* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download A Primary Care Approach to Treating the Red Eye
Survey
Document related concepts
Transcript
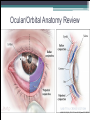
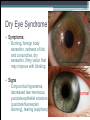
A Primary Care Approach to Treating the Red Eye 30th Annual Family Medicine Review April 12, 2014 Rachel Cook, MD Scott & White Ophthalmology Resident We’re all doctors, so why discuss this? • “Red eye” is a common complaint • It’s intimidating because I might miss something serious! • I feel comfortable with conjunctivitis but am not familiar with many other ocular diagnoses. • How do I know when to refer to ophthalmology? Discussion Topics • History (How to get a useful ophthalmic history!) • Anatomy Review • Exam (What am I looking for?) • Common causes of “red eye” and what to do! Taking a Useful Ophthalmic History: 101 • Still the basics: onset, timing, quality, severity, duration, modifying factors, context • When taking a history, think: Does this sound like something that could: ▫ - kill my patient?!? ▫ - blind my patient or cause significant vision loss? ▫ - be merely uncomfortable and/or self-limited? • Consider systemic context! Taking a Useful Ophthalmic History: 101 • Decreased Vision? ▫ Acute or chronic? ▫ While wearing refractive correction? • Laterality of complaints? • History of Trauma? ▫ ▫ ▫ ▫ Blunt or sharp? What object? Vegetable matter? How severe? Possible ocular laceration? Possible foreign body? Chemical injury? Taking a Useful Ophthalmic History: 101 • Contact Lens Wearer? ▫ Still wearing lenses? ▫ Sleep in lenses? • Itching? Seasonal pattern? • Recent sick contacts? Recent respiratory illness? • Discharge? Tearing? Crusting on eyelids? Taking a Useful Ophthalmic History: 101 • Photophobia? • Foreign body sensation? • Medications ▫ ▫ ▫ ▫ On oral antihistamines? Diuretics? TCAs? Require nasal corticosteroids for allergies? Using topical glaucoma medications? Using OTC topical vasoconstrictors/ “gets the red out” drops? Ocular/Orbital Anatomy Review Encyclopaedia Iranica. FĀRESĪ, KAMĀL-AL-DĪN ABU’L-ḤASAN MOḤAMMAD. http://www.iranicaonline.org/artic les/faresi-2 Ocular/Orbital Anatomy Review © 2013 American Academy of Ophthalmology Ocular/Orbital Anatomy Review © 2013 American Academy of Ophthalmology Ocular/Orbital Anatomy Review JAMA. 2013;310(16):1721-1730. doi:10.1001/jama.2013.280318 Ocular/Orbital Anatomy Review © 2013 American Academy of Ophthalmology Elements of a Complete Eye Exam • • • • • • • • Visual acuity (near and distance) Pupils Motility/alignment Visual fields Tonometry (intraocular pressure) External exam (orbits, eyelids, lashes) Anterior segment exam Posterior segment exam http://www.opsweb.org/?page=Externaleye Anterior Segment Exam • Penlight / Diffuse Beam ▫ Conjunctival injection? How deep does the redness appear? ▫ Chemosis? (Edematous, puffy or ballooning conjunctiva) ▫ Where is the injection? Ciliary flush (deep purple hue at limbus) or limbal sparing? ▫ Cornea clear or hazy? Corneal light reflex sharp or scattered? http://www.med.uottawa.ca/procedures/slamp/seg_exam.htm Anterior Segment Exam • Slit Beam Exam ▫ Scan corneal surface to look for opacities, changing angle of beam. ▫ Look between the two beams at the anterior chamber – should be black space with no cloudiness (cell/flare), hyphema, hypopyon. ▫ Beams should be fairly far apart. © 2013 American Academy of Ophthalmology http://emedicine.medscape.com/article/1228681-overview#aw2aab6b3 Eyelid Eversion Technique http://www.nlm.nih.gov/medlineplus/ency/imagepages/19662.htm Eye Exam Toolkit Essentials http://www.eyesite4u.net https://lombartinstrument.com http:/emedicine.medscape.com/ Proparacaine or Tetracaine http://www.scrubshopper.com http://www.optometrial.com Eye Exam Toolkit Essentials Don’t forget that smartphone or tablet resources can fill in the gaps! Screenshot of my phone – EyeHandbook app “Red eye” Glossary of Terms • Blepharitis – inflammation of eyelid margins • Conjunctivitis – inflammation of