* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Unit III Structures to ID
Survey
Document related concepts
Transcript
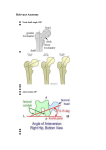
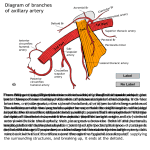
ID Guide & Notes for Unit 3 Anatomy Practical Lab 1: Surface Anatomy, Skeleton of Thorax, Intercostal Space/Muscles, Removal of Thoracic Wall, Pleural Cavities, and Lungs Thorax: Functions to protection vital organs while maintaining flexibility for respiration, achieved by alternating arrangement of ribs and intercostal muscles Surface Anatomy and Skeleton of Thorax: Sternum: Jugular/suprasternal notch, manubrium, sternal angle, body, xiphoid process o Sternal angle—@ attachment of 2nd costal cartilage and level of T4/T5 IV disc Scapula: Acromion, coracoid process Sternoclavicular and acromioclavicular joints Costal margin—The lower edge of the thorax formed by the bottom edge of the rib cage o Costal cartilages 7-10 join to form costal margin Anterior axillary fold—lateral border of the pec. major muscle Ribs—note that first rib is the highest, shortest, broadest, and most sharply curved rib o Head—articulates w/ 2 vertebral bodies & their IV disc (ribs 1,10-12 only articulate w/ 1TV body) o Neck o Tubercle—articulates w/ transverse costal facet on transverse process of its TV o Costal angle o Shaft o Costal groove o Costal cartilage—attached to anterior end of each rib o True ribs (1-7)—costal cartilage attached directly to sternum o False ribs (8-12)—costal cartilage not directly attached to sternum 8-10: attached to costal cartilage of rib above 11-12: floating ribs b/c cartilage ends in abdominal musculature, not skeleton Intercostal Space and Intercostal Muscles: Intercostal space: Interval between adjacent ribs; there are 11, #’d by rib that is sup. to space External intercostal muscle—att. to inf. border of rib above & sup. border of rib below o Elevates rib below o Fibers descend diagonally toward the ant. midline External intercostal membrane—at ant. end of intercostal space btwn. costal cartilages o Fibers of external intercostal muscle end at lateral edge of membrane Internal intercostal muscle—att. to sup. border of the rib below & inf. border of rib above o Depresses rib above o Fibers are perpendicular to external intercostal muscle Innermost intercostal muscle—same fiber direction, att.s, and action as internal intercostals o Does not extend as far anteriorly in intercostal space as internal intercostals Neurovascular bundle—run in plane between internal intercostal muscle and innermost intercostal muscle; from superior to inferior (VAN): o Posterior intercostal vein o Posterior intercostal artery o Intercostal nerve o NV bundle supplies intercostal muscles, skin of thoracic wall, & parietal pleura Removal of Thoracic Wall: Costal pleura—lines the internal surface of the anterior thoracic wall Transversus thoracis muscle—inf. origin on sternum & sup. insertion on costal cartilages 2-6 o Just adjacent to sternum o Depresses the ribs Internal thoracic vessels—cut at the 5th sternocostal joint, near lower end of sternum o Located between transversus thoracis and costal cartilages o Internal thoracic artery—runs vertically just lateral to border of sternum, crossing deep surfaces of costal cartilages Anterior intercostal branches: blood supply to anterior end of intercostal space Posterior to 6th or 7th costal cartilage, branches into: Superior epigastric artery Musculophrenic artery Pleural Cavities: Superior thoracic aperture (thoracic inlet)—bounded by manubrium, first rib, & body of TV1 o Trachea, esophagus, [X], thoracic duct, major blood vessels all pass btwn. thorax, neck, and upper limb via the thoracic inlet Inferior thoracic aperture (thoracic outlet)—bounded by xiphisternal joint, costal margin, ribs 11-12, & body of TV12 o Diaphragm att. to boundary structures Separates thoracic cavity from abdominal cavity Aorta, thoracic duct, inferior vena cava, esophagus, [X] all pass btwn. thorax and abdomen via openings in diaphragm Mediastinum—Region btw. the pleural cavities o Contains heart, aorta, trachea, & esophagus as they pass to/from head and neck Pleural cavities—Occupy lateral parts of thoracic cavity; contain the lungs o Parietal pleura—serous membrane that lines pleural cavities Costal pleura—lines inner surface of thoracic wall Mediastinal pleura—lines mediastinum Diaphragmatic pleura—lines superior surface of diaphragm Cervical pleura (cupula)—extends superior to first rib; covers apex of lung o Lines of pleural reflection—acute folds where inner surfaces of parietal plurae contact one another Costomediastinal recess—posterior to sternum @ costal/mediastinal pleural junction Costodiaphragmatic recess—most inf. limits of parietal pleura Lung does not extend into this recess during quiet inspiration o Endothoracic fascia—connective tissue that attaches costal pleura to thoracic wall o Visceral (pulmonary) pleura—directly covers lung Continuous w/ mediastinal pleura @ root of lung Pulmonary ligament—extends inferior to root of lung o Pleural cavity is potential space btwn. visceral and parietal pleurae Lung Root of the lung—pulmonary vessels and main bronchus can be felt w/in Lung surfaces—costal, mediastinal, & diaphragmatic o Costal surface is only surface visible in situ Borders of lung—anterior, posterior, and inferior Lung fissures: o Oblique (major) fissure—lies deep to 5th rib laterally & deep to 6th costal cartilage anteriorly Separates superior/inferior lobes on both lungs o Horizontal (minor, transverse) fissure—deep to 4th rib and 4th costal cartilage on right lung Defines middle lobe; on right lung only Lung lobes: o Right—superior, inferior, & middle o Left—superior & inferior Cardiac notch—on ant. border of superior lobe of left lung; ant. to heart Lingula—inferomedial portion of superior lobe of left lung; homolog of middle lobe of right lung o Most of inferior lobe is post. in thorax & most of superior lobe is ant. in thorax Apex—ant. to neck of 1st rib/sup. to body of 1st rib o Apex & cervical pleura lay sup. to plane of thoracic inlet Contact impressions—on mediastinal surface of each lung; illustrate close proximity of mediastinal structures to lung o On right lung: Cardiac impression Esophagus impression Arch of azygos vein