of 20 mCi the cylindrical scanner gave an
NEC rate more than 3 times that of the planar dual-head scanner, at the cost of
only a slight increase in the system scatter fraction (table 6.2). In general, scatter
fractions across all systems were comparable. The NEC rates for the five-sided
box scanner were lower than the cylindrical scanner even though it has a higher
effective solid angle. This result is attributed to the high singles flux from outside
119
60
Cylindrical
DOI Scanner
Current Prototype
NEC rate (kcps)
50
40
30
20
10
0
0
10
20
30
40
50
60
Injecte d Activity (mCi)
Figure 6.5. NEC rates versus injected activity for the cylindrical (without DOI
capabilities), DOI scanner (cylindrical geometry), and current planar dual-head
prototype, with the medium breast phantom. The DOI scanner does not show
peak NEC rates even at injected values > 50 mCi.
the FOV on the bottom sector and the small percentage of LORs between the
bottom and side sectors intersecting the breast.
Figure 6.5 shows NEC rates for the non-DOI cylindrical scanner, the DOI
capable scanner, and our current prototype (the dual planar system with readout at
the detector head level and PCI-based acquisition electronics). System parameters
for the prototype are given by Lamare et al. [139]. It can be seen that at 20 mCi
injected dose, the cylindrical scanner generates an NEC of 32 kcps, compared to 21
kcps for the DOI scanner (figure 6.5). This difference can be accounted for largely
by the reduced overall packing fraction of the DOI vs. the non-DOI cylindrical
scanner. The DOI design with the fast electronics still has rising NEC at an
injected dose of 55 mCi, a value appropriate for imaging of short-lived isotopes
for blood-flow imaging (figure 6.5). The scatter fraction for the DOI scanner was
found to be just 13%. This is explained by the good energy resolution and high
120
70
60
NEC rate (kcps)
1.0
Large
Medium
Small
Small
0.8
50
0.6
40
30
0.4
20
0.2
10
0
0.0
0
5
10
15
20
25
Injecte d Activity (mCi)
30
35
0
5
10
15
20
25
30
Injected Activity (mCi)
Figure 6.6. NEC rates versus injected activity for the cylindrical scanner imaging several breast sizes. Results for the small, medium, and large sized breast
volumes (left). Magnified NEC rates axis for the small sized breast volume
(right).
Table 6.3. Simulated NEC rates for cylindrical scanner with different breast
sizes
Breast Size
NEC (kcps) at 20 mCi
NEC density (cps/cm3 ) at 20 mCi
large
49.8
70.5
medium
32.4
57.6
small
0.3
9.8
LLD.
6.3.2
Comparison of NEC Rates for the Cylindrical Scanner with Different Breast Sizes
Figure 6.6 shows NEC rate curves for the different breast phantoms imaged on
the non-DOI cylindrical scanner. NEC rates for the small breast phantom were
much lower than either those of the medium or large breast even when normalizing
by volume in the FOV (figure 6.6) (table 6.3). This may be explained for by the
relatively low sensitivity of the scanner at the edge of the FOV.
35
121
A
B
Figure 6.7. Maximum intensity projections from the same view of 3D histograms
representing the actual activity distribution (A) and the origin of received singles
(B) from the anthropomorphic phantom. Images were normalized by the total
number of counts.
The increased volume and axial extent of the large breast relative to the medium
breast led to an increase in the NEC rate by 60% at an injection activity of 20
mCi (table 6.3). More specifically, the trues rates increased significantly for the
large breast vs. the medium breast while the scatter and random rates did not
(data not shown). Scatter fraction for these two breast sizes were both 0.28. This
similarity is accounted for by a negligible difference in the average coronal cross
sectional area within the FOV between the medium and large breast phantoms.
6.3.3
Impact of Activity from Outside the Field of View
To better understand the contribution of activity from outside the FOV on random and single event rates, 3D histograms of the origin of detected singles were
generated for the different scanners. Figure 6.7 shows maximum intensity projection images of the activity distribution and the singles histogram for the cylin-
122
drical scanner. The histograms were quite similar for the cylindrical, box and
split-ring geometries (the DOI and planar dual-head systems were not assessed).
The singles contributions from the heart and stomach were most significant, but
detected counts from the brain and bladder were also non-negligible. These results are due to the relatively high uptake ratio of these organs with respect to
the background of the muscle (activity concentration ratio is 1:6:3 for the muscle:myocardium:stomach).
6.4
Discussion and Conclusion
The cylindrical scanner out-performed the unconventional designs in terms of NEC,
but we note that the difference between NEC rates at 20 mCi between the cylindrical and split-ring geometries may not, on its own, justify the larger number
of detectors required; however, there are other advantages to a cylindrical design
that cannot be assessed using NEC. In particular, the process of normalization for
cylindrical scanners is well understood, and the circular symmetry permits practical protocols for direct measurements of the system response matrix, which has
been shown to improve spatial resolution [143, 144].
Our results show that breast scanners can achieve similar NEC rates to wholebody scanners, and with appropriate electronics, it should be possible to image
at 55 mCi injected dose - enough to use short-lived radioisotopes for blood-flow
imaging. The DOI scanner geometry investigated substantially out-performs the
current prototype system in terms of NEC, and offers the promise of significant
advantages in terms of spatial resolution. However, our data suggest that efforts
to improve packing fraction are likely to be worthwhile.
123
In contrast to whole-body imaging, we found that in our sample, NEC increased
with increasing breast volume. Singles to trues ratio (STR) results from patient
imaging (see section 4.3.2) suggest a similar trend. More research is required
however, to determine what if any relationship exists between breast volume and
NEC rates for the general population. NEC is low for the smallest breast, even
after normalizing for volume in the field of view. In practice we hope to bring the
field of view closer to the chest wall, but small breasts and imaging close to the
chest wall in larger breasts will remain difficult with the pendant configuration.
The distribution of singles sources in our anthropomorphic model suggest that
standard oncology preparation for whole-body
18
F-FDG-PET imaging (fasting to
reduce cardiac uptake and voiding prior to scanning) is also likely to be useful in
dedicated
18
F-FDG-PET imaging of the breast.
124
Chapter 7
Future Directions
7.1
Improvements in Data Corrections and Quantification
7.1.1
Minimizing the Effects of the Limited PET Transaxial FOV
Patient imaging results have demonstrated that the transaxial FOV of the PET
component (12 cm) for DbPET/CT is significantly less than the maximum expected breast diameter (18.1 cm) (see table 5.1). The limited transaxial FOV can
lead to an inability to image the full volume of the breast and can induce artifacts
in the reconstructed images (see section 4.3.1). This limitation of DbPET/CT is
most significant at axial positions close to the chest wall. The breast positioning
system described in section 2.5 aids in accurately positioning the subject’s breast
in the CFOV, thereby limiting OFOV tissue, but methods of physically extending
the PET transaxial FOV are expected to have a more significant impact on image
quality.
Figure 7.1 depicts a method to extend the FOV, by laterally translating the
PET heads from the center (centerline). Advantages of this approach are that it
125
A
B
3.2 cm
Figure 7.1. Method to increase the transaxial FOV for the PET component of
DbPET/CT. (A) Transaxial viewpoint showing original (dashed) and 3.2 cm
offset centerline (solid). (B) View from the front of a detector head.
requires no new detectors and is mechanically straightforward, but at the cost of
a 360◦ rotation to meet the criteria for fully tomographic sampling and reduced
symmetries in the system matrix. An early WB PET system [145] utilized such an
offset detector geometry. An alternative method would be to change the detector
configuration from 4x4 to 2x8, with 8 detector modules placed radially, effectively
doubling the transaxial FOV. This second approach, however, would require extensive machining and reduce the axial FOV by one half.