conjunctiva (no matter what the etiology) • Episcleritis/Scleritis – inflammation of episclera/sclera (deeper than conjunctiva), often associated with autoimmune disease “Red eye” Glossary of Terms • Corneal abrasion – area of denuded corneal epithelium due to mechanical injury • Keratitis – corneal inflammation, often due to infection • Corneal ulcer – ulcerative keratitis: epithelial defect with stromal inflammatory infiltrate and often thinning, typically infectious Dry Eye Syndrome dry • Symptoms: ▫ Burning, foreign body sensation, redness of lids and conjunctiva, dry sensation, filmy vision that may improve with blinking © 2013 American Academy of Ophthalmology http://en.wikipedia.org/wiki/Naked_eye • Signs ▫ Conjunctival hyperemia, decreased tear meniscus, punctate epithelial erosions (punctate fluorescein staining), tearing (epiphora) normal Dry Eye Syndrome http://www.willseye.org/health-library/dry-eye-syndrome Dry Eye Syndrome • Tear film – 3 layers ▫ Oil (surface) – Meibomian and Zeis glands in eyelid ▫ Aqueous (middle) – main and accessory lacrimal glands ▫ Mucin (juxtacorneal) – conjunctival goblet cells • Deficiency in any layer dry eye symptoms http://www.emedicinehealth.com/dry_eye_syndrome/page17_em.htm Dry Eye Syndrome • Aqueous Tear Deficiency / Keratoconjunctivitis Sicca ▫ Sjögren – Primary or Secondary ▫ Non-Sjögren – many causes but consider medications; elderly, women (low androgen state) at risk http://www.optometricmanagement.com/articleviewer.aspx?articleid=102506 • Evaporative Dry Eye ▫ Blepharitis / Meibomian Gland Dysfunction ▫ Environmental ▫ Accutane ▫ Ectropion/Exposure Dry Eye Syndrome • Initial Management ▫ Artificial tears – frequent use; if >5x/day consider recommending preservative free ▫ Avoid aggravating factors – turn fans off, modify medications ▫ Treat blepharitis – warm compresses, lid hygiene • If unresponsive refer • Severe dry eye can cause corneal decompensation, increased risk of infection, scarring, perforation! http://www.improveeyesighthq.com/blepharitis.html Blepharitis • Chronic eyelid inflammation, typically bilateral • Symptoms: ▫ Burning, eyelid irritation and redness, tearing, foreign body sensation, gritty sensation, blurry vision • Signs: ▫ Eyelid margin redness, swelling, scaling, crusting on lashes ▫ Hordeola (styes) or chalazia ▫ Chronic conjunctivitis red, irritated-looking eye Blepharitis • Seborrheic and Staphylococcal varieties (most common) • Seborrheic associated with rosacea and chalazia • Staphylococcal (typically S. aureus) can be associated with blepharoconjunctivitis = blepharitis presentation + conjunctivitis appearance with scant discharge; also associated with hordeolum (“stye”) formation • Different than acute bacterial conjunctivitis! Blepharitis (Seborrheic) © 2013 American Academy of Ophthalmology Chalazion © 2013 American Academy of Ophthalmology Blepharitis (Staphylococcal) © 2013 American Academy of Ophthalmology External Hordeolum © 2013 American Academy of Ophthalmology Chronic Blepharokeratoconjunctivitis Refer for corneal infiltrates or a cloudy appearance! Blepharitis Conservative Management • warm compresses (several times daily) • lid hygiene (dilute baby shampoo or OTC preps) • topical ophthalmic antibiotic ointment (bacitracin, erythromycin, azithromycin) Both images: http://patienteducationcenter.org/articles/blepharitis/ Sebaceous Carcinoma This can kill your patient! Images courtesy of Evan Silverstein, MD and Louise Mawn, MD http://eyewiki.aao.org/Sebaceous_carcinoma Refer after 3 months of conservative “chalazion” or “chronic unilateral blepharitis” management! From: Conjunctivitis: A Systematic Review of Diagnosis and Treatment JAMA. 2013;310(16):1721-1730. doi:10.1001/jama.2013.280318 Figure Legend: Suggested Algorithm for Clinical Approach to Suspected Acute Conjunctivitis Date of download: 3/25/2014 Copyright © 2014 American Medical Association. All rights reserved. Allergic / Hay Fever Conjunctivitis • Associated with seasonal allergy symptoms • Often in patients with other atopic conditions • Typically Type I hypersensitivity (IgE mediated) ▫ Mast cell degranulation histamine / other inflammatory mediators conjunctivitis • Contact lenses and dry eye can exacerbate symptoms! Allergic / Hay Fever Conjunctivitis • Signs and Symptoms: intense itching, burning eyelid swelling, chemosis, conjunctival hyperemia, mucoid or watery discharge, papillary reaction • Management ▫ Avoidance of allergens ▫ Supportive: cold compresses, artificial tears (try cold!) ▫ Topical antihistamines/mast cell stabilizers (ketotifen, olopatadine) Allergic / Hay Fever Conjunctivitis Digital Reference of Ophthalmology. http://dro.hs.columbia.edu/ Contact Blepharoconjunctivitis • Type I Hypersensitivity - Acute Contact Dermatoblepharitis (immediate) • Type IV Hypersensitivity (T-cell mediated) ▫ Typically begins 24-72 hours after starting a topical medication (diagnostic clues in history are critical) • Clinical appearance and management are the same as allergic/hay fever conjunctivitis + remove offending agent! Contact Blepharoconjunctivitis • Can also get an acute excematous dermatitis on eyelid skin (leathery, scaly, erythematous) • Common culprits for delayed reaction: ▫ Preservatives in OTC and prescription (often generic) eye drops ▫ Topical aminoglycosides: neomycin, gentamicin, tobramycin ▫ Topical antivirals (trifluridine) and cycloplegics (atropine) Viral Conjunctivitis • Typically bilateral (or unilateral quickly bilateral) • Symptoms: ▫ Diffuse hyperemia, watery/serous discharge, sudden onset especially following recent contact with others with “pink eye” or recent respiratory viral illness, mild itching, foreign body sensation, if severe may have photophobia • Signs: ▫ Diffuse conjunctival injection, normal vision, normally reactive pupils, preauricular lymphadenopathy, follicular reaction, severe cases may develop pseudomembranes and/or subepithelial corneal infiltrates Viral Conjunctivitis © 2013 American Academy of Ophthalmology This is not purulent discharge, it is a pseudomembrane! http://www.hindawi.com/journals/joph/2010/423672/fig4/ Viral Conjunctivitis • Common viruses: ▫ Adenovirus – very common, can be very severe (epidemic keratoconjunctivitis) Very contagious! It’s critical to advise hand hygiene, washing linens, etc. Clean your office thoroughly to avoid epidemic! Typically self-limited, worsens over first 4-7 days, lasts 2-3 weeks, contagious while eyes are red ▫ Enterovirus & coxsackievirus (acute hemorrhagic conjunctivitis), molluscum, EBV Viral Conjunctivitis • Treatment for typical viral conjunctivitis: ▫ Counseling about careful hygiene while contagious ▫ Frequent (every 2-4 hours) preservative-free artificial tears ▫ Cool compresses ▫ Topical antibiotics discouraged unless you notice corneal involvement ▫ If corneal involvement or vision decreases refer! Viral Conjunctivitis • Common viruses: ▫ Herpes Simplex Virus Primary ocular – HSV blepharoconjunctivitis can present with typical viral conjunctivitis picture with vesicles on skin or eyelids, can be bilateral, can have epithelial dendritic keratitis Recurrent HSV – typically unilateral, presentation more often involves dendritic and stromal keratitis and iritis HSV Epithelial (Dendritic) Keratitis Digital Reference of Ophthalmology. http://dro.hs.columbia.edu/ Viral Conjunctivitis • Common viruses: ▫ Herpes Simplex Virus Treatment is supportive + referral. Course is self-limited but you may initiate oral antivirals (can shorten duration of symptoms) Treat for 10 days with one antiviral: Acyclovir 400mg 5x/day, famciclovir 250mg TID, valacyclovir 1000mg BID Viral Conjunctivitis • Common viruses: ▫ Varicella Zoster Virus © 2013 American Academy of Ophthalmology Viral Conjunctivitis • Common viruses: ▫ Varicella Zoster Virus Virus reactivates in 20% of infected individuals 15% of all reactivations occur in CN V1 distribution (Herpes zoster ophthalmicus) Of those, 70% have ocular involvement Hutchinson’s sign (nasociliary branch of CN