* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Over-the-counter vaginal preparations
Survey
Document related concepts
Transcript
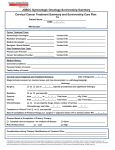
Review Over-the-counter vaginal preparations Johnston L, BPharm Amayeza Info Centre The vagina is typically acidic (pH around 3.5-4.5) in healthy women during their fertile years. The acidic environment is established by the presence of Lactobacillus species which have an essential role in preventing the proliferation of pathogenic microorganisms. The vagina offers a good drug delivery site thanks to its large surface area, rich blood supply, and reduced enzymatic breakdown as compared with the gastrointestinal tract. However, there are some limitations to the intravaginal route, such as variability in drug absorption related to the menstrual cycle, pregnancy and menopause. Symptoms include: • • • Itching, discomfort and/or burning in the vagina; A white curd-like discharge; A red rash affecting the inner and outer parts of the vulva. Azole antifungals such as clotrimazole and miconazole are the drugs of choice for the local treatment of vulvovaginal candidiasis (vaginal thrush). There is no clear evidence that one intravaginal azole is more effective than another. Intravaginal nystatin may also be used in the treatment of uncomplicated vulvovaginal candidiasis. However, it is generally less effective than the intravaginal azole antifungals. vaginalis and Mycoplasma hominis and a decrease in the levels of lactobacilli. Bacterial vaginosis is often asymptomatic and may resolve spontaneously. However, treatment is indicated in symptomatic women. Symptoms may include an abnormal white or grey vaginal discharge with an unpleasant odour (sometimes reported as a fish-like odour, especially after intercourse). The patient may also report burning during urination and or itching around the outside of the vagina. Low sugar/yeast and high yoghurt diets have not been shown to be effective, nor has inserting yoghurt into the vagina. Intravaginal metronidazole is as effective as a seven-day oral metronidazole regimen. The dosage is one applicatorful (37.5 mg/5 g dose) administered intravaginally, once daily, preferably at bedtime, for five consecutive days. An available formulation is Metrogel V®. Approximately 20% of non-pregnant women aged 15-55 years harbour Candida albicans, a type of yeast, in the vagina. Candidial infection is more prevalent in this age group due to the presence of oestrogen, which causes the lining to mature and produce glycogen on which Candida albicans thrives. Most individuals have no symptoms of infection, unless there is overgrowth of the organism. Who should be referred? Other vaginal infections • • Povidone iodine is a broad-spectrum antiseptic with bactericidal and fungicidal properties. It is indicated in the treatment of trichomonal, candidial and nonspecific vaginal infections. Available preparations include Betadine® Douche and Betadine® Vaginal Gel. Overgrowth of Candida albicans may be precipitated by: • • • • • • Several types of intravaginal formulations are available. These include tablets, ovules, gels, creams, and douches. Vaginal candidiasis (thrush) Vaginal candidiasis is not usually acquired through sexual contact and treatment of the sexual partner is not recommended, but may be considered in women who have recurrent infections. • Table I lists a number of OTC vaginal formulations for the treatment of vaginal candidiasis. Bacterial vaginosis Bacterial vaginosis is not caused by a single organism. It is a complex change in the vaginal flora characterised by an increase in the levels of Gardnerella Povidone iodine vaginal preparations should not be used by pregnant or breastfeeding women. Atrophic vaginitis Atrophic vaginitis is inflammation of the vagina due to reduced lubrication and thinning tissue. It is caused by reduced levels of oestrogen, generally following menopause. Oestrogen assists in keeping the vagina lubricated and healthy. However, when oestrogen levels drop, vaginal tissue may become thin, dry and inflamed. Atrophic vaginitis can also occur in younger women who have had their ovaries removed, or immediately after childbirth, or during lactation when oestrogen levels are lower. SA Pharmacist’s Assistant [ Autumn 2011 ] • Pregnancy; Broad-spectrum antibiotics; Diabetes mellitus; Immunosuppression [e.g. human immunodeficiency virus (HIV) infection or chemotherapy]; Combined oral contraceptives or oestrogen-based hormone replacement therapy. • Pregnant patients. Patients whose infections do not improve within three days, or that persist beyond seven days of having started treatment. Patients who have symptoms of vulvovaginal candidiasis that recurs within two months of using vaginal cream self-medication. Patients who are experiencing vaginal itching or discomfort for the first time. Patients experiencing malodorous vaginal discharge, or abdominal pain and fever. Girls under the age of 12 years. 