impression Superior vena cava impression o On left lung: Cardiac impression Aortic arch impression Thoracic aorta impression Hilum—region on mediastinal surface where structures in root of lung enter/leave o Main bronchus—post. to pulmonary vessels; look for cartilage in its wall o Pulmonary artery—sup. to pulmonary veins o Pulmonary vein—inf. to artery; thinner vessel walls than in artery o Lymph nodes and vessels o Autonomic nerve fibers Bronchial artery—on surface of main bronchus o Lumen may be seen where main bronchus cut during lung removal Anterior & Posterior pulmonary plexuses—supply lungs SS nerve supply to lung—from right/left sympathetic trunks Phrenic nerve—passes ant. to root of lung & medial to mediastinal pleura Pericadiacophrenic vessels—passes. ant. to root of lung & medial to mediastinal pleura [X]—passes post. to root of lung o Provides PS innervation to lung Pericardium—contains heart; occupies midline btwn. lungs Mediastinum Region btwn. pleural cavities Boundaries: o Superior—thoracic inlet o Inferior—diaphragm o Anterior—sternum o Posterior—bodies of TV1-12 o Lateral—Mediastinal pleurae Superior mediastinum—sup. to plane of sternal angle; btwn. manubrium & bodies of TV1-4 Inferior Mediastinum—inf. to plane of sternal angle; divided by pericardium into: o Anterior mediastinum—btwn. sternum & pericardium Contains part of thymus in children/adolescents o Middle mediastinum—contains pericardium, heart, and roots of great vessels o Posterior mediastinum—post. to pericardium & ant. to bodies of TV5-12 Contains esophagus, [X], azygos system of veins, thoracic duct, & thoracic aorta as they pass btwn. neck, thorax, & abdomen Plane of sternal angle—marks level of: o Superior border of pericardium o Bifurcation of trachea o Beginning & end of arch of aorta o End of ascending aorta & beginning of thoracic aorta Mediastinal pleura—from ant. to post., it contacts: o Pericardium and root of lung o Esophagus (right side) o Thoracic aorta (left side) o Becomes costal pleura posteriorly where it contacts sides of TV bodies Endothoracic fascia—cleavage plane for separation of costal pleura from thoracic wall Phrenic nerves—btwn. mediastinal pleura & pericardium, ant. to root of lung o Only motor innervation to half of the diaphragm Pericardiacophrenic vessels—small branch of the internal thoracic artery; originates @ level of lower margin of the manubrium o Runs with the phrenic nerve Lab 2: Middle Mediastinum, External/Internal Heart Middle Mediastinum: contains pericardium, heart, and roots of great vessels Pericardium is a sac that encloses the heart o Pierced by great vessels: aorta, pulmonary trunk, SVC & IVC, and 4 pulmonary veins o Outer surface is fibrous, inner surface is serous/smooth o Attached to central tendon of diaphragm: pericardium and heart move during respiration Heart in the Thorax/Removal of the Heart Superior vena cava Inferior vena cava Ascending aorta Arch of aorta Pulmonary trunk 4 pulmonary veins Ligamentum arteriosum—connects left pulmonary artery to arch of aorta Left vagus nerve—crosses left side of aortic arch o Left recurrent laryngeal nerve—inf. to aortic arch & post. to ligamentum arteriosum Chambers seen from anterior view: o Right atrium o Right ventricle Forms most of anterior surface of heart o Left ventricle Borders of the heart: right, inferior, & left borders easily seen on chest radioraph o Right border—formed by right atrium o Inferior border—formed by right ventricle & small part of left ventricle o Left border—formed by left ventricle o Superior border—formed by right/left atria & auricles Not easily seen on chest radiograph Apex of heart—part of left ventricle o Normally deep to left 5th intercostal space Base of heart—left atrium & part of right atrium; or area of great vessel emergence Parietal layer of serous pericardium—smooth/shiny lining of inner surface of pericardium Visceral layer of serous pericardium—reflection of parietal layer that is on surface of heart o Line of reflection of parietal-visceral pericardium occurs @ roots of great vessels Pericardial cavity—potential space btwn. parietal & visceral layers o Contains a thin film of lubricating serous fluid to allow free movement of heart in pericardium Oblique pericardial sinus—blind sac btwn. pulmonary veins where visceral pericardium doesn’t touch heart Transverse pericardial sinus—just inferior to great vessels & superior to pulmonary veins External Features of the Heart Coronary (atrioventricular) sulcus—separates atria from ventricles Anterior/posterior interventricular sulcus—indicate location of interventricular septum o Join coronary sulcus at a right angle Surfaces of the heart: o Sternocostal (ant.) surface—mainly right ventricle o Diaphragmatic (inf.) surface—mainly left ventricle & a little right ventricle o Left pulmonary surface—mainly left ventricle; contacts cardiac impression of left lung o Right pulmonary surface—mainly right atrium Chambers: right atrium/auricle, right ventricle, left ventricle, left atrium/auricle In superior view: o Aorta and aortic valve, pulmonary trunk and pulmonary valve, & superior vena cava Diaphragmatic surface: o Opening of inferior vena cava & posterior interventricular surface Vessels of heart—located between visceral pericardium & muscular wall of heart Coronary sinus—on diaphragmatic surface of heart in the coronary sulcus o Opens into right atrium o Receives cardiac veins—veins are superior to coronary arteries Great cardiac vein—near superior end of sinus Middle cardiac vein—in posterior interventricular sulcus Small cardiac vein—near inferior end of sinus; courses along inf. border of heart Anterior cardiac veins—bridge atrioventricular sulcus btwn. right atrium/ventricle o Drains anterior wall of right ventricle directly into right atrium o Passes superficial to right coronary artery Aortic valve—in lumen of the ascending aorta o Right, left, & posterior semilunar cusps o Aortic sinuses—small pockets behind each valve cusp Opening of left coronary artery—in left aortic sinus Opening of right coronary artery—in right aortic sinus Left coronary artery—begins btwn. left auricle & pulmonary trunk; is short; divides in coronary sulcus: o Anterior interventricular branch—runs in anterior interventricular sulcus to apex