V1) Vesicular eruption on face, scalp eyelids + typical viral conjunctivitis features + pseudodendrite lesions on cornea (look very similar to HSV dendrites) Viral Conjunctivitis • Common viruses: ▫ Varicella Zoster Virus Treatment with oral antivirals within 72 hours reduces viral shedding, decreases incidence and severity of ocular complications and reduces risk of post-herpetic neuralgia Treat for 7-10 days with one antiviral: Acyclovir 800mg 5x/day, famciclovir 500mg TID, valacyclovir 1000mg TID (essentially double the dose for HSV) Refer to ophthalmology! Acute Bacterial Conjunctivitis • Typically unilateral (can become bilateral) • Far less common than viral conjunctivitis in adults • Acute = <4 weeks duration • Symptoms: ▫ Diffuse hyperemia, sticky white, green, or yellow discharge, eyelids/lashes stuck together on awakening, mild eye pain and foreign body sensation, intermittent blurry vision • Signs: ▫ Diffuse conjunctival injection, normal vision, normally reactive pupils, mucopurulent discharge, eyelid edema, papillary reaction Acute Bacterial Conjunctivitis http://www.optometry.co.uk/clinical/details?aid=718 © 2013 American Academy of Ophthalmology • Common pathogens: S.aureus, S. pneumoniae, H. influenzae, Moraxella Acute Bacterial Conjunctivitis • Gonococcal Conjunctivitis (Hyperacute) ▫ If hyperacute onset (12-24 hrs) and severe mucopurulent discharge consider Gonococcal conjunctivitis ▫ GC is often more painful, with more chemosis, can have decreased vision ▫ GC can invade and perforate the cornea very quickly! need immediate referral to ophthalmology if GC conjunctivitis is suspected! ▫ Culture the discharge! If positive, will require systemic antibiotic treatment & chlamydia coverage. Acute Bacterial Conjunctivitis • Gonococcal Conjunctivitis (Hyperacute) © 2013 American Academy of Ophthalmology Acute Bacterial Conjunctivitis • Treatment of Non-Gonococcal Conjunctivitis ▫ Most uncomplicated acute bacterial conjunctivitis is self-limited (most improve by 1 week) ▫ Supportive Measures: eye irrigation, artificial tears; NO patching! ▫ Many options for empiric treatment, prefer drops vs ointments ▫ Suggested Antibiotics: 4-6x daily for 5-7 days Polymixin B/ trimethoprim – topical hypersensitivity uncommon, great coverage (even H. influenzae), cheap! Fluoroquinolones: Ciprofloxaxin, Ofloxacin, Moxifloxacin – excellent coverage, well tolerated, more expensive Acute Bacterial Conjunctivitis • Treatment of Non-Gonococcal Conjunctivitis ▫ Consider immediate vs delayed antibiotics Quicker recovery vs increasing resistance Regardless of strategy, need follow-up in 2-3 days If not improving by day 4 of symptoms, start antibiotics ▫ These patients need immediate coverage: Healthcare workers Immunocompromised, hospitalized Contact lens wearers Unlikely to follow up or unreliable ▫ May consider delayed coverage in low-risk patients with expected reliable follow-up General Tips: Treating Conjunctivitis • If patient is a contact lens wearer no use of contact lenses ▫ Trap allergens to ocular surface if allergic conjunctivitis ▫ Increase risk of keratitis /corneal ulcers in microbial conjunctivitis which may be CL-related…discontinue use for at least 2 weeks • Follow-up for bacterial conjunctivitis should be frequent until patient is definitely improving • Immediate referral for: HSV or VZV conjunctivitis, suspected Gonococcal or hyperpurulent conjunctivitis, severely immunocompromised patients, neonates, any corneal involvement • If patient is not improving in expected amount of time with appropriate therapy refer! Subconjunctival Hemorrhage • Symptoms/History: ▫ Red eye, otherwise usually asymptomatic, normal vision ▫ Ask about history of minor trauma, Valsalva or straining, uncontrolled HTN, antiplatelet or anticoagulant use • Signs: ▫ Frank blood under the conjunctiva, often sectoral, occasional elevation of the conjunctiva Subconjunctival Hemorrhage • Like a bruise, will resolve in 2-3 weeks • If on anticoagulants, check INR • If recurrent