* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CDHO Factsheet Strep Throat (Group A Strep)
Transmission (medicine) wikipedia , lookup
Schistosomiasis wikipedia , lookup
Neonatal infection wikipedia , lookup
Periodontal disease wikipedia , lookup
Globalization and disease wikipedia , lookup
Urinary tract infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Gastroenteritis wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Infection control wikipedia , lookup
Common cold wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
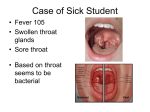
Disease/Medical Condition STREP THROAT Date of Publication: March 11, 2013 (also know as “streptococcal sore throat”, “strep pharyngitis”, and “strep tonsillitis”; caused by Group A [beta-haemolytic] streptococci bacteria [GAS]) Is the initiation of non-invasive dental hygiene procedures* contra-indicated? Yes ■ Is medical consult advised? Yes, if the patient/client has suspected or laboratory-confirmed strep throat or is otherwise unwell with oral manifestations and related signs and symptoms. Refer to primary care provider (e.g., physician or nurse practitioner) for follow-up and definitive diagnosis (e.g., throat swab and culture or rapid strep test). Instruct patient/client to reschedule dental hygiene appointment when s/he feels well AND when antibiotic therapy has been initiated for at least 24 hours if strep throat has been diagnosed. If there is a patient/client history of rheumatic fever (now rare in developed countries), it is most prudent to wait until the course of antibiotic treatment has been completed. Antibiotic regimens − such as penicillin V and most alternatives − typically require a 10-day course to achieve successful treatment and prevent poststreptococcal complications. A notable exception is azithromycin which, given its long half-life, requires only 5 days of therapy. Is the initiation of invasive dental hygiene procedures contra-indicated?** Yes ■ ■ ■ ■ Is Is Is Is medical consult advised? ............................................... Yes; see above. medical clearance required? .......................................... Yes antibiotic prophylaxis required? ...................................... No postponing treatment advised? ....................................... Yes (until patient/client has been on an antibiotic regimen for at least 24 hours) Oral management implications ■ Mode of transmission is most commonly via large respiratory droplets or direct contact with patients/clients or carriers, and rarely via direct contact with objects. Outbreaks of strep throat may occur via ingestion of contaminated food; contamination of milk or egg products by humans appears to be the most important source of foodborne episodes. ■ In untreated, uncomplicated cases, the period of communicability is typically 10−21 days. With adequate penicillin treatment, transmissibility usually ends within 24 hours. Persons with untreated strep throat may carry the bacteria for weeks to months; contagiousness of these persons decreases sharply in 2−3 weeks after the onset of infection. ■ In cases of laboratory confirmed or suspected strep throat, delay elective treatment until the signs and symptoms of strep throat have subsided and antibiotic therapy has been initiated for at least 24 hours and preferably for the full duration of the prescription (typically 10 days). ■ Spread of GAS infection can be reduced by good hand washing, especially after coughing and sneezing. Oral manifestations ■ Red and swollen tonsils, often with white patches (exudate) or streaks of pus (purulent discharge) ■ Red spots (petechiae) on the soft and/or hard palate ■ Throat pain and difficulty swallowing cont’d on next page... Disease/Medical Condition STREP THROAT (also know as “streptococcal sore throat”, “strep pharyngitis”, and “strep tonsillitis”; caused by Group A [beta-haemolytic] streptococci bacteria [GAS]) Related signs and symptoms ■ Fever; swollen, tender lymph nodes in the neck; headache; rash; abdominal pain (especially in young children, and sometimes accompanied by vomiting); fatigue. ■ Some people may carry GAS in the throat or on the skin and have no symptoms of illness. Most GAS infections are relatively mild illnesses such as strep throat or impetigo. Severe, sometimes life-threatening, GAS infections occasionally occur when bacteria spread to the blood, muscles, or lungs. ■ Sick persons, such as those who have strep throat or impetigo, are most likely to spread the infection. Persons who carry the bacteria but are asymptomatic are much less contagious. References and sources of more detailed information ■ US Centers for Disease Control and Prevention http://www.cdc.gov/ncidod/dbmd/diseaseinfo/groupastreptococcal_g.htm ■ Medline Plus A Service of the US National Library of Medicine National Institutes of Health http://www.nlm.nih.gov/medlineplus/impetigo.html ■ Canadian Paediatric Society, Caring for Kids http://www.caringforkids.cps.ca/handouts/strep_throat ■ Mayo Clinic http://www.mayoclinic.com/health/strep-throat/DS00260/DSECTION=symptoms ■ Anti-Infective Review Panel. Anti-infective guidelines for community-acquired infections. Toronto: MUMS Guideline Clearinghouse; 2010. ■ David L. Heymann (ed.). Control of Communicable Disease Manual (18th edition). Baltimore: American Public Health Association; 2004. * Includes oral hygiene instruction, fitting a mouth guard, taking an impression, etc. ** Ontario Regulation 501/07 made under the Dental Hygiene Act, 1991. Invasive dental hygiene procedures are scaling teeth and root planing, including curetting surrounding tissue. Date: December 10, 2012 69 Bloor St. E, Suite 300, Toronto, ON M4W 1A9 t: 416-961-6234 ● tf: 1-800-268-2346 ● f: 416-961-6028 ● www.cdho.org 2