of heart Also known as left anterior descending (LAD) artery Accompanies great cardiac vein o Circumflex branch—runs in coronary sulcus & around left border of heart Branches supply posterior wall of left ventricle (such as obtuse marginal branches) Accompanies coronary sinus in the coronary sulcus Right coronary artery—begins btwn. right auricle & ascending aorta in coronary sulcus o Anterior right atrial branch—arises close to origin of RCA Ascends along ant. wall of right atrium towards SVC Gives off sinuatrial (S.A.) nodal branch—supplies S.A. node o Right marginal branch—arises near inf. border of heart Accompanies small cardiac vein along inf. border o Posterior interventricular branch—arises in posterior interventricular sulclus Courses along post. IV sulcus to apex of heart Anastomoses w/ ant. IV branch of LCA Accompanies middle cardiac vein o Artery to the atrioventricular node—arises from RCA @ crux of heart Crux is point where IV sulcus meets coronary sulcus Internal Features of the Heart Right atrium Inner surface of anterior wall: o Pectinate muscles—horizontal ridge of muscle o Crista terminalis—vertical ridge of muscle that connects the pectinate muscles Posterior wall: o Opening of SVC o Opening and valve (valvule) of ICA o Opening and valve (valvule) of coronary sinus o Fossa ovalis & limbus of fossa ovalis—remnant of fetal foramen ovale Conducting system of heart—in the walls, but are not visible o Sinuatrial (SA) node—@ sup. end of crista terminalis, at junction btwn. right atrium & SVC o Atrioventricular (AV) node—in interatrial septum, above opening of coronary sinus Opening of right atrioventricular valve—leads into right ventricle Right ventricle Interventricular septum Opening of right atrioventricular valve (tricuspid)—has 3 cusps: o Anterior, septal, & posterior Chordae tendineae—pass from valve cusps to apices of papillary muscles o Attach to adjacent sides of two valve cusps Papillary muscles—arise from walls of right ventricle o Anterior, septal, & posterior Anterior papillary muscle is largest Spetal papillary is small and may be multiple Trabeculae carneae—muscular ridges that roughen inner surface of wall Septomarginal trabecular (moderator band)—extends from IV septum to base of ant. papillary muscle o Contains part of the right bundle of conducting system, which stimulates ant. papillary muscle Opening of the pulmonary trunk o Conus arteriosus (infundibulum)—cone-shaped portion of ventricle inf. to opening of trunk Its inner wall is smooth Pulmonary valve—consists of 3 semilunar cusps—anterior, right, & left o Prevents backflow of blood during diastole o Each cusp has 1fibrous nodule & 2 lunules—help seal cusps Left Atrium 4 pulmonary veins—openings on post. surface of heart o Arranged in pairs: 2 from right lung, 2 from left long Inner surface of atrial wall is smooth; inner surface of auricle is roughened by pectinate muscles Valve of the foramen ovale—on interatrial septum Opening into left auricle Opening of the left atrioventricular valve Left Ventricle Aortic valve—has 3 semilunar valve cusps: o Posterior, right, & left cusps Each cusp has 1 nodule & 2 lunules Left atrioventricular valve (bicuspid/mitral)—has 2 cusps: o Anterior & posterior cusps Anterior & posterior papillary muscles—chordae tendineae of each muscle attach to both valve cusps Trabeculae carneae—muscular roughening of the inner surface of the ventricular wall Muscular part of interventricular septum—much thicker than membranous part Membranous part of interventricular septum—inf. to attachment of right cusp of aortic valve Openings of the coronary artieres—LCA begins in left aortic sinus, RCA begins in right aortic sinus o Posterior cusp of aortic valve aka noncoronary cusp b/c no coronary artery arises from its sinus Conducting system of the heart—are not visible o AV node—receives impulses from SA node after they pass through wall of right atrium AV bundle—receives impulses originating in AV node through membranous IV septum Right and left bundles—divisions of AV bundle on either side of IV septum; stimulate ventricles to contract Lab 3: Superior/Posterior Mediastinum Superior mediastinum—its structures pass btwn. thorax-neck or thorax-upper lumb Boundaries: o Superior—superior thoracic aperture o Posterior—bodies of T1-T4 o Anterior—manubrium o Lateral—left/right mediastinal pleurae o Inferior—plane of sternal angle Thymus—will be a fatty mass post. to manubrium; only a remnant of gland remains after puberty Superior vena cava—formed post. to inf. border of right 1st costal cartilage o Passes ant. to root of lung Left and right brachiocephalic veins—meet to form SVC Azygos vein—right side o Arch of azygos vein passes sup. to root of right lung; drains into post. surface of SVC Right/left phrenic nerves—note that they pass post. to brachiocephalic veins o Pass ant. to roots of lungs, run w/ pericardiacophrenic vessels, & enter sup. surface of diaphragm Arch of aorta—begins/ends @ level of sternal angle o Branches: from ant. to post. Brachiocephalic trunk Left common carotid Left subclavian Ligamentum arteriosum—fibrous cord connecting concavity of arch of aorta to left pulmonary artery Left vagus—passes post. to root of lung toward esophagus o Left recurrent laryngeal—inf. to aortic arch & post. to ligamentum arteriosum Right vagus nerve—passes post. to root of lung o Right recurrent laryngeal—loops around right subclavian artery Trachea—ant. to the esophagus o Bifurcation—@ plane of sternal angle Right main bronchus—arch of azygos vein passes superiorly Larger in diameter, shoter, and more vertical than left main bronchus Left main bronchus—arch of aorta passes superiorly Carina—ridge of cartilage inside bifurcation; usually slightly left of median plane Tracheobronchial lymph nodes—located around trachea near bifurcation Tracheal rings—C-shape w/ open part posterior Esophagus—post. to trachea; closely related to open part of tracheal cartilages Posterior Mediastinum—its strctures pass btwn. thorax-abdomen; post. to pericardium Boundaries: o Superior—plane of sternal angle o Posterior—bodies of TV5-TV12 o Anterior—pericardium o Lateral—left/right mediastinal pleurae o Inferior—diaphragm Esophagus—muscular tube sitting just right of midline o Lies post. to LA and part of LV o Esophageal plexus of nerves—covers surface & innervates inf. portion Right vagus nerve—fibers spread out on surface of esophagus Left vagus nerve—fibers contribute to plexus o Ant./Post. vagal trunks—on inf. part of esophagus just sup. to diaphragm Formed by esophageal plexus & innervate large portion of GI tract Pass through diaphragm w/ esophagus Thoracic aorta—lies left and slightly post. to esophagus o Esophageal aa. & bronchial aa.