un-provoked hemorrhages, workup for bleeding disorder • If no view of the sclera, decrease in vision, or history of significant trauma, refer to ophthalmology immediately! Corneal Abrasion © 2013 American Academy of Ophthalmology • History ▫ Mechanism of Injury? Vegetable matter? Fingernail? ▫ Contact lens wearer? Corneal Abrasion • Symptoms: ▫ Sharp pain, foreign body sensation, discomfort with blinking, photophobia, tearing, history of minor trauma • Signs: ▫ Epithelial defect that stains with fluorescein, clear underlying corneal stroma, conjunctival injection, mild eyelid edema • Exam: ▫ ▫ ▫ ▫ Topical anesthetic helpful for exam (do not prescribe!) Must examine with fluorescein Evert eyelids to look for foreign body Note size of abrasion & location (central vs peripheral) Corneal Abrasion • Treatment: ▫ Topical antibiotic Ointments provide more lubrication (erythromycin, bacitracin, polymixin B/bacitracin), use q2-4 hours Drops are associated with less blurry vision (trimethoprim/polymixin B), use QID ▫ If contact lens wearer: no CL use until 1 week after eye feels comfortable Must cover for Pseudomonas with a topical fluoroquinolone at least QID ▫ If fingernail or vegetable matter caused abrasion: Cover with a fluoroquinolone at least QID Corneal Abrasion • Treatment: ▫ Follow up in 2-3 days to ensure abrasion is healed, consider sooner if the abrasion is large or central ▫ If contact lens wearer, continue antibiotic for 2 days after epithelial defect is healed ▫ Patching is not recommended! ▫ If abrasion is not healed in 3 days, refer! ▫ Counsel patient about protective eyewear! Corneal Foreign Body • Symptoms: same as for corneal abrasion • Signs: visible foreign body on corneal surface, no distortion of pupil, no vision loss, no visible FB in the anterior chamber, no hyphema • History: determine type of FB, velocity of injury, contact lens use? © 2013 American Academy of Ophthalmology Corneal Foreign Body • Exam: ▫ Must check vision! ▫ Complete anterior segment exam ▫ Ensure no pupillary distortion or hyphema – could indicate penetrating, intraocular foreign body ▫ Give topical anesthetic ▫ Use fluorescein to help visualize ▫ If no penetrating injury, and not a high-velocity injury, can attempt to remove FB ▫ Evert eyelids to inspect for trapped FB Corneal Foreign Body • Methods of Removal ▫ Saline irrigation ▫ Under magnified visualization (loupes), gently roll FB off of corneal surface with anesthetic-moistened cotton tip applicator (Don’t push it in!) ▫ Corneal foreign body spud is an excellent tool! ▫ If you are comfortable and patient reliable, with magnification, attempt to use small-gauge (20-25G) short needle on a syringe with bevel away from cornea to dislodge FB Corneal Foreign Body • Any residual rust ring from metallic FB needs removal refer • Antibiotic coverage following corneal abrasion guidelines, prefer ointment, need more coverage than erythromycin • If any corneal infiltrate / clouding refer • Follow-up in 2 days to ensure no signs of infection • Counsel regarding protective eyewear! Corneal Ulcer / Keratitis Refer! • Symptoms/History ▫ Red eye, pain, decreased vision, photophobia, discharge ▫ Poor contact lens hygiene © 2013 American Academy of Ophthalmology High risk of permanent vision loss, perforation, loss of the eye! If you see anything like this, refer to ophthalmology immediately!! © 2013 American Academy of Ophthalmology Episcleritis • Symptoms/History: ▫ Red eye, mild if any pain, often history of recurrent episodes, often young patients, no discharge • Signs: ▫ Sectoral, occasionally diffuse hyperemia, deeper than conjunctiva, engorged radially oriented episcleral vessels, normal vision ▫ If nodular redness, can move the area with anesthetic moistened cotton tip applicator (anesthetize patient too!) Episcleritis • Etiology: typically idiopathic, may be associated with VZV (by history), recurrent may be associated with gout, collagen vascular disease, rosacea • Treatment: ▫ Condition is self-limited (days to