7.1.2
Attenuation Correction
In chapter 5 a calculated attenuation correction method using a segmented CT
image with a uniform linear attenuation coefficient was validated. We used a
segmentation method instead of a scaling approach [42] due to its straightforward
integration with the MC based scatter correction (only a discrete set of materials
can be specified in the MC model) and unknown influence of contrast-enhanced
CT scanning on HU based µ511keV map estimation (see section 5.4). An area of
study yet to be addressed with this method is determination of the optimal linear
126
attenuation coefficient and how and if µ511keV should be varied as a function of
breast composition. For example, the µ511keV values for adipose and fibroglandular
tissue are significantly different (0.091 versus 0.103 cm−1 ), based on the bilinear
scaling approach [42] and recent results from Yaffe et al. [146]. Additionally, the
volume fraction of fibroglandular tissue in the breast has a broad distribution in
the patient population, with the mean breast density (including the skin) measured
at 19.3% in a recent study [146]. Assuming a µ511keV =0.093 cm−1 for the average
breast density, an understimation in attenuation of >7% would occur for LORs
passing through an 18 cm breast if the patient being imaged actually had a breast
density =50% (∼ the upper breast density estimated in [146]). For DbPET/CT
µ511keV could be adjusted based on breast density, as estimated from the CT, if
signficant bias results in using a constant coefficient. Additionally, a histogrambased, two means clustering algorithm has been used previously to segment adipose
and fibroglandular tissue, which would allow for exact assignment of the µ511keV
for these tissues in the calculated attenuation correction method.
7.2
Studies to Estimate the Influence of Patient
Related Factors on Quantification
7.2.1
Measuring Breast Motion
Due to the relatively long acquisition time of typical PET scans compared to
the time course of several physiological processes, including respiration and the
cardiac cycle, reconstructed images for ungated PET imaging represent the spatial
and temporal average of the activity distribution of structures involved in such
processes. Cumulative patient motion has been found to increase as a function of
127
time in brain imaging largely from a drift in head position [49]. Motion effectively
degrades reconstructed spatial resolution and contrast and has been found to be
particularly degrading for imaging organs near or in the thoracic cavity with WB
PET (see section 1.5.4). Additionally, when displacement has occurred between
the PET and CT scans for a dual-modality system correction for attenuation can
produce significant image artifacts. Findings from gadolinium-enhanced dynamic
MR breast imaging studies [53] have shown that imaging the patient in the prone
position (versus supine), as has been done with DbPET/CT, acts to reduce breast
motion, however, a large degree of both rigid and non-rigid motion still remains.
As no immobilization of the breast has been used in prior DbPET/CT studies
and motion between the PET and CT components has been noted to reduce image
interpretation in one patient (see chapter 4) we propose quantifying the degradation in performance due to movement of the breast during DbPET/CT patient
imaging. The goal of this proposed study is to construct a system to measure
breast motion in a patient trial, recreate the motion via a phantom, and quantify
the effect of this motion on image quality.
Motion tracking will be performed using an optical computational stereo vision motion capture system (MoCap). In MoCap two or more cameras imaging
the same field of view acquire video of specialized retro-reflective targets. The 2D
coordinates of these targets, as seen in the reference frame of the cameras, can
be converted to 3D positions using stereo triangulation. MoCap systems can be
purchased commercially and the desired system must meet the following specifications: acquisition rate of >= 20 Hz, small foot-print, sensitivity to near infrared
128
(near-IR) light band (700-1400 nm), and spatial resolution significantly higher than
the reconstructed PET resolution (∼ 3.3 mm). For optimal accuracy MoCap systems require calibration for camera position and lens distortion and we propose
using the method proposed by Bouguet et al. [147]. Comparable MoCap systems
have achieved accuracies and stability of less than 200 µm (RMSE), and 30 µm
(max error), respectively [148]. The system will be positioned in the CT gantry
with cameras focused on isocenter. Accuracy and stability of the system will be
quantified as in [148].
Using the MoCap system the magnitude, frequency, direction, and type of
breast motion will be quantified by tracking breast position in a patient trial as a
function of time for typical scan durations. For a total of 10 healthy female volunteers, each subject will be positioned on the scanner bed and a nuclear medicine
technician will attach 3 retro-reflective markers to the subject’s breast at the central portion, upper outer, and lower outer quadrants of the breast. This arrangement of targets is chosen in order to maximize the detection of deformable motion.
After proper positioning of the subject, MoCap video will be acquired continuously,
start to end, for a duration of 20 minutes. To reveal how the spatial distribution
of positions changes with increased acquisition time, change in translation data for
all degree of freedom (DOF) will be binned into 1 minute segments on a subject
by subject basis. The standard deviation of these bins will be calculated, and the
mean along with error of these standard deviations plotted as a function of time. A
cumulative change in position distribution with time will be generated by summing
standard deviation bins (e.g. 0-1, then 0-2 minutes, etc), and then computing the
129
mean and error. To quantify deformable motion a similar method will be used as
described above, although using the change in marker separation distance instead
of positional changes. The magnitude, frequency, and direction of breast motion
for subjects imaged in the prone position has not been quantitatively assessed as
to date, however, in a study with DCE-MR, Hayton et al. [53] postulated that
translation in the patient’s transaxial plane should be much more frequent than
inferior-superior movements due to the frictional restraints of the patient bed.
The influence of breast motion on image contrast and effective spatial resolution will be quantified through phantom studies based on the results from the
patient trial. Although the overall breast motion is predicted to be largely deformable, local regions of the breast can be modeled as rigid structures. To this
end, a computer-controlled 2D linear stage coupled to a breast phantom will be
implemented to approximate translations along the two axes where breast motion
is most significant. A uniformly filled cylinder phantom, containing higher contrast spheres with diameters of 1.0-2.0 cm, will be attached to the linear stage and
moved in a sequence approximating the motion observed in the patient trial. The
in motion phantom will be scanned by PET at several acquisition times and at
the time-averaged position for the control case. Raw emission data will be fully
corrected (see chapter 5), reconstruction by MAP, and analyzed with ROI analysis
to compute contrast recovery coefficients as in section 5.2.2.4. To assess spatial
resolution degradation radial, tangential, and axial profiles will be drawn through
the center of each sphere, and the standard deviation of these profiles calculated.
The contrast recovery coefficients are expected to decrease with the moving phan-
130
tom compared with the static case. Nehmeh et al. [51] demonstrated that for
imaging lesions in the lung with PET, SUV changes between gated and ungated
cases ranged from 8-160%. The changes in contrast in this study are not expected
to be as large due to the lower magnitude and frequency of patient breast motion.
The effective spatial resolution is also expected to be less than that measured in
the static case.
7.2.2
Optimizing
18
F-FDG Injection Dose
Using an anthropomorphic torso phantom, with a single cylinder phantom representing the breast, we previously estimated that optimal
18
F-FDG injection is ∼3
mCi for patient imaging with DbPET/CT (see section 3.3.3). Patient trial results
and MC simulations, however have suggested that NECR varies significantly as a
function of breast volume for patient imaging (see chapters 4 and 6) such that the
prior anthropomorphic torso phantom experiment may have limited applicability.
As NECR is proportional to the square of image SNR, for a given acquisition
time and patient, the injection activity administered will influence image quality
and radiation dose delivered to the patient (see section 1.6.1). Previous results
with WB PET [57] have found that optimal 18 F-FDG injection dose does not vary
significantly with patient weight, although peak NECR decreases significantly for
larger subjects. No comparable analysis has been performed for PEM or bPET
imaging. We propose to determine optimal injection dose and acquisition time for
18
F-FDG DbPET/CT imaging as a function of patient habitus using the methods
of Watson et al. [57].
The Watson model is capable of estimating continuous NECR curves as a func-
131
tion of injection activity on an individual patient basis. As generating NECR
curves as a function of activity for patients would not be practical, coincidence
curves from phantom acquisitions are scaled to match individual patient values at
a given singles rate. Simple scaling is justified from the finding that for a given
general activity distribution (e.g. brain scanning), coincidence rates are a function
of the singles rates. Furthermore, the singles rate is related to activity in the FOV.