—small, unpaired; arise from ant. surface of aorta o Posterior intercostal arteries—right aa. cross midline on ant. surface of vertebral bodies Right aa. pass post. to all other contents of post. mediastinum Azygos vein—arches sup. to root of right lung o Posterior intercostal veins—azygos tributaries on right side Thoracic duct—btwn. azygos vein & thoracic aorta; left of vein & post. to esophagus o Passes through diaphragm w/ thoracic aorta o Terminates by draining into junction of left IJV & left subclavian vein o Crosses ant. surface of right post. intercostal aa., hemiazygos v., & acc. hemiazygos v. Hemiazygos & accessory hemiazygos veins—on left side of post. mediastinum o Drain left post. intercostal veins o Cross bodies of TV8 (hemiazygos) & TV9 (accessory hemiazygos) o Drain into azygos vain Intercostal nerve—will disappear post. to innermost intercostal muscle Sympathetic trunk—crosses heads of ribs 2-9, then inferiorly, lies more ant. on sides of vertebral bodies o Sympathetic ganglion—1 for each thoracic vertebral level Rami communicantes—connect intercostal nerves w/ corresponding thoracic sympathetic ganglia o White & gray rami—can’t distinguish based on color; white rami are more lateral than gray Greater splanchnic nerve—on sides of vertebral bodies T5-T9; receives contributions from SG 5-9 o Sympathetic trunk is post. to greater splanchnic nerve Lesser splanchnic nerve—from SG 10-11 Least splanchnic nerve—from SG 12 Lab 4: Surface Anatomy, Superficial Fascia, Muscles of Abdominal Wall, Inguinal Region Abdomen: portion of trunk btwn. thorax and pelvis; diaphragm separates it from thoracic cavity; continuous with pelvic cavity Surface Anatomy Xiphoid process Costal margin Pubic symphysis Pubic crest Pubic tubercle Anterior superior iliac spine Tubercle of iliac crest Quadrant system: divided by transumbilical plane and median plane into: o Right upper, left upper, right lower, & left lower quadrants Regional system: divided by midclavicular lines, subcostal plane, & transtubercular plane into: o R/L hypochondriac, epigastric, R/L lumbar, umbilical, R/L inguinal, & hypogastric Superficial Fascia Camper’s fascia—fatty; most superficial layer Scarpa’s fascia—membranous, deeper layer; att. to fascia lata of thigh & continuous w/ fascias in perineum Superficial epigastric atery & vein—slightly lateral to midline in superficial fascia Anterior cutaneous nerves—enter fascia just lateral to midline o They branch off different nerves depending on spinal level: Intercostal nerves—T7-11 T7 innervates skin superficial to xiphoid (Grant’s says T6, Dr. Ireland says T7) Subcostal nerve—T12 Innervates skin superior to pubic symphysis Iliohypogastric & ilioinguinal nerves—L1 Innervates skin overlying pubic symphysis Lateral cutaneous nerves—enter fascia near midaxillary line Muscles of Anterolateral Abdominal Wall & Inguinal Region Skeleton of abdominal wall: xiphisternal junction, xiphoid process, costal margin, pubic symphysis, pubic crest, pubic tubercle, anterior superior iliac spine, iliac crest, & tubercle of iliac crest External oblique muscle—fibers run superolateral to inferomedial Origin: external surfaces of ribs 5-12 Insertion: aponeurosis on linea alba, pubic tubercle, & ant. half of iliac crest Superficial inguinal ring—opening in aponeurosis; passage for spermatic cord/round ligament of utuerus External oblique aponeurosis—ant. wall of abdominal cavity; has contributions to superficial inguinal ring: o Lateral (inf.) crus—forms lateral margin; att. to pubic tubercle o Medial (sup.) crus—forms medial margin; att. to pubic crest o Intercrural fibers—span superolateral to ring; prevent crura from spreading apart Inguinal ligament—inf. border of ext. oblique aponeurosis; spans from ASIS to pubic tubercle Vessels/nerves enter/exit abdominal cavity posteriorly Forms floor of abdominal cavity External spermatic fascia—fascia extending from ext. oblique aponeurosis onto spermatic cord Ilioinguinal nerve—branch emerges at superficial inguinal ring; ant. to spermatic cord/round ligament o Sensory innervation to skin on ant. surface of ext. genitalia & medial surface of thigh Lacunar ligament—medial end of inguinal ligament that turns posteriorly & att. to pecten pubis Internal oblique muscle—fibers ascend from inferolateral to superomedial (perpendicular to ext. oblique) Origin: thoracolumbar fascia, iliac crest, & lateral half of inguinal ligament Insertion: inferior borders of ribs 10-12, linea alba, pubic crest, & pecten pubis Lowest fibers arch over cord/round ligament (roof of inguinal canal) & form part of post. wall of inguinal canal as conjoint tendon Cremaster muscle & fascia—extension of int. oblique to coverings of spermatic cord o In females, this surrounds the round ligament of uterus Ilioinguinal nerve—runs through inguinal canal to emerge at superficial inguinal ring Iliohypogastric nerve—runs parallel & superior to ilioinguinal nerve Transversus abdominis muscle—deep to int. oblique w/ fibers in same direction Origin: int. surfaces of costal cartilages 7-12, thoracolumbar fascia, iliac crest, & lat. 1/3 of inguinal lig. Insertion: linea alba, pubic crest, & pecten pubis Ilioinguinal nerve—courses btwn. transversus abdominis & int. oblique Fibers surround inguinal canal—form part of roof; aponeurotic insertion form part of post. wall o Weakness in post. wall of inguinal canal: no muscle fibers inf. to transversus & int. oblique Deep inguinal ring—point where gubernaculum passed through transversalis fascia during development Transversalis fascia—fascia lining inner surface of abdominal muscles Ductus deferens passes through in males; round ligament of uterus passes through in females Located sup. to midpoint of inguinal ligament Inferior epigastric vessles—w/in layer of extraperitoneal fascia o Medial to deep inguinal