weeks) ▫ Supportive treatment with artificial tears and oral NSAIDs if patient has discomfort ▫ Refer to ophthalmology if recurrent episodes Conjunctivitis vs Episcleritis vs Scleritis All images: © 2013 American Academy of Ophthalmology Scleritis Refer! • Symptoms: ▫ Severe “boring” eye pain, red eye, decreased vision, often recurrent episodes • Signs: ▫ Injection of blood vessels at all levels (conjunctival, episcleral, scleral) with characteristic “violaceous hue”, ciliary flush, globe very tender to palpation, may have scleral thinning, if infectious, may have infiltrate, unable to move inflammed scleral vessels with cotton tip • Etiology: 50% associated with systemic disease (RA, Wegener, SLE, reactive arthritis, relapsing polychondritis, PAN, IBD, syphillis, gout), also infectious causes (TB, Pseudomonas, Lyme, etc.) Iritis / Iridocyclitis Refer • Symptoms: ▫ Blurred vision, mild to moderate pain with brow/retro-orbital ache, direct and consensual photophobia, tearing, red eye • Signs: ▫ Ciliary flush, anterior chamber cell and flare, no discharge, variable decreased vision • Etiology: ▫ Autoimmune (HLA-B27, Behçet’s + see scleritis list of causes) ▫ Infectious: TB, syphillis, Lyme, HSV, VZV ▫ Idiopathic, sarcoid • Do a great ROS! (rashes, sexual hx, arthritis patterns, ulcers, travel, etc.) Iritis / Anterior Uveitis Refer http://www.medscape.com/viewarticle/540129_2 http://drsobol.com/Default.aspx?blogcategory=Cases http://www.cyberounds.com/cmecontent/art281.html?pf=yes Chemical Injury • Your management could be sight or eye-saving! • Signs: ▫ minimal to complete epithelial defect, chemosis, hyperemia, conjunctival/episcleral blanching (severe), corneal edema/opacification, moderate to severe anterior chamber cell/flare, increased intraocular pressure, burns on eyelids/surrounding skin • Alkali burns are worse than acidic burns • Ask if patient has a label from the chemical product Chemical Injury • Management (Contraindication = ruptured globe) ▫ Emergent irrigation (always neutral fluid like saline, sterile water, or LR) for at least 30 minutes ▫ Evert eyelids and irrigate, may need to swab conjunctival fornices ▫ Check pH with litmus paper (target is 7.0 to 7.4), any higher, continue irrigation ▫ May require up to 10 liters of irrigation! ▫ Once pH neutralized, apply antibiotic ointment (erythromycin) and prescribe q1-2 hours ▫ Oral pain medication ▫ Urgent ophthalmology referral, need daily monitoring Chemical Injury © 2013 American Academy of Ophthalmology https://www.proceduresconsult.jp/Home/ProcedureListing/ProcedureDetails/tabid /74/c/379/language/en-US/Default.aspx http://www.morganlens.com/ © 2013 American Academy of Ophthalmology Preseptal and Orbital Cellulitis • Presentation of both: tender, erythematous, edematous, warm periorbital tissues • Orbital cellulitis: concern when there is marked conjunctival injection with chemosis, pain with eye movement, restricted motility, diplopia, blurred vision, proptosis, fever • Clinical diagnosis, but may CT if uncertain © 2013 American Academy of Ophthalmology http://emedicine.medscape.com/article/1217858-overview Preseptal and Orbital Cellulitis • Treatment ▫ Preseptal cellulitis: mild, afebrile 10 days oral antibiotics (amoxicillin/clavulanate, trimethoprim/sulfamethoxazole, doxycycline, clindamycin) Daily follow-up until consistent improvement seen, then every 2-4 days until resolved ▫ Preseptal cellulitis: more severe, toxic-appearing, resistant to therapy, or less than 5 yrs of age Hospitalize for IV antibiotics (Vancomycin + Gm- coverage) Daily follow-up, involve ophthalmology ▫ Orbital cellulitis: same as severe preseptal Acute Angle Closure Glaucoma • Symptoms: ▫ Typically sudden onset, unilateral severe aching or throbbing pain, blurred vision, photophobia, halos around lights, nausea/vomiting • Signs: ▫ Fixed, mid-dilated pupil, diffuse injection, diffusely hazy/“steamy” cornea, flat or shallow anterior chamber, very high IOP (eye feels hard) • Treatment: Emergent ophthalmology