Calculating patient NECR curves first involves measurement of trues + scatters
and randoms rates from a decay experiment. Analytical expressions, termed model
functions, are then derived from fitting polynomials to plots of coincidence rates
versus singles.
To validate the Watson model for DbPET/CT patient imaging and obtain
model functions we will use the previously implemented anthropomorphic torso
phantom with a cylinder representing the breast (see section 3.2.3). The phantom
will be filled with 18 F-FDG such that the activity concentration ratio of the organs
will approximate that seen in WB PET
18
F-FDG scans. Additionally, we will use
two breast phantom cylinders representing the medium and large breast sizes. For
imaging, the phantom will be placed on the gantry, fitted with a breast phantom,
and scanned tomographically for several half-lives. The rate of randoms can be
calculated directly from the delayed coincidence acquisition, the trues + scatters
rate will be estimated by subtracting randoms from DAQ acquired prompts (see
section 5.2.1.4), and scatter rates will be calculated using the MC scatter estimate
(see section 5.2.1.6). In order to only include counts with LORs passing through
the breast phantom, a mask will be created from the CT derived attenuation co-
132
efficients (see section 4.2.2). In order to produce model functions, trues + scatters
and randoms rates versus singles will be fitted with 3rd order polynomials. In addition, the total activity in the phantom as a function of singles will also be fitted.
By calculating the rate of trues, NECR curves can be produced as a function of
total phantom activity for each breast size. The model functions from the small
breast, will be scaled to match trues + scatters and randoms rates from a single
time point of the large breast. The degree of correlation between these estimated
and true NECR curves will be quantified.
Using the model functions calculated from the anthropomorphic phantom study
continual NECR curves can be estimated from patient scans. Patient rates can
be estimated from our proof of principle clinical trial, involving 4 patients, and a
study examining the use of DbPET/CT in primary therapy response monitoring,
which is set to include 20 patients scanned a total of 3 times each. For each
patient the injection time, injection activity, patient body mass index (BMI), and
breast volume (calculated from the CT scan) will be recorded. In addition to
NECR curves, injection activity will be normalized for uptake time, representing
the activity administered the patient 60 minutes before the mean imaging time.
Optimal injection activity will be taken to be the activity at 95% of the peak SNR,
as this will typically result in minimal reduction in image SNR, but a significant
reduction in radiation dose. Plots of optimal injection activity versus BMI and
breast volume will be generated.
133
7.3
Clinical Utility of Quantitative Metrics in
Patient Imaging
7.3.1
Neoadjuvant Therapy Response Monitoring
Based on changes in SUVs with respect to a baseline scan, WB PET imaging
18
F-FDG has shown high accuracy in predicting a subject’s pathological response
to neoadjuvant chemotherapy of breast cancer, and after far fewer cycles of therapy than conventional imaging (see section 1.8). The limitations of WB PET in
breast imaging (see section 1.8), however, may significantly reduce the NPV of
this modality for neoadjuvant therapy response monitoring, especially for smaller
or diffuse stage II breast tumors. The use of bPET and PEM scanners may offer
improved diagnostic accuracy over WB PET for this application, and has not been
explored in a clinical trial in the literature to date, to our knowledge. Our group
has recently initiated a clinical trial comparing DbPET/CT with x-ray mammography in predicting response to primary chemotherapy for a cohort of 20 patients.
Metrics for estimating response include changes in SUV and size (maximum diameter and estimated volume) for the primary tumor. Further insight into the
clinical utility of dedicated breast positron emission imaging for neoadjuvant therapy response monitoring would be gained by a direct comparison with WB PET
and WB PET/CT, as well as with DCE-MRI, and comparing bPET with PEM
directly.
134
References
[1] T. G. Turkington, S. Majewski, A. G. Weisenberger, V. Popov, M. F. Smith,
W. H. Sampson, R. Wojcik, D. Kieper, and S. Majewski, “A large field of
view positron emission mammography imager,” in Nuclear Science Symposium Conference Record, 2002 IEEE, vol. 3, 2002, pp. 1883–1886 vol.3.
[2] R. Freifelder, C. Cardi, I. Grigoras, J. R. Saffer, J. S. Karp, and C. Cardi,
“First results of a dedicated breast PET imager, BPET, using NaI(Tl) curve
plate detectors,” in Nuclear Science Symposium Conference Record, 2001
IEEE, vol. 3, 2001, pp. 1241–1245 vol.3.
[3] R. R. Raylman, M. F. Smith, P. E. Kinahan, and S. Majewski, “Quantification of radiotracer uptake with a dedicated breast PET imaging system,”
Medical Physics, vol. 35, no. 11, pp. 4989–4997, 2008.
[4] M. Furuta, K. Kitamura, J. Ohi, H. Tonami, Y. Yamada, T. Furumiya,
M. Satoh, T. Tsuda, M. Nakazawa, N. Hashizume, and et al., “Basic evaluation of a c-shaped breast pet scanner,” in Nuclear Science Symposium
Conference Record, 2009 IEEE, 2009, pp. 2548–2552.
[5] American Cancer Society, Breast Cancer Facts & Figures 2009-2010. American Cancer Society, Inc., 2010.
[6] W. L. Donegan and J. S. Spratt, “Cancer of the breast,” St. Louis, 2002.
[7] S. R. Cherry, J. A. Sorenson, and M. E. Phelps, Physics in Nuclear Medicine.
Philadelphia: Saunders, 2003, vol. 3rd.
[8] J. L. Humm, A. Rosenfeld, and A. D. Guerra, “From PET detectors to PET
scanners,” European Journal of Nuclear Medicine and Molecular Imaging,
vol. 30, no. 11, pp. 1574–1597, 2003.
[9] O. Warburg, “Origin of cancer cells,” Science, vol. 123, no. 3191, pp. 309–
314, 1956.
[10] R. S. Brown and R. L. Wahl, “Overexpression of GLUT-1 glucose-transporter
in human breast-cancer - an immunohistochemical study,” Cancer, vol. 72,
no. 10, pp. 2979–2985, 1993.
[11] R. B. Workman, R. E. Coleman, and M. P. Sandler, PET/CT essentials for
clinical practice. Springer, 2006.
[12] R. Fazel, H. M. Krumholz, Y. Wang, J. S. Ross, J. Chen, H. H. Ting, N. D.
Shah, K. Nasir, A. J. Einstein, and B. K. Nallamothu, “Exposure to LowDose ionizing radiation from medical imaging procedures,” New England
Journal of Medicine, vol. 361, no. 9, pp. 849–857, 2009.
135
[13] G. Brix, U. Lechel, G. Glatting, S. I. Ziegler, W. Munzing, S. P. Muller, and
T. Beyer, “Radiation exposure of patients undergoing Whole-Body DualModality 18F-FDG PET/CT examinations,” Journal of Nuclear Medicine,
vol. 46, no. 4, pp. 608–613, 2005.
[14] Y. F. Yang, Y. B. Wu, J. Y. Qi, S. St James, H. N. Du, P. A. Dokhale,
K. S. Shah, R. Farrell, and S. R. Cherry, “A prototype PET scanner with
DOI-encoding detectors,” Journal of Nuclear Medicine, vol. 49, no. 7, pp.
1132–1140, 2008.
[15] N. Inadama, H. Murayama, M. Hamamoto, T. Tsuda, Y. Ono, T. Yamaya,
E. Yoshida, K. Shibuya, and F. Nishikido, “8-Layer DOI encoding of 3dimensional crystal array,” IEEE Transaction on Nuclear Science, vol. 53,
no. 5, pp. 2523–2528, 2006.
[16] H. Anger, “Scintillation camera with multichannel collimators,” Journal of
Nuclear Medicine, vol. 5, no. 7, pp. 515–531, 1964.