25 Review Table I: Available over-the-counter (OTC) vaginal formulations Topical antifungal Available formulations Dose and administration Clotrimazole Vaginal creams: A-Por®, Canalba®, Candaspor®, Candizole V®, Canestan®, Canex®, Closcript®, Covospor®, Fungispor V®, Innospor®, Medaspor®, Normospor® One applicatorful (about 5 g) of the 1% cream inserted into the vagina daily (preferably at night) for six to seven consecutive days. Cream may also be applied to the external genitalia two to three times a day for one to two weeks. Nystatin Vaginal tablets: Canstat® tablets (100 000 units of nystatin per tablet) Insert one to two tablets (100 000 to 200 000 units) daily. Two weeks of the therapy is usually sufficient, but prolonged treatment may be necessary. It is important for the treatment to be continued during menstruation. Miconazole nitrate Vaginal cream: Gyno Daktarin® Insert one applicatorful (5 g) into the vagina at night, for seven days. Vaginal capsules: Gyno Daktarin® single-dose (1 200 mg) vaginal capsules. Vaginal cream and capsules: Gyno Daktarin Combipak® Insert the capsule into the vagina at night. Vaginal cream: Gyno-Pevaryl® cream Vaginal ovules: Gyno-Pevaryl® ovules One applicatorful at night for two weeks. Vaginal depot-ovule: Gyno-Pevaryl® depot-ovule One depot-ovule (150 mg) in the vagina before retiring for the night. Econazole Symptoms of atrophic vaginitis may include: • • • • Burning on urination; Painful intercourse; Vaginal pain, including itching or burning; Slight vaginal discharge. Treatments SA Pharmacist’s Assistant [ Autumn 2011 ] Vaginal lubricants and moisturisers 26 Mild symptoms during intercourse may be relieved by water-soluble vaginal lubricants such as KY® jelly or Durex® water-soluble lubricants . An OTC, water-based moisturising gel (Replens®) is available as a vaginal moisturiser. Replens® is an aqueous gel containing 78.82% purified water in a hydrophilic polymer base. The vaginal gel offers long lasting moisture and should be used every three days for best results, although it is safe to use daily if necessary. KY® jelly, Durex® lubricants and Replens® are compatible with condom use. Insert one capsule into the vagina at night for three consecutive nights, and apply the cream around the entrance to the vagina mornings and evenings. One ovule (150 mg) nightly for three consecutive nights. Vaginal oestrogen preparations Bibliography Vaginal oestrogen therapy is indicated for short-term treatment of symptoms related to vaginal atrophy in postmenopausal women. Available formulations include Synapause® and Premarin® creams and Vagifem® vaginal tablets. 1. 2. Instructions for use of vaginal formulations 4. 5. • 6. 7. • • • • • • • Wash your hands with soap and water. Open/prepare the vaginal applicators. Lie on your back with the knees drawn up, or squat, or stand with one leg up on a chair. Hold open the folds of the skin around the vagina in one hand. Place the tip of the applicator into the vagina, then, using the index finger, gently push the applicator into vagina until there is some resistance. Depress the plunger expelling the preparation (tablet/cream/ovule/ capsule). Remove the applicator. Wash your hands and the applicator with warm soapy water. 3. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. Gad SC. Pharmaceutical manufacturing handbook: production and processes, Volume 10. Wiley-Interscience. New Jersey: John Wiley and Sons; 2008. Oakley A. New Zealand Dermatological Society. Vulvovaginal candidiasis [homepage on the Internet]. c2010. Available from: http:// dermnetnz.org/fungal/vaginal-candidiasis.html American Hospital Formulary Service (AHFS) Drug Information, 2009. Canstat® vaginal tablets package insert, 1993. Gyno Daktarin® VC vaginal cream package insert, 2009. Gyno Daktarin Combipak® package insert, 2009. Gyno-Pevaryl® vaginal cream package insert, 2005. Gyno-Pevaryl® ovule package insert, 2005. Amayeza Drug Information Centre. MetroGel V: a metronidazole vaginal preparation. SA Fam Pract. 2007:49(4) [homepage on the Internet]. Available at: http://www.safpj.co.za/index.php/ safpj/article/viewFile/831/725 MetroGel V® vaginal gel package insert, 2000. Centres for Disease Control and Prevention. Bacterial vaginosis fact sheet. [homepage on the Internet]. c2011. Available from: http://www. cdc.gov/std/bv/stdfact-bacterial-vaginosis.htm Betadine® douche package insert, 1993. Betadine® vaginal gel package insert, 1987. MedlinePlus. Atrophic vaginitis [homepage on the Internet]. c2011. Available from: http://www. nlm.nih.gov/medlineplus/ency/article/000892. htm Replens ® vaginal moisturising gel package insert, 1994. Synapause® vaginal cream package insert, 2005. Premarin® cream package insert, 1974. Vagifem® vaginal tablets package insert, 1992.