referral (call the provider and discuss treatment measures you can initiate while the patient is on their way) • Know the patient’s visual acuity, helpful if you can check a pressure Acute Angle Closure Glaucoma This can blind or seriously impair vision in your patient! http://shop.onjoph.com/catalog/popup_image.php?pID=3791 From: Conjunctivitis: A Systematic Review of Diagnosis and Treatment JAMA. 2013;310(16):1721-1730. doi:10.1001/jama.2013.280318 Figure Legend: Selected Nonconjunctivitis Causes of Red Eyea Date of download: 3/27/2014 Copyright © 2014 American Medical Association. All rights reserved. References CONTENT SOURCES • American Academy of Ophthalmology. Basic and Clinical Science Course: External Disease and Cornea. Section 8. San Francisco: AAO; 2013. • American Academy of Ophthalmology. Basic and Clinical Science Course: Fundamentals and Principles of Ophthalmology. Section 2. San Francisco: AAO; 2012. • American Academy of Ophthalmology. Basic and Clinical Science Course: Orbit, Eyelids, and Lacrimal System. Section 7. San Francisco: AAO; 2012. • American Academy of Ophthalmology. Preferred Practice Patterns. Blepharitis. http://one.aao.org/preferred-practicepattern/blepharitis-ppp--2013. Accessed March 29, 2014. • American Academy of Ophthalmology. Preferred Practice Patterns. Conjunctivitis. http://one.aao.org/preferred-practicepattern/conjunctivitis-ppp--2013. Accessed March 29, 2014. • American Academy of Ophthalmology. Preferred Practice Patterns. Dry Eye Syndrome. http://one.aao.org/preferredpractice-pattern/dry-eye-syndrome-ppp--2013. Accessed March 29, 2014 • Azari AA, Barney NP. Conjunctivitis: A Systematic Review of Diagnosis and Treatment. JAMA. 2013;310(16):1721-1730. • Cronau H, Kankanala RR, Mauger T. Diagnosis and management of red eye in primary care. Am Fam Physician. 2010 Jan 15;81(2):137-44. • Gerstenblith AT and Rabinowitz MP (Eds.). (2012). The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. Sixth ed. Philadelphia, PA: Lippincott Williams & Wilkins. • Leibowitz HM. The Red Eye. N Engl J Med. 2000; 343:345-351 MULTIPLE IMAGE SOURCES • American Academy of Ophthalmology ONE Image Collection http://one.aao.org/browse-multimedia?filter=image • EyeRounds: Online Atlas of Ophthalmology – University of Iowa http://webeye.ophth.uiowa.edu/eyeforum/atlas/index.htm • Digital Reference of Ophthalmology. http://dro.hs.columbia.edu • Wills Eye Hospital Health Library. “Dry Eye Syndrome” http://www.willseye.org/health-library/dry-eye-syndrome SOURCES AS CITED WITH IMAGES • Encyclopaedia Iranica. FĀRESĪ, KAMĀL-AL-DĪN ABU’L-ḤASAN MOḤAMMAD. http://www.iranicaonline.org/articles/faresi-2 • http://www.opsweb.org/?page=Externaleye • http://www.nlm.nih.gov/medlineplus/ency/imagepages/19662.htm • https://lombartinstrument.com/product.php?productid=16843&cat=249&bestsel ler=Y • http://www.optometrial.com/direct-ophthalmoscope-oph8c-pocket-type • http://www.scrubshopper.com/products/2729-disposable-penlight-with-pupilguage • http://emedicine.medscape.com/article/82717-overview#showall • http://www.eyesite4u.net/uploaded/3913/d9b91439-71fd-45c6-a562f59d5e584b5especialty_eyechart.jpg • http://www.emedicinehealth.com/dry_eye_syndrome/page17_em.htm • http://en.wikipedia.org/wiki/Naked_eye • http://www.optometricmanagement.com/articleviewer.aspx?articleid=102506 • http://www.improveeyesighthq.com/blepharitis.html • http://patienteducationcenter.org/articles/blepharitis/ • http://eyewiki.aao.org/Sebaceous_carcinoma • http://www.hindawi.com/journals/joph/2010/423672/fig4/ • http://www.optometry.co.uk/clinical/details?aid=718 • http://www.medscape.com/viewarticle/540129_2 • http://drsobol.com/Default.aspx?blogcategory=Cases • http://www.cyberounds.com/cmecontent/art281.html?pf=yes • http://www.morganlens.com/ • https://www.proceduresconsult.jp/Home/ProcedureListing/ProcedureDetails/ta bid/74/c/379/language/en-US/Default.aspx • http://emedicine.medscape.com/article/1217858-overview • http://shop.onjoph.com/catalog/popup_image.php?pID=3791