[17] H. W. A. M. de Jong, F. H. P. van Velden, R. W. Kloet, F. L. Buijs, R. Boellaard, and A. A. Lammertsma, “Performance evaluation of the ECAT HRRT:
an LSO-LYSO double layer high resolution, high sensitivity scanner,” Physics
in Medicine and Biology, vol. 52, no. 5, pp. 1505–1526, 2007.
[18] G. C. Wang, J. S. Huber, W. W. Moses, J. Qi, and W. S. Choong, “Characterization of the LBNL PEM camera,” IEEE Transactions on Nuclear
Science, vol. 53, no. 3, pp. 1129–1135, 2006.
[19] J. A. Fessler, Image Reconstruction: Algorithms and Analysis.
press, 2008.
Book pre-
[20] R. M. Leahy and J. Qi, “Statistical approaches in quantitative positron emission tomography,” Statistics and Computing, vol. 10, no. 2, pp. 147–165,
2000.
[21] S. Surti and J. S. Karp, “Imaging characteristics of a 3-dimensional GSO
whole-body pet camera,” Journal of Nuclear Medicine, vol. 45, no. 6, pp.
1040–1049, 2004.
[22] M. Brambilla, C. Secco, M. Dominietto, R. Matheoud, G. Sacchetti, and
E. Inglese, “Performance characteristics obtained for a new 3-dimensional
lutetium oxylorthosilicate-based whole-body PET/CT scanner with the national electrical manufacturers association NU 2-2001 standard,” Journal of
Nuclear Medicine, vol. 46, no. 12, pp. 2083–2091, 2005.
[23] S. Cherry and M. Dahlbom, PET: Physics, Instrumentation, and Scanners,
2006, pp. 1–117.
136
[24] J. T. Bushberg, The Essential Physics of Medical Imaging, 2nd ed. Lippincott Williams and Wilkins, 2002.
[25] T. G. Flohr, S. Schaller, K. Stierstorfer, H. Bruder, B. M. Ohnesorge, and
U. J. Schoepf, “Multi-detector row CT systems and image-reconstruction
techniques,” Radiology, vol. 235, no. 3, pp. 756–773, 2005.
[26] A. L. C. Kwan, J. M. Boone, and N. Shah, “Evaluation of x-ray scatter
properties in a dedicated cone-beam breast ct scanner,” Medical Physics,
vol. 32, no. 9, pp. 2967–2975, 2005.
[27] C. C. Watson, V. Rappoport, D. Faul, D. W. Townsend, and J. P. Carney, “A
method for calibrating the ct-based attenuation correction of pet in human
tissue,” IEEE Transactions on Nuclear Science, vol. 53, no. 1, pp. 102–107,
2006.
[28] C. Christiansen, “X-ray contrast media - an overview,” Toxicology, vol. 209,
no. 2, pp. 185–187, 2005.
[29] P. Dawson, “Functional imaging in CT,” European Journal of Radiology,
vol. 60, no. 3, pp. 331–340, 2006.
[30] S. J. Swensen, L. R. Brown, T. V. Colby, and A. L. Weaver, “Pulmonary
nodules: CT evaluation of enhancement with iodinated contrast material,”
Radiology, vol. 194, no. 2, pp. 393–398, 1995.
[31] M. M. Morrin, R. J. Farrell, J. B. Kruskal, K. Reynolds, J. B. McGee, and
V. Raptopoulos, “Utility of intravenously administered contrast material at
CT colonography,” Radiology, vol. 217, no. 3, pp. 765–771, 2000.
[32] K. A. Miles, “Tumour angiogenesis and its relation to contrast enhancement
on computed tomography: a review,” European Journal of Radiology, vol. 30,
no. 3, pp. 198–205, 1999.
[33] T. M. Blodgett, C. C. Meltzer, and D. W. Townsend, “PET/CT: form and
function,” Radiology, vol. 242, no. 2, pp. 360–385, 2007.
[34] T. F. Lang, B. H. Hasegawa, S. C. Liew, J. K. Brown, S. C. Blankespoor,
S. M. Reilly, E. L. Gingold, and C. E. Cann, “Description of a prototype
emission-transmission computed-tomography imaging-system,” Journal of
Nuclear Medicine, vol. 33, no. 10, pp. 1881–1887, 1992.
[35] T. Beyer, D. W. Townsend, T. Brun, P. E. Kinahan, M. Charron, R. Roddy,
J. Jerin, J. Young, L. Byars, and R. Nutt, “A combined PET/CT scanner for
clinical oncology,” Journal of Nuclear Medicine, vol. 41, no. 8, pp. 1369–1379,
2000.
137
[36] D. W. Townsend, “Dual-modality imaging: Combining anatomy and function,” Journal of Nuclear Medicine, vol. 49, no. 6, pp. 938–955, 2008.
[37] C. J. Thompson, “The problem of scatter correction in positron volume
imaging,” IEEE Transactions on Medical Imaging, vol. 12, no. 1, pp. 124–
132, 1993.
[38] J. Qi and R. H. Huesman, “Scatter correction for positron emission mammography,” Physics in Medicine and Biology, vol. 47, no. 15, pp. 2759–2771,
2002.
[39] S. R. Cherry, S. R. Meikle, and E. J. Hoffman, “Correction and characterization of scattered events in Three-Dimensional PET using scanners with
retractable septa,” The Journal of Nuclear Medicine, vol. 34, no. 4, pp. 671–
678, 1993.
[40] S. R. Cherry and S. C. Huang, “Effects of scatter on model parameter estimates in 3D PET studies of the human brain,” IEEE Transactions on
Nuclear Science, vol. 42, no. 4, pp. 1174–1179, 1995.
[41] P. L. Chow, F. R. Rannou, and A. F. Chatziioannou, “Attenuation correction
for small animal pet tomographs,” Physics in Medicine and Biology, vol. 50,
no. 8, pp. 1837–1850, 2005.
[42] P. E. Kinahan, B. H. Hasegawa, and T. Beyer, “X-ray-based attenuation correction for positron emission tomography/computed tomography scanners,”
Seminars in Nuclear Medicine, vol. 33, no. 3, pp. 166–179, 2003.
[43] E. J. Hoffman, S. C. Huang, M. E. Phelps, and D. E. Kuhl, “Quantitation
in positron emission computed tomography: 4. effect of accidental coincidences,” J Comput Assist Tomogr, vol. 5, no. 3, pp. 391–400, 1981.
[44] T. J. Spinks, M. P. Miller, D. L. Bailey, P. M. Bloomfield, L. Livieratos, and
T. Jones, “The effect of activity outside the direct field of view in a 3D-only
whole-body positron tomograph,” Physics in Medicine and Biology, vol. 43,
pp. 895–904, 1998.
[45] M. E. Daube-Witherspoon and R. E. Carson, “Unified deadtime correction
model for PET,” Medical Imaging, IEEE Transactions on, vol. 10, no. 3, pp.
267–275, 1991.
[46] L. Eriksson, K. Wienhard, and M. Dahlbom, “A simple data loss model for
positron camera systems,” IEEE Transactions on Nuclear Science, vol. 41,
no. 4, pp. 1566–1570, 1994.
[47] G. F. Knoll, Radiation detection and measurement.
Inc, 1999, vol. 3rd.
John Wiley & Sons,
138
[48] J. A. Sorenson, “Deadtime characteristics of anger cameras,” The Journal of
Nuclear Medicine, vol. 16, no. 4, pp. 284–288, 1975.
[49] M. V. Green, J. Seidel, S. D. Stein, T. E. Tedder, K. M. Kempner, C. Kertzman, and T. A. Zeffiro, “Head movement in normal subjects during simulated
PET brain imaging with and without head restraint,” Journal of Nuclear
Medicine, vol. 35, pp. 1538–1546, 1994.