ring o Ductus deferens/round ligament pass through this area Boundaries of inguinal canal: Deep—deep inguinal ring Superficial—superficial inguinal ring Anterior—aponeurosis of ext. oblique Inferior (floor)—inguinal ligament & lacunar ligament Superior (roof)—arching fibers of int. oblique & transversus abdominis Posterior—transversalis fascia laterally; conjoint tendon medially Rectus abdominis muscle—runs vertically to flex the trunk Origin: symphysis & body of pubis Insertion: costal cartilages 5-7 Rectus sheath—formed by aponeuroses of ext./int. obliques & transversus abdominis; contents: o Rectus abdominis, pyramidalis muscle, sup. & inf. epigastriac vessels, terminal ends of VR of spinal nerves T7-12 Tendinous intersections—firm attachments of ant. wall of rectus sheath to ant. surface of rectus muscle Pyramidalis muscle—if present, ant. to inf. end of rectus muscle; att. to ant. surface of pubis & linea alba o Function: draws down/tenses the linea alba Nerves T7-12—branches enter rectus sheath, penetrate deep surface surface of rectus muscle o Anterior cutaneous branches—emerged from muscle; termination of thoracic nerves Superior epigastric artery & vein—on sup. half of rectus muscle’s post. surface Inferior epigastric artery & vein—on inf. half of rectus muscle’s post. surface Arcuate line—inf. limit of post. wall of rectus sheath o Variable location midway btwn. pubic symphysis & umbilicis o Level where inf. epigastric vessels enter rectus sheath Transversalis fascia—inf. to arcuate line Parietal peritoneum—deep to transversalis fascia & deep to extraperitoneal fascia Linea alba—formed by fusion of aponeuroses of R/L ext. oblique, int. oblique, & transversus abdominis Lab 5: Reflection of Abdominal Wall, Peritoneum, & Peritoneal Cavity Reflections of Abdominal Wall Falciform ligament—connects ant. abdominal wall to liver; on inner surface of right upper quadrant flap Peritoneal folds—on inner surface of lower abdominal wall: o Median umbilical fold—midline inf. to umbilicis; contains urachus (remnant of allantoic duct) Att. to right lower quadrant flap o Medial umbilical fold—lateral to median fold; contains remnant of umbilical artery o Lateral umbilical fold—lateral to medial fold; overlies inf. epigastric vessels Deep inguinal ring—see markings of it as a small depression lateral to umbilical fold Peritoneum & Peritoneal Cavity Peritoneum: serous membrane that secrete fluid to lubricate movements of organs that it lines Parietal peritoneum—lines inner surfaces of abdominal & pelvic walls Visceral peritoneum—covers surfaces of abdominal & pelvic organs Peritoneal cavity—potential space btwn. 2 layers of peritoneum containing peritoneal fluid Peritoneal organs—developed in peritoneal cavity; suspended on a mesentery; include: o Stomach, 1st part of duodenum, jejunum, ileum, transverse colon, sigmoid colon, liver, spleen Retroperitoneal organs—developed behind peritoneum; include: o Kidneys, ureters, suprarenal glands, & rectum Secondary retroperitoneal organs—begin peritoneal in embryo & end retroperitoneal; include: o 2nd–4th parts of duodenum, pancreas, ascending colon, & descending colon Gastrointestinal tract Liver—right upper quadrant, across midline, to left upper quadrant; lies against inf. surface of diaphragm o Falciform ligament divides it into right & left lobes Gallbladder—right upper quadrant; extends below inf. order of liver o @ tip of right 9th costal cartilage in midclavicular line Stomach—left upper quadrant; cont. w/ esophagus prox. & duodenum dist.; ant. surface covered by liver Spleen—left upper quadrant; post. to stomach Greater omentum—att. to greater curvature of stomach to intestines Small intestine—begins @ pyloric end of stomach; has 3 parts: o Duodenum—post. to other parts of GI tract o Jejunum—extends from left upper quad. to right lower quad.; occupies all 4 quads o Ileum—extends from left upper quad. to right lower quad; occupies all quads Large intestine—begins in right lower quad @ ileocecal junction; has 6 parts: o Cecum—right lower quadrant Appendix—att. to inf. end of cecum o Ascending colon—right lower quadrant to right upper quadrant Right colic (hepatic) flexure—termination of ascending colon o Transverse colon—right upper quadrant to left upper quadrant Left colic (hepatic) flexure—termination of transverse colon o Descending colon—left upper quadrant to left lower quadrant o Sigmoid colon—left lower quadrant; ends in pelvic cavity @ SV3 o Rectum—in pelvis Visceral peritoneum—ID it on surface of stomach or small intestine; smooth, slippery Parietal peritoneum—ID on inner surface of abdominal wall; smooth, slippery Lesser omentum—lesser curvature of stomach & 1st part of duodenum to inf. surface of liver; terminal end: o Hepatoduodenal ligament—att. liver to 1st part of duodenum Falciform ligament—att. parietal peritoneum on ant. abdominal wall to visceral peritoneum on liver o Ligamentum teres hepatis (round ligament of liver)—remnant of umbilical vein in inf. edge of falciform lig. Coronary ligament—att. liver to diaphragm o Left/Right triangular ligaments—btwn. left/right lobes of liver & diaphragm Gastrophrenic ligament—connects sup. part of stomach’s greater curvature to diaphragm Gastrosplenic ligament—connects stomach’s greater curvature to spleen Splenorenal ligament—connects spleen to body wall ant. to left kidney Transverse mesocolon—att. ant. surface of duodenum & pancreas to body wall Phrenicocolic ligament—att. left colic flexure to diaphragm; @ left end of transverse mesocolon Mesentery—suspends jejunum & ileum from post. abdominal wall, from l. upper quad. to r. lower quad. Mesoappendix—att. appendix to post. abdominal wall; contains appendicular artery Sigmoid mesocolon—suspends sigmoid colon from post. abdominal wall Greater peritoneal sac—contains all the peritoneal structures listed above Lesser peritoneal sac (omental bursa)—post. to stomach & lesser omentum; smaller than greater sac o Inferior recess—lowest part of lesser sac; extends inf. as far as greater omentum o Superior recess—highest part of lesser sac; diaphgram is post.; caudate lobe of liver is ant. o Pancreas—post. to main part of lesser sac; peritoneal covering is part of post. wall of lesser sac Epiploic foramen (omental foramen)—connection