[50] Y. E. Erdi, S. A. Nehmeh, T. Pan, A. Pevsner, K. E. Rosenzweig, G. Mageras,
E. D. Yorke, H. Schoder, W. Hsiao, O. D. Squire, P. Vernon, J. B. Ashman,
H. Mostafavi, S. M. Larson, and J. L. Humm, “The CT motion quantitation
of lung lesions and its impact on PET-measured SUVs,” Journal of Nuclear
Medicine, vol. 45, no. 8, pp. 1287–1292, 2004.
[51] S. A. Nehmeh, Y. E. Erdi, C. C. Ling, K. E. Rosenzweig, H. Schoder, S. M.
Larson, H. A. Macapinlac, O. D. Squire, and J. L. Humm, “Effect of respiratory gating on quantifying PET images of lung cancer,” Journal of Nuclear
Medicine, vol. 43, no. 7, pp. 876–881, 2002.
[52] N. Avril, S. Bense, S. I. Ziegler, J. Dose, W. Weber, C. Laubenbacher,
W. Romer, F. Jonicke, and M. Schwaiger, “Breast imaging with Fluorine-18FDG PET: quantitative image analysis,” The Journal of Nuclear Medicine,
vol. 38, no. 8, pp. 1186–1191, 1997.
[53] P. M. Hayton, M. Brady, S. M. Smith, and N. Moore, “A non-rigid registration algorithm for dynamic breast MR images,” Artificial Intelligence, vol.
114, no. 1-2, pp. 125–156, 1999.
[54] C. Schorn, U. Fischer, W. Doler, M. Funke, and E. Grabbe, “Compression
device to reduce motion artifacts at contrast-enhanced MR imaging in the
breast,” Radiology, vol. 206, no. 1, pp. 279–82, 1998.
[55] S. C. Strother, M. E. Casey, and E. J. Hoffman, “Measuring PET scanner
sensitivity: relating countrates to image signal-to-noise ratios using noise
equivalents counts,” Nuclear Science, IEEE Transactions on, vol. 37, no. 2,
pp. 783–788, 1990.
[56] M. Dahlbom, C. Schiepers, and J. Czernin, “Comparison of noise equivalent
count rates and image noise,” IEEE Transactions on Nuclear Science, vol. 52,
no. 5, pp. 1386–1390, 2005.
[57] C. C. Watson, M. E. Casey, B. Bendriem, J. P. Carney, D. W. Townsend,
S. Eberl, S. Meikle, and F. P. DiFilippo, “Optimizing injected dose in clinical
PET by accurately modeling the counting-rate response functions specific to
individual patient scans,” Journal of Nuclear Medicine, vol. 46, no. 11, pp.
1825–1834, 2005.
139
[58] R. D. Badawi, P. Domigan, O. Johnson, B. Kemp, H. Kudrolli, T. Rempel,
R. Rohatgi, L. V. Romanov, S. Surti, W. A. Worstell, and R. E. Zimmerman, “Count-rate dependent event mispositioning and NEC in PET,” IEEE
Transactions on Nuclear Science, vol. 51, no. 1, pp. 41–45, 2004.
[59] R. D. Badawi, S. G. Kohlmyer, R. L. Harrison, S. D. Vannoy, and T. K.
Lewellen, “The effect of camera geometry on singles flux, scatter fraction and
trues and randoms sensitivity for cylindrical 3D PET - a simulation study.”
IEEE Transactions on Nuclear Science, vol. 47, no. 3, pp. 1228–1232, 2000.
[60] O. Mawlawi, D. A. Podoloff, S. Kohlmyer, J. J. Williams, C. W. Stearns,
R. F. Culp, and H. Macapinlac, “Performance characteristics of a newly
developed PET/CT scanner using NEMA standards in 2D and 3D modes,”
The Journal of Nuclear Medicine, vol. 45, no. 10, pp. 1734–1742, 2004.
[61] J. Zhang, P. D. Olcott, G. Chinn, A. M. K. Foudray, and C. S. Levin, “Study
of the performance of a novel 1 mm resolution dual-panel PET camera design
dedicated to breast cancer imaging using monte carlo simulation,” Medical
Physics, vol. 34, no. 2, pp. 689–702, 2007.
[62] American Cancer Society, Breast Cancer Facts & Figures 2007-2008.
lanta: American Cancer Society, Inc., 2008.
At-
[63] T. M. Kolb, J. Lichy, and J. H. Newhouse, “Comparison of the performance
of screening mammography, physical examination, and breast US and evaluation of factors that influence them: An analysis of 27,825 patient evaluations,” Radiology, vol. 225, no. 1, pp. 165–175, 2002.
[64] N. Avril, C. A. Rose, M. Schelling, J. Dose, W. Kuhn, S. Bense, W. Weber,
S. Ziegler, H. Graeff, and M. Schwaiger, “Breast imaging with positron emission tomography and fluorine-18 fluorodeoxyglucose: Use and limitations,”
Journal of Clinical Oncology, vol. 18, no. 20, pp. 3495–3502, 2000.
[65] I. Khalkhali, I. Mena, E. Jouanne, L. Diggles, R. Venegas, J. Block, K. Alle,
and S. Klein, “Prone scintimammography in patient with suspicion of carcinoma of the breast,” Journal of the American College of Surgeons, vol. 178,
no. 5, pp. 491–497, 1994.
[66] S. G. Orel and M. D. Schnall, “MR imaging of the breast for the detection,
diagnosis, and staging of breast cancer,” Radiology, vol. 220, no. 1, pp. 13–30,
2001.
[67] N. Avril, S. Sassen, and R. Roylance, “Response to therapy in breast cancer,”
Journal of Nuclear Medicine, vol. 50, no. Suppl-1, pp. 55S–63, 2009.
[68] C. Rousseau, A. Devillers, C. Sagan, L. Ferrer, B. Bridji, L. Campion,
M. Ricaud, E. Bourbouloux, I. Doutriaux, M. Clouet, D. Berton-Rigaud,
140
C. Bouriel, V. Delecroix, E. Garin, S. Rouquette, I. Resche, P. Kerbrat, J. F.
Chatal, and M. Campone, “Monitoring of early response to neoadjuvant
chemotherapy in stage ii and iii breast cancer by [F-18]fluorodeoxyglucose
positron emission tomography,” Journal of Clinical Oncology, pp. 5366–5372,
2006.
[69] S. Mahner, S. Schirrmacher, W. Brenner, L. Jenicke, C. R. Habermann,
N. Avril, and J. Dose-Schwarz, “Comparison between positron emission tomography using 2-[fluorine-18]fluoro-2-deoxy-D-glucose, conventional imaging and computed tomography for staging of breast cancer,” Annals of Oncology, vol. 19, no. 7, pp. 1249–1254, 2008.
[70] M. Schelling, N. Avril, J. Nahrig, W. Kuhn, W. Romer, D. Sattler,
M. Werner, J. Dose, F. Janicke, H. Graeff, and M. Schwaiger, “Positron
emission tomography using [F-18]fluorodeoxyglucose for monitoring primary
chemotherapy in breast cancer,” Journal of Clinical Oncology, vol. 18, no. 8,
pp. 1689–1695, 2000.
[71] R. Kumar, V. A. Loving, A. Chauhan, H. Zhuang, S. Mitchell, and A. Alavi,
“Potential of dual-time-point imaging to improve breast cancer diagnosis
with 18f-fdg pet,” Journal of Nuclear Medicine, vol. 46, no. 11, p. 1819,
2005.
[72] T. A. Heusner, S. Kuemmel, L. Umutlu, A. Koeninger, L. S. Freudenberg,
E. A. M. Hauth, K. R. Kimmig, M. Forsting, A. Bockisch, and G. Antoch,
“Breast cancer staging in a single session: Whole-body PET/CT mammography,” J. Nucl. Med., vol. 49, no. 8, pp. 1215–1222, 2008.
[73] M. Tatsumi, C. Cohade, K. Mourtzikos, E. K. Fishman, and R. L. Wahl,
“Initial experience with FDG-PET/CT in the evaluation of breast cancer,”
Europen Journal of Nuclear Medicine and Molecular Imaging, vol. 33, no. 3,
pp. 254–262, 2006.