of greater & lesser sacs; post. to hepatoduodenal ligament o Boundaries: Anterior—hepatic portal vien, hepatic artery proper, & bile duct w/in hepatoduodenal lig. Posterior—IVC & right crus of diaphragm, covered by parietal peritoneum Superior—caudate lobe of liver, covered by visceral peritoneum Inferior—1st part of duodenum, covered by visceral peritoneum Lab 6: Celiac Trunk, Stomach, Spleen, Liver, & Gallbladder: ID external parts of stomach: o Body, great./less. curvatures, cardia, cardial notch, fundus, body, angular notch, pyloric part, pylorus ID internal parts of stomach: o Gastric folds (rugae), pyloric antrum, pyl. canal, pyl. sphincter, pyl. orifice, ampulla of duodenum ID parts of liver: o Right/left lobes, diaphragmatic surface, inf. border o Visceral surface of liver—in contact with gallbladder & the peritoneum that covers stomach, duodenum, colon, right kindey & right suprarenal gland Porta hepatis—fissure through which vessels, ducts, lymphatics, & nerves enter/exit liver Hepatoduodenal ligament—free edge of lesser omentum; ant. border of epiploic foramen; contains: o Bile duct—most lateral in ligament Cystic duct Common hepatic duct—tributaries from left/right hepatic ducts, which exit porta hepatis o Hepatic artery proper—Branches in hepatoduodenal ligament: Left hepatic artery—terminal branch near porta hepatis Right hepatic artery—terminal branch near porta hepatis Cystic artery—to gallbladder; from right hepatic artery Right gastric artery—to lesser curvature of stomach o Right gastric artery o Hepatic portal vein—most posterior in ligament; passes post. to first part of duodenum Right & left portal veins—divide from portal vein in porta hepatis Left & right gastric veins—tributaries of hepatic portal vein o Autonomic nerves—surround the hepatic artery proper o Lymphatic vessels—hepatic lymph nodes Common hepatic artery—arises off celiac trunk; branches: o Hepatic artery proper o Gastroduodenal artery—passes post. to first part of duodenum; branches: Right gastro-omental artery Anterior superior pancreaticoduodenal artery Celiac trunk—arises from ant. abdominal aorta @ TV12; very short; branches: o Common hepatic artery o Left gastric artery o Splenic artery Left gastric artery—reaches stomach near esophagus; to lesser curvature; anastomosis w/ r. gastric a. Splenic artery—courses along sup. border of pancreas; branches: o Short gastric arteries—from distal end; supply fundus of stomach o Left gastro-omental artery—to greater curvature; anastomosis w/ r. gastro-omental a. Spleen—covered by visceral peritoneum except @ hilum (where splenic vessels enter/exit) o Diaphragmatic surface—smooth; related (through the diaphragm) to ribs 9-11 o Visceral surface of spleen—related to 4 organs: Stomach, left kindey, transverse colon/left colic flexure, & pancreas Liver o Right lobe—six times larger than left lobe o Inferior border—sharp; separates visceral surface from diaphragmatic surface o Bare area—on post. aspect of diaphragmatic surface o Coronary ligament—around the bare area o Visceral surface—contains H-shaped fissures/fossae that defines its 4 lobes: Right lobe, left lobe, caudate lobe, & quadrate lobe Ligamentum venosum & falciform ligament—occupy left fissure of “H” Gallbladder & IVC—occupy fossae that forms right side of “H” Porta hepatis—forms horizontal bar of “H” IVC—hepatic veins drain directly from liver o Right & left anatomical lobes—defined by falciform ligament division o Right & left functional lobes—defined by pattern of bile drainage/vascular supply o Path of lymphatic drainage: Hepatic lymph nodes—drains small lymph vessesl @ porta hepatis Celiac lymph nodes—lymph vessels follow hepatic arteries to nodes near celiac trunk Phrenic nodes—post. drainage of liver Gallbladder—occupies shallow fossa on visc. surface of liver; near tip of 9th costal cartilage in midclav. line o Fundus, body, & neck o Cystic artery—from right hepatic artery o Spiral fold—fold in mucosal lining of neck Cystic duct—drains gallbladder secretions; continuation of spiral fold Lab 7: SMA & Small Intestine, IMA & Large Intestine, Duodenum/Pancreas/Portal Vein Superior Mesenteric Artery (SMA)—arises from ant. surface of abd. aorta @ LV1 Post. to neck of pancreas @ origin Passes ant. to uncinate process, 3rd part of duodenum, & left renal v. Enters mesentery & courses towards terminal end of ileum in right lower quadrant Mesentery—its root is att. to post. abd. wall in a line from l. upper quad. to r. lower quad. Superior mesenteric plexus of nerves—dense ANS network surrounding BVs Branches of SMA: o Inferior pancreaticoduodenal artery—1st branch o Intestinal arteries—15-18 to the jejunum & ileum Arterial arcades—connect the intestinal arteries Jujunum only has only 1-2 arcades, so longer arteriae rectae than ileum Ileum has 4-5 arcades, so shorter arteriae rectae than jejunum Arteriae rectae (straight arteries)—straight terminal branches of intestinal arteries o Ileocolic artery—from right side of SMA & runs to right in a retroperitoneal position; branches: Appendicular artery—to appendix; runs in mesoappendix Ant./post. cecal arteries—to ant./post. cecum Ileal artery—to distal ileum Asc. colic artery—to ascending colon o Right colic artery—supplies ascending colon; from right side of SMA & runs right in retro. position Ascending branch Descending branch—anastomoses w/ asc. colic artery (branch of ileocolic a.) o Middle colic artery—supplies trans. colon; from ant. surface of SMA & courses through transverse mesocolon Right branch—anastomoses w/ asc. branch of right colic a. Left branch—anastomoses w/ asc. branch of left colic a. (left colic comes off IMA) Superior mesenteric vein (SMV)—usually along right side of SMA o Tributaries—correspond in name/position to branches of SMA o Drainage—joins splenic vein to form hepatic portal vein post. to pancreas Mesenteric lymph nodes—up to 200 in mesentery; can ID them along branches of SMA/SMV o Superior mesenteric lymph nodes—drain the mesenteric lymph nodes near origin of SMA Small Intestine Jejunum—proximal two-fifths of SI; circular folds (internal feature) are larger & closer together than ileum Ileum—distal three-fifths of SI Duodenojenual junction Suspensory ligament of the duodenum—fibromuscular ligament arising from right crus of diaphragm o Anchors SI @ duodenojejunal junction; passes post. to pancreas Cecum o Ileocecal orifice o Sup./inf. lips of ileocecal valve o Opening of appendix Ileocecal junction Root of mesentery—crosses post. abd. wall from duodenojejunal junction to ileocecal junction; 15 cm long o Intestinal attachment of mesentery—6m long Inferior Mesenteric Artery (IMA)—from ant. surface of abd. aorta @ LV3 (post. to 3rd part of duodenum) Supplies left 3rd of trans. colon, desc. colon, sigmoid colon, & most of rectum Branches are all retroperitoneal except for branches that pass through sigmoid mesocolon IMA & vein pass ant. to ureter Branches of IMA: o Left colic artery—supplies desc. colon & left 3rd of trans. colon Anastomoses w/ middle colic branch of SMA & asc. branch of first sigmoid artery o Sigmoid arteries—3-4 arteries to sigmoid colon; pass through sigmoid mesocolon; form arcades o Sup. rectal artery—to proximal rectum Right/left branches—descend into pelvis on either side of rectum Inferior mesenteric vein (IMV)—tributaries correspond to branches of IMA; drains to portal vein o Ascends on left side of IMA, passes post. to pancreas, usually joins splenic v. (sometimes SMV) Inferior mesenteric nodes—around origin of IMA; drain lymph vessels that drain desc. & sigmoid colon Large Intestine Cecum—in right lower quadrant o Vermiform appendix—attached to end of cecum, suspended from mesoappendix Ascending colon—extends from cecum to right colic flexure Transverse colon—extends from right colic flexure to left colic flexure; mucosa is relatively smooth o Left colic flexure is more superior than right colic flexure o Semilunar folds (plicae semilunares)—found internally btwn. adj. haustra Descending colon—descends from left colic flexure to left lower quadrant; secondary retroperitoneal organ Sigmoid colon—in left lower quadrant; suspended from sigmoid mesocolon; cont. w/ rectum @ 3rd sacrum Rectum—contained entirely w/in pelvic cavity Anal canal Three external features distinguish LI from SI: o Teniae coli—3 narrow bands of longitudinal muscle o Haustra—outpouchings on wall of colon o Omental appendices (epiploic appendages)—small accumulation of fat, covered by visc. peritoneum Duodenum—drainage point for ducts of liver & pancreas Superior (1st) part—at LV1; lies in transverse plane; att. to hepatoduodenal ligament; mostly peritoneal o Ampulla/Duodenal cap/duodenal bulb—expanded proximal part Descending (2nd) part— at LV2; right of midline, ant. to hilum of r. kidney/renal vessels & IVC; retroperit. o Major (greater) duodenal papilla—elevation of mucosa on post.-medial wall It is the shared opening of the main pancreatic duct & bile duct o Minor (lesser) duodenal papilla—site of drainage of acc. pancreatic duct; sup. to major papilla o Circular folds (plicae circulares) Horizontal (3rd) part—at LV3; ant. to IVC & abd. aorta; retroperitoneal o Crossed anteriorly by sup. mesenteric vessels & posteriorly by inf. mesenteric vessels Ascending (4th) part—ascends to LV2; mostly retroperitoneal; turns anteriorly @ duodenojejunal junction Pancreas—secondarily retroperitoneal; lies across midline against LV1-3 Head—w/in curve of duodenum; IVC lies posteriorly o Uncinate process—small projection from inf. margin of head; passes post. to sup. mesenteric vessels Neck—short; lies ant. to sup. mesenteric vessels; connects head to body Body—extends from right-to-left & slightly superiorly; crosses post. abd. wall; abd. aorta lies posteriorly Tail—narrow left end; tip of tail in splenorenal ligament (thus tip is peritoneal); contacts hilum of spleen Main pancreatic duct—joined by bile duct near left side of 2nd part of duodenum Accessory pancreatic duct—joins sup. side of main pancreatic duct Ant./Post. superior pancreaticoduodenal (PD) arteries—branches of gastroduodenal artery Inferior PD artery—usually most proximal branch of SMA; enters inf. portion of head Splenic artery—runs along sup. border of pancreas; gives off up to 10 small branches to body & tail: o Dorsal pancreatic artery—enters neck o Greater pancreatic (pancreatica magna) artery—enters btwn. neck & tail Left gastro-omental artery—to greater omentum; anastomoses w/ right gastro-omental (from GD artery) Veins of pancreas—correspond to arteries; drain into SMV/splenic v. & ultimately portal vein Hepatic Portal Vein—carries venous blood to liver from abd. portion of GI tract, spleen, & pancreas Formed by union of SMV & splenic vein, post. to neck of pancreas Ascends in hepatoduodenal ligament to porta hepatis of liver Splenic vein—courses post. to pancreas; inf. to splenic artery IMV—usually joins splenic v., but may join either SMV or junction of SMV/splenic Portal-systemic anastomoses: o Gastroesophageal—left gastric v./esophageal v./azygos v. o Anorectal—sup. rectal v./middle & inf. rectal vv. o Paraumbilical—paraumbilical vv./superficial epigastric vv. o Retroperitoneal—colic vv./retroperitoneal vv. Lab 8: Posterior Abdominal Viscera, Posterior Abdominal Wall, & Diaphragm Posterior Abdominal Viscera—located in retroperitoneal space Retroperitoneal space—btwn. post. parietal peritoneum bounding abdominal cavity/muscles & bones of post. abdominal wall; contains kidneys, ureters, suprarenal glands, aorta, IVC, & abdominal portions of sympathetic trunks Testicular artery & vein—@ deep inguinal ring; cross ant. to ureter o Left testicular v. drains into left renal v.; right testicular v. drains into IVC Right/left testicular arteries—branch from aorta @ LV2 (inf. to origin of renal aa.) Ovarian vessels—cross ant. to ureter; more inferiorly, cross ant. to external iliac vessels Kidneys—lateral to vertebral column from T12-L3 o Renal fascia o Perirenal fat o Superior pole—separated from suprarenal gland by layer of renal fascia o Left renal vein—ant. to both renal aa. & aorta; drains to IVC; tributaries: Left testicular/ovarian vv. (aka gonadal vv.) Left suprarenal v. o Left renal artery—post. to left renal v.; divides into segmental arteries @ hilum; branches: Inferior suprarenal artery—to left suprarenal gland Ureteric branch—to left ureter o Renal pelvis o Ureter—passes post. to gonadal vessels; crosses ant. surface of psoas major; post. to branches of IMA o Right renal veins—has no tributaries o Right renal artery—longer than