[74] L. Radan, S. Ben-Haim, R. Bar-Shalom, L. Guralnik, and O. Israel, “The
role of FDG-PET/CT in suspected recurrence of breast cancer,” Cancer, vol.
107, no. 11, pp. 2545–2551, 2006.
[75] S. Carkaci, H. Macapinlac, M. Cristofanilli, O. Mawlawi, E. Rohren, A. Angulo, S. Dawood, E. Resetkova, H. Le-Petross, and W. Yang, “Retrospective
study of F-18-FDG PET/CT in the diagnosis of inflammatory breast cancer:
Preliminary data,” Journal of Nuclear Medicine, vol. 50, no. 2, pp. 231–238,
2009.
[76] M. Imbriaco, M. G. Caprio, G. Limite, L. Pace, T. De Falco, E. Capuano, and
M. Salvatore, “Dual-time-point 18F-FDG PET/CT versus dynamic breast
MRI of suspicious breast lesions,” American Journal of Roentgenology, vol.
191, no. 5, pp. 1323–1330, 2008.
141
[77] W. W. Moses and J. Qi, “Fundamental limits of positron emission mammography,” Nuclear Instruments & Methods in Physics Research Section aAccelerators Spectrometers Detectors and Associated Equipment, vol. 497,
no. 1, pp. 82–89, 2003.
[78] H. Kaida, M. Ishibashi, T. Fuji, S. Kurata, M. Uchida, K. Baba, T. Miyagawa, H. Kaibara, S. Kawamura, E. Ogo, and et al., “Improved breast cancer
detection of prone breast fluorodeoxyglucose-PET in 118 patients,” Nuclear
Medicine Communications, vol. 29, no. 10, pp. 885–893, 2008.
[79] S. S. Orlov, “Theory of 3-dimensional reconstruction.1. conditions for a full
set of projections,” Kristallografiya, vol. 20, no. 3, pp. 511–515, 1975.
[80] R. Freifelder and J. S. Karp, “Dedicated PET scanners for breast imaging,”
Physics in Medicine and Biology, vol. 42, no. 12, pp. 2463–2480, 1997.
[81] C. J. Thompson, K. Murthy, Y. Picard, I. N. Weinberg, and R. Mako,
“Positron emission mammography (PEM) - a promising technique for detecting Breast-Cancer,” IEEE Transactions on Nuclear Science, vol. 42, no. 4,
pp. 1012–1017, 1995.
[82] L. R. MacDonald, J. Edwards, T. K. Lewellen, D. Haseley, J. Rogers, and
P. E. Kinahan, “Clinical imaging characteristics of the positron emission
mammography camera: PEM flex solo II,” Journal of Nuclear Medicine,
vol. 50, no. 10, pp. 1666–1675, 2009.
[83] M. C. Abreu, J. D. Aguiar, F. G. Almeida, P. Almeida, P. Bento, B. Carrico,
M. Ferreira, N. C. Ferreira, F. Goncalves, C. Leong, F. Lopes, P. Lousa,
M. V. Martins, N. Matela, P. R. Mendes, R. Moura, J. Nobre, N. Oliveira,
C. Ortigao, L. Peralta, R. Pereira, J. Rego, R. Ribeiro, P. Rodrigues, J. Sampaio, A. I. Santos, L. Silva, J. C. Silva, P. Sousa, I. C. Teixeira, J. P. Teixeira,
A. Trindade, and J. Varela, “Design and evaluation of the Clear-PEM scanner for positron emission mammography,” IEEE Transactions on Nuclear
Science, vol. 53, no. 1, pp. 71–77, 2006.
[84] E. A. Levine, R. I. Freimanis, N. D. Perrier, K. Morton, N. M. Lesko,
S. Bergman, K. R. Geisinge r, R. C. Williams, C. Sharpe, V. Zavarzin, and
et al., “Positron emission mammography: Initial clinical results,” Annal of
Surgical Oncology, vol. 10, no. 1, pp. 86–91, 2003.
[85] K. Murthy, M. Aznar, C. J. Thompson, A. Loutfi, R. Lisbona, and J. H.
Gagnon, “Results of preliminary clinical trials of the positron emission mammography system PEM-I: a dedicated breast imaging system producing glucose metabolic images using FDG,” Journal of Nuclear Medicine, vol. 41,
no. 11, pp. 1851–1858, 2000.
142
[86] E. L. Rosen, T. G. Turkington, M. S. Soo, J. A. Baker, and R. E. Coleman,
“Detection of primary breast carcinoma with a dedicated, large-field-of-view
FDG PET mammography device: Initial experience,” Radiology, vol. 234,
no. 2, pp. 527–534, 2005.
[87] L. Tafra, Z. Cheng, J. Uddo, M. B. Lobrano, W. Stein, W. A. Berg, E. Levine,
I. N. Weinberg, D. Narayanan, E. Ross, and et al., “Pilot clinical trial of 18Ffluorodeoxyglucose positron-emission mammography in the surgical management of breast cancer,” American Journal of Surgery, vol. 190, no. 4, pp.
628–632, 2005.
[88] W. A. Berg, I. N. Weinberg, D. Narayanan, M. E. Lobrano, E. Ross,
L. Amodei, L. Tafra, L. P. Adler, J. Uddo, W. Stein, and E. A. Levine, “Highresolution fluorodeoxyglucose positron emission tomography with compression (”positron emission mammography”) is highly accurate in depicting
primary breast cancer,” Breast Journal, vol. 12, no. 4, pp. 309–323, 2006.
[89] A. C. of Radiology, Breast imaging reporting and data system (BI-RADS) Mammography. Reston, VA: American College of Radiology, 2003, vol. 4th.
[90] R. R. Raylman, “Positron Emission Tomography-guided biopsy with a dedicated breast scanner: Initial evaluation,” IEEE Transactions on Nuclear
Science, vol. 56, no. 3, pp. 620–624, 2009.
[91] H. D. Li, W. H. Wong, H. Baghaei, J. Uribe, Y. Wang, Y. X. Zhang, S. S.
Kim, R. Ramirez, J. G. Liu, and S. T. Liu, “The engineering and initial results of a transformable low-cost high-resolution PET camera,” IEEE Transactions on Nuclear Science, vol. 54, no. 5, pp. 1583–1588, 2007.
[92] J. M. Boone, K. Yang, G. W. Burkett, N. J. Packard, S. Y. Huang, S. L.
Bowen, R. D. Badawi, and K. K. Lindfors, “An X-ray computed tomography/positron emission tomography system designed specifically for breast
imaging,” Technology in Cancer and Research Treatment, vol. 9, no. 1, pp.
29–43, 2010.
[93] N. K. Doshi, Y. P. Shao, R. W. Silverman, and S. R. Cherry, “Design and
evaluation of an LSO PET detector for breast cancer imaging,” Medical
Physics, vol. 27, no. 7, pp. 1535–1543, 2000.
[94] A. L. C. Kwan, J. M. Boone, K. Yang, and S. Y. Huang, “Evaluation of the
spatial resolution characteristics of a cone-beam breast CT scanner,” Med.
Phys., vol. 34, no. 1, pp. 275–281, 2007.
[95] K. K. Lindfors, J. M. Boone, T. R. Nelson, K. Yang, A. L. C. Kwan, and
D. F. Miller, “Dedicated breast CT: Initial clinical experience,” Radiology,
vol. 246, no. 3, pp. 725–733, 2008.
143
[96] J. M. Boone, A. L. C. Kwan, K. Yang, G. W. Burkett, K. K. Lindfors, and
T. R. Nelson, “Computed tomography for imaging the breast,” Journal of
Mammary Gland Biology and Neoplasia, vol. 11, no. 2, pp. 103–111, 2006.