left renal a.; branches: Inferior suprarenal artery—to right suprarenal gland Ureteric branch o Relationships of kidneys: Suprarenal gland is superior Right kidney contacts hepatic flexure, visceral surface of liver, & 2nd part of duodenum Left kidney contacts tail of pancreas, splenic flexure, stomach, & spleen Hilum of kidney faces anteromedially; lateral border of kidney faces posterolaterally o Internal features of kidneys: Renal capsule—fibrous capsule, firmly att. to surface of kidney Renal cortex—outer zone of kidney Renal medulla—inner zone fo kidney; consists of renal pyramids & renal columns Renal sinus—space w/in kidney occupied by renal pelvis, calices, vessels, nerves, & fat Renal papilla—apex of renal pyramid, projects into minor calyx Minor calyx—cup-like chamber, beginning of extrarenal duct system Major calyx—combo of minor calices, 2-3 per kidney combine to form renal pelvis Renal pelvis—funnel-like end of ureter, begins w/in renal sinus & emerges from renal hilum Ureter—muscular duct that carries urine from kidney to bladder Suprarenal glands—endocrine fx (thus extensive blood supply); sup. to kidneys w/in own renal fascia shell o Right SRG—triangular; part is post. to IVC o Left SRG—semilunar in shape o Superior suprarenal arteries—from inferior phrenic artery (from abdominal aorta) o Middle suprarenal artery—arises from aorta near celiac trunk o Inferior suprarenal artery—arises from renal artery o Left suprarenal vein drains to left renal v.; right suprarenal vein drains to IVC Abdominal aorta—begins @ TV12 (as cont. of thoracic aorta); bifurcates into common iliac aa. @ LV4 o Common iliac arteries—supply blood to pelvis & lower limbs o Unpaired visceral arteries—to GI tract: Celiac trunk, SMA, IMA o Paired visceral arteries—to 3 paired abdominal organs: middle suprarenal aa., renal aa., gonadal aa. o Paired somatic arteries—to abdominal walls: lumbar aa., inferior phrenic aa. Lumbar arteries: supply post. abd. wal; pass deep to psoas major; right a. passes post. to IVC Inf. phrenic arteries: arise near aortic hiatus; give rise to sup. suprarenal aa. IVC—begins @ LV5 by joining of common iliac vv.; ends @ TV8 by passing thru caval hiatus & emptying into RA o Has no unpaired tribuatires from GI tract b/c portal system drains GI tract o Receives drainage from paired abdominal organs—renal v., suprarenal v., gonadal v. o Receives paired vv. from abdominal wall—lumbar vv., inf. phrenic vv. Posterior Abdominal Wall—composed of vertebral column, mm. that move column, mm. that move lower limbs, & diaphragm Psoas major muscle—strong flexor of thigh & vertebral column o Origin: bodies, IV discs, & transverse processes of LVs o Insertion: lesser trochanter of femur Psoas minor muscle—long flat tendon passes down ant. surface of psoas major; inserts on iliopubic eminence & arcuate line of ilium Iliacus muscle—flexes the thigh; joins w/ psoas major to form functional unit called iliopsoas muscle o Origin: iliac fossa o Insertion: lesser trochanter of femur Quadratus lumborum muscle—flexes vertebral column laterally & anchros inf. end of rib cage during resp. o Origin: 12th rib & lumbar transverse processes o Insertion: iliolumbar ligament & iliac crest Transversus abdominis muscle—forms lateral part of post. abdominal wall; lies post. to quad. lumborum Relationship of kidneys to post. abdominal wall: o Post. surface of each kidney related to diaphragm, psoas major, quad. lumborum, & transverse abd. o Sup. pole of right kidney is near 12th rib; sup. pole of left kidney is near 11th rib Subcostal nerve—about 1 cm inf. to rib 12 Lumbar plexus—formed by ant. rami of nerves L1-L4 w/in psoas major o Genitofemoral nerve—on ant. surface of psoas major; divides sup. to inguinal ligament: Genital branch—passes thru deep inguinal ring & inguinal canal; motor to cremaster muscle Femoral branch—passes under inguinal ligament on ant. surface of external iliac a.; supplies skin inf. & med. to inguinal ligament o Iliohypogastric & ilioinguinal nerves—desc. steeply across ant. surface of quad. laborum; ilioinguinal nerve runs to superficial inguinal ring o Lateral cutaneous nerve of thigh—passes deep to inguinal ligament near ASIS o Femoral nerve—in groove btwn. psoas major & iliacus; inn. iliacus; passes deep to inguinal ligament Motor/sensory branches to ant. thigh o Obturator nerve—motor/sensory to medial thigh o Lumbosacral trunk—deep to obturator nerve; formed by ½ of L4 ant. ramus & all of L5 ant. ramus Joins sacral plexus in pelvis Sympathetic trunk—abdominal part lies on lumbar vertebral bodies btwn. crus of diaphragm & psoas major Lumbar splanchnic nerves—pass. ant. from lumbar SG to aortic ANS plexus Rami communicantes—pass post. from SG to lumbar ant. rami; deep to psoas major on lat. side of LV’s o Gray rami here are longest in body b/c sympathetic trunk crosses anterolateral surface of LV bodies Diaphragm—roof of abdominal cavity & floor of thoracic cavity; principal muscle of respiration Central tendon—aponeurotic center; distal att. of all mucular parts Sternal part—two small bundles of muscle fibers that att. to post. surface of xiphoid process Costal part—muscle fibers that att. to inf. 6 ribs & their costal cartilages Lumbar part—formed by left/right crura & muscle fibers arising from medial & lateral arcuate ligaments Right crus—proximal att. are LV1 to LV3 o Esophageal hiatus—opening in the right crus @ TV10 Left crus—proximal att. ar LV1 to LV2 Arcuate ligaments—thickenings of fascia, serve as proximal att. for some muscle fibers of diaphragm o Lateral arcuate ligaments—bridge ant. surface of quad. lumborum o Medial arcuate ligaments—bridge the ant. surface of psoas major o Median arcuate ligament—bridges ant. surface of aorta @ aortic hiatus Vena caval foramen—passes thru central tendon (TV8) Esophageal hiatus—passes thru right crus (TV10) Aortic hiatus—passes behind diaphragm (TV12) Right/left phrenic nerves—each provides motor inn. to one hemidiaphragm; sensory to diaphragm’s parietal pleura & parietal peritoneum o Note: diaphragm also receives sensory inn. from intercostal nn. T5-T11 & subcostal n. (T12) Greater splanchnic nerve—penetrates crus to enter abdominal cavity; mainly to celiac ganglion Celiac ganglia—lateral to celiac trunk near origin from aorta