[97] J. M. Boone, A. L. C. Kwan, J. A. Seibert, N. Shah, K. K. Lindfors, and
T. R. Nelson, “Technique factors and their relationship to radiation dose in
pendant geometry breast CT,” Medical Physics, vol. 32, no. 12, pp. 3767–
3776, 2005.
[98] L. A. Feldkamp, L. C. Davis, and J. W. Kress, “Practical cone-beam algorithm,” Journal of the Optical Society of America A-Optics Image Science
and Vision, vol. 1, no. 6, pp. 612–619, 1984.
[99] M. S. Judenhofer, B. J. Pichler, and S. R. Cherry, “Evaluation of high performance data acquisition boards for simultaneous sampling of fast signals
from PET detectors,” Physics in Medicine and Biology, vol. 50, no. 1, pp.
29–44, 2005.
[100] Y. Wu, S. L. Bowen, K. Yang, N. Packard, L. Fu, G. Burkett Jr., J. Qi,
J. M. Boone, S. R. Cherry, and R. D. Badawi, “PET characteristics of a
dedicated breast PET/CT scanner prototype,” Physics in Medicine and Biology, vol. 54, no. 13, pp. 4273–4287, 2009.
[101] A. Todd-Pokropek, T. Cradduck, and F. Deconinck, “A file format for the
exchange of nuclear-medicine image data - a specification of interfile version
3.3,” Nuclear Medicine Communications, vol. 13, no. 9, pp. 673–699, 1992.
[102] A. J. Chaudhari, A. A. Joshi, S. L. Bowen, R. M. Leahy, S. R. Cherry, and
R. D. Badawi, “Crystal identification in positron emission tomography using
nonrigid registration to a fourier-based template,” Phys. Med. Biol., vol. 53,
no. 18, pp. 5011–5027, 2008.
[103] J. Qi, R. M. Leahy, S. R. Cherry, A. Chatziioannou, and T. H. Farquhar,
“High-resolution 3D Bayesian image reconstruction using the microPET
small-animal scanner,” Physics in Medicine and Biology, no. 4, p. 1001, 1998.
[104] J. M. Boone, N. Shah, and T. R. Nelson, “A comprehensive analysis of
DgN(CT) coefficients for pendant-geometry cone-beam breast computed tomography,” Medical Physics, vol. 31, no. 2, pp. 226–235, 2004.
[105] R. R. Raylman, S. Majewski, R. Wojcik, A. G. Weisenberger, B. Kross, and
V. Popov, “Corrections for the effects of accidental coincidences, compton
scatter, and object size in positron emission mammography (PEM) imaging,”
IEEE Transactions on Nuclear Science, vol. 48, no. 3, pp. 913–923, 2001.
[106] W. Luo, E. Anashkin, and C. G. Matthews, “Performance evaluation of a
PEM scanner using the NEMA NU 4-2008 small animal PET standards,”
IEEE Transactions on Nuclear Science, vol. 57, p. 94103, 2010.
144
[107] National Electrical Manufactures Association, NEMA Standards Publication
NU 4-2008: Performance Measurements of Small Animal Positron Emission
Tomographs. Rosslyn, VA: National Electrical Manufactures Association,
2008.
[108] ——, NEMA Standards Publication NU 2-2001: Performance Measurements
of Positron Emission Tomographs. Rosslyn, VA: National Electrical Manufactures Association, 2001.
[109] Y. F. Yang, Y. C. Tai, S. Siegel, D. F. Newport, B. Bai, Q. Z. Li, R. M.
Leahy, and S. R. Cherry, “Optimization and performance evaluation of the
microPET II scanner for in vivo small-animal imaging,” Physics in Medicine
and Biology, vol. 49, no. 12, pp. 2527–2545, 2004.
[110] S. Jan, G. Santin, D. Strul, S. Staelens, K. Assie, D. Autret, S. Avner,
R. Barbier, M. Bardies, P. M. Bloomfield, D. Brasse, V. Breton, P. Bruyndonckx, I. Buvat, A. F. Chatziioannou, Y. Choi, Y. H. Chung, C. Comtat, D. Donnarieix, L. Ferrer, S. J. Glick, C. J. Groiselle, D. Guez, P. F.
Honore, S. Kerhoas-Cavata, A. S. Kirov, V. Kohli, M. Koole, M. Krieguer,
D. J. van der Laan, F. Lamare, G. Largeron, C. Lartizien, D. Lazaro, M. C.
Maas, L. Maigne, F. Mayet, F. Melot, C. Merheb, E. Pennacchio, J. Perez,
U. Pietrzyk, F. R. Rannou, M. Rey, D. R. Schaart, C. R. Schmidtlein, L. Simon, T. Y. Song, J. M. Vieira, D. Visvikis, R. V. de Walle, E. Wieers, and
C. Morel, “GATE: a simulation toolkit for PET and SPECT,” Physics in
Medicine and Biology, vol. 49, no. 19, pp. 4543–4561, 2004.
[111] R. L. Siddon, “Fast calculation of the exact radiological path for a 3dimensional CT array,” Medical Physics, vol. 12, no. 2, pp. 252–255, 1985.
[112] N. K. Doshi, M. Basic, and S. R. Cherry, “Evaluation of the detectability of
breast cancer lesions using a modified anthropomorphic phantom,” Journal
of Nuclear Medicine, vol. 39, no. 11, pp. 1951–1957, 1998.
[113] J. K. Moran, H. B. Lee, and M. D. Blaufox, “Optimization of urinary FDG
excretion during PET imaging,” Journal of Nuclear Medicine, vol. 40, no. 8,
pp. 1352–1357, 1999.
[114] C. Studholme, D. L. G. Hill, and D. J. Hawkes, “An overlap invariant entropy
measure of 3D medical image alignment,” Pattern Recognition, vol. 32, no. 1,
pp. 71–86, 1999.
[115] L. F. Schelper, H. J. Gosink, B. Meller, E. Richter, and M. Baehre, “Performance comparison of two dual-head coincidence cameras of the first and
latest generation,” Medical Physics, vol. 33, no. 2, pp. 329–336, 2006.
[116] R. R. Raylman, S. Majewski, M. F. Smith, J. Proffitt, W. Hammond,
A. Srinivasan, J. McKisson, V. Popov, A. Weisenberger, C. O. Judy,
145
B. Kross, S. Ramasubramanian, L. E. Banta, P. E. Kinahan, and K. Champley, “The positron emission mammography/tomography breast imaging and
biopsy system (PEM/PET): design, construction and phantom-based measurements,” Physics in Medicine and Biology, vol. 53, no. 3, pp. 637–653,
2008.
[117] J. Fessler and W. Rogers, “Spatial resolution properties of penalizedlikelihood image reconstruction: Space-invariant tomographs,” IEEE Transactions on Image Processing, vol. 5, no. 9, pp. 1346–1358, 1996.
[118] S. L. Bowen, Y. Wu, A. J. Chaudhari, L. Fu, N. J. Packard, G. W. Burkett,
K. Yang, K. K. Lindfors, D. K. Shelton, R. Hagge, A. D. Borowsky, S. R.
Martinez, J. Qi, J. M. Boone, S. R. Cherry, and R. D. Badawi, “Initial characterization of a dedicated breast PET/CT scanner during human imaging,”
Journal of Nuclear Medicine, vol. 50, no. 9, pp. 1401–1408, 2009.
[119] D. L. Miglioretti, C. M. Rutter, B. M. Geller, G. Cutter, W. E. Barlow,
R. Rosenberg, D. L. Weaver, S. H. Taplin, R. Ballard-Barbash, P. A. Carney, and et al., “Effect of breast augmentation on the accuracy of mammography and cancer characteristics,” JAMA-Journal of the American Medical
Association, vol. 291, pp. 442–450, 2004.
[120] C. H. McCollough and F. E. Zink, “Performance evaluation of a multi-slice
CT system,” Medical Physics, vol. 26, no. 11, pp. 2223–2230, 1999.
[121] R. L. Harrison, S. D. Vannoy, D. R. Haynor, S. B. Gillispie, M. S. Kaplan, and
T. K. Lewellen, “Preliminary experience with the photon history generator
module of a public-domain simulation system for emission tomography,” in
Nuclear Science Symposium and Medical Imaging Conference Record, 1993
IEEE, 1993, pp. 1154–1158.
[122] N. K. Doshi, R. W. Silverman, Y. Shao, and S. R. Cherry, “maxPET: a dedicated mammary and axillary region PET imaging system for breast cancer,”
IEEE Transactions on Nuclear Science, vol. 48, no. 3, pp. 811–815, 2001.
[123] R. D. Badawi, M. A. Lodge, and P. K. Marsden, “Algorithms for calculating detector efficiency normalization coefficients for true coincidences in 3D
PET,” Physics in Medicine and Biology, vol. 43, no. 1, pp. 189–205, 1998.
[124] P. E. Kinahan, D. W. Townsend, T. Beyer, and D. Sashin, “Attenuation
correction for a combined 3D PET/CT scanner,” Medical Physics, vol. 25,
no. 10, pp. 2046–2053, 1998.
[125] M. E. Daube-Witherspoon and G. Muehllehner, “Treatment of axial data
in three-dimensional PET,” Journal of Nuclear Medicine, vol. 28, no. 11, p.
1717, 1987.
146
[126] M. Defrise, P. E. Kinahan, D. W. Townsend, C. Michel, M. Sibomana, and
D. F. Newport, “Exact and approximate rebinning algorithms for 3-D PET
data,” IEEE Transactions on Medical Imaging, vol. 16, no. 2, p. 145158,
1997.
[127] R. D. Badawi, M. P. Miller, D. L. Bailey, and P. K. Marsden, “Randoms
variance reduction in 3D PET,” Physics in Medicine and Biology, vol. 44,
no. 4, pp. 941–954, 1999.
[128] S. Grootoonk, T. J. Spinks, D. Sashin, N. M. Spyrou, and T. Jones, “Correction for scatter in 3D brain PET using a dual energy window method,”
Physics in Medicine and Biology, vol. 41, no. 12, pp. 2757–2774, 1996.
[129] S. C. Huang, E. J. Hoffman, M. E. Phelps, and D. E. Kuhl, “Quantitation in
positron emission computed-tomography .2. effect of inaccurate attenuation
correction,” Journal of Computer Assisted Tomography, vol. 3, no. 6, pp.
804–814, 1979.
[130] G. Germano and E. J. Hoffman, “A study of data loss and mispositioning due
to pileup in 2-D detectors in pet,” IEEE Transactions on Nuclear Science,
vol. 37, no. 2, pp. 671–675, 1990.
[131] G. Antoch, L. S. Freudenberg, T. Egelhof, J. Stattaus, W. Jentzen, J. F. Debatin, and A. Bockisch, “Focal tracer uptake: a potential artifact in contrastenhanced dual-modality PET/CT scans,” Journal of Nuclear Medicine,
vol. 43, no. 10, pp. 1339–1342, 2002.
[132] H. Zaidi, “Comparative evaluation of scatter correction techniques in 3D
positron emission tomography,” European Journal of Nuclear Medicine and
Molecular Imaging, vol. 27, no. 12, pp. 1813–1826, 2000.
[133] R. Accorsi, L. E. Adam, M. E. Werner, and J. S. Karp, “Optimization
of a fully 3D single scatter simulation algorithm for 3D PET,” Physics in
Medicine and Biology, vol. 49, no. 12, pp. 2577–2598, 2004.
[134] D. R. Haynor, R. L. Harrison, and T. K. Lewellen, “The use of importance
sampling techniques to improve the efficiency of photon tracking in emission
tomography simulations,” Medical Physics, vol. 18, no. 5, pp. 990–1001, 1991.
[135] R. D. Badawi and P. K. Marsden, “Developments in component-based normalization for 3D pet,” Physics in Medicine and Biology, vol. 44, no. 2, pp.
571–94, 1999.
[136] J. M. Ollinger, “Detector efficiency and compton scatter in fully 3D PET,”
IEEE Transactions on Nuclear Science, vol. 42, no. 4, pp. 1168–1173, 1995.
147
[137] M. Conti, J. Hamill, and W. K. Luk, “Component-based normalization for
panel detector pet scanners,” IEEE Transactions on Nuclear Science, vol. 51,
no. 1, pp. 16–20, 2004.
[138] B. Bai, Q. Li, C. H. Holdsworth, E. Asma, Y. C. Tai, A. Chatziioannou,
and R. M. Leahy, “Model-based normalization for iterative 3d pet image
reconstruction,” Physics in Medicine and Biology, vol. 47, no. 15, pp. 2773–
2784, 2002.
[139] F. Lamare, S. L. Bowen, D. Visvikis, P. A. C. P. Cortes, Y. Wu., V. H.
Tran, J. M. Boone, S. R. Cherry, and R. D. Badawi, “Design simulation
of a rotating dual-headed PET/CT scanner for breast imaging,” in Nuclear
Science Symposium Conference Record, 2005 IEEE, vol. 3, 2005, p. 6 pp.
[140] S. L. Bowen, S. R. Cherry, J. M. Boone, and R. D. Badawi, “Monte Carlo
simulation study of several camera designs for the PET component of a dedicated breast PET/CT scanner,” in European Journal of Nuclear Medicine
and Molecular Imaging Meeting Abstracts, 2006.
[141] W. P. Segars, D. S. Lalush, and B. M. W. Tsui, “Modeling respiratory mechanics in the MCAT and spline-based MCAT phantoms,” IEEE Transactions on Nuclear Science, vol. 48, no. 1, pp. 89–97, 2001.
[142] C. D. Ramos, Y. E. Erdi, M. Gonen, E. Riedel, H. W. D. Yeung, H. A.
Macapinlac, R. Chisin, and S. M. Larson, “FDG-PET standardized uptake
values in normal anatomical structures using iterative reconstruction segmented attenuation correction and filtered back-projection,” European Journal of Nuclear Medicine, vol. 28, no. 2, pp. 155–164, 2001.
[143] A. M. Alessio, P. E. Kinahan, and T. K. Lewellen, “Modeling and incorporation of system response functions in 3-D whole body PET,” IEEE Transactions on Medical Imaging, vol. 25, no. 7, pp. 828–837, 2006.
[144] M. S. Tohme and J. Qi, “Iterative image reconstruction for positron emission tomography based on a detector response function estimated from point
source measurements,” Physics in Medicine and Biology, vol. 54, no. 12, pp.
3709–3725, 2009.
[145] D. L. Bailey, H. Young, P. M. Bloomfield, S. R. Meikle, D. Glass, M. J. Myers,
T. J. Spinks, C. C. Watson, P. Luk, A. M. Peters, and T. Jones, “ECAT
ART - a continuously rotating PET camera: Performance characteristics,
initial clinical studies, and installation considerations in a nuclear medicine
department,” European Journal of Nuclear Medicine, vol. 24, no. 1, pp. 6–15,
1997.
[146] M. J. Yaffe, J. M. Boone, N. Packard, O. Alonzo-Proulx, S.-Y. Huang, C. L.
Peressotti, A. Al-Mayah, and K. Brock, “The myth of the 50-50 breast,”
Medical Physics, vol. 36, no. 12, pp. 5437–5443, 2009.
148
[147] J.
Bouguet,
“Camera
calibration
toolbox
for
matlab,”
http://robots.stanford.edu/cs223b04/JeanYvesCalib/index.html#system,
2003.
[148] B. J. Lopresti, A. Russo, W. F. Jones, T. Fisher, D. G. Crouch, D. E. Altenburger, and D. Townsend, “Implementation and performance of an optical motion tracking system for high resolution brain PET imaging,” Nuclear
Science, IEEE Transactions on, vol. 46, no. 6, pp. 2059–2067, 1999.