* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Common fungi - Fungal Infection Trust
Survey
Document related concepts
Germ theory of disease wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Neonatal infection wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Infection control wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Transcript
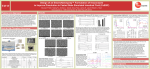
Fungal Research Trust supports launch of new anti-fungal drug Patrons Lord Turnberg of Cheadle Mrs Nicola Horlick Prof Stefan Buczacki The Fungal Research trust are pleased to announce the long awaited launch of Posaconazole (NoxafilR, Schering-Plough) in the UK. The world's first studies showing the effect of this drug against Aspergillus infections were as demonstrated in 1997 by studies funded by the Fungal Research Trust (FRT). In particular, Aspergillus resistant to itraconazole was shown to respond to Posaconazole. Approval for use in patients was granted for "Invasive aspergillosis in patients refractory to/or intolerant of amphotericin B or itraconazole." Trustees Dr Geoff Scott (Chairman) Mr John Morgan (Secretary) Mr Richard Gourlay Mr Phillip Oxnam Research Advisory Board Prof Jacques Bille (Lausanne) Prof David Denning (Manchester) Prof Roderick Hay (Belfast) Dr Kenneth Haynes (London) Prof Jack Sobel (Detroit) Aspergillus species are a cosmopolitan very common air-borne fungus, carried in the air all over the world as spores. Aspergillosis (the diseases caused by Aspergillus) mainly affects the lungs and sinuses, but can spread to other organs such as the brain. As well as leukaemia and bone marrow transplant patients, 'invasive aspergillosis' is increasingly affecting other immuno-suppressed hospital patient groups and is very difficult to treat. Up to half of sufferers die of the condition, and as many as 1 in 25 patients who die in modern European teaching hospitals are now suffering from it. Other immuno-compromised patients such as those after transplantation, with AIDS or leukaemia or on steroid treatment are increasingly being affected with life-threatening Aspergillus pneumonia and sinusitis. Death from fungal infection is a very disappointing outcome after successful treatment of patients for underlying diseases. Estimates of the numbers of patients in the UK in 2002 are shown in this table. Patient The Fungal Research Trust is responsible for The Aspergillus website: www.aspergillus.man.ac.uk Number (2002) Bone marrow Tx Solid organ Tx Leukaemia Solid tumour (neutropenic) Advanced cancer ICU AIDS Total 793 2,697 15,802 27,824 127,766 ~200,000 <400 % invasive aspergillosis 8.10% 2.2-2.8% 6.50% 1% 1.86% 3.62% 0.60% The Fungal Research Trust Charity No: 1003361 P O Box 482, Macclesfield, Cheshire, SK10 9AR, UK Telephone No: 01625 500228 Website: www.fungalresearchtrust.org Email: [email protected] Range 2.8-15.1% 0.8-16.0(lung)% 2.0-9.6% 1 study only 1.3-2.2% 2.7-3.7% 0.02-4.0% Expected cases invasive aspergillosis 64 62-78 1,027* 278 2,376* 7,240* 2 10,992 *Some double counting To put these numbers in context, there are between 1000 and 2000 cases of meningitis per year in the UK. Posaconazole has advantages over previous drugs in being more active against Aspergillus and other rarer moulds, has very few side-effects and many fewer drug interference properties compared with other similar drugs. The FRT's Scientific Advisor, Professor David Denning said, "Having seen such powerful activity in 1997, it is gratifying that posaconazole has now become available to treat patients. It will have a particular role in preventing infection in leukaemia and after bone marrow transplantation. It is the broadest spectrum antifungal now available." Aspergillus can worsen asthma and cause allergic sinusitis in patients with allergic tendencies, and can also get into lung cavities created by tuberculosis (which affects a third of the world's population) causing general ill-health and bleeding in the lung. - E N D S - For further information please contact : June Beedham: 0771 432 6527 Prof. David Denning: 078024 82193 12 May 2006 NOTE TO EDITORS: The Fungal Research Trust (www.fungalresearchtrust.org) is a registered charity which funds research into and education about fungal infection. It was set up in 1991 and since then has distributed in excess of £1.6m in research grants resulting in more than 80 research publications in clinical and scientific aspects of fungal infection. It also supports the Aspergillus Website which achieves around 160,000 page requests a month. As well as being a key resource for clinicians, the website also devotes a section to patients and relatives to help them understand more about the disease. It can be found at www.aspergillus.man.ac.uk. What is fungal disease? There are 4 broad groups of fungal infections in man (fungi are the main cause of plant disease as well). Fungal infections can be grouped as follows: Thrush (ie vaginal thrush, oral thrush (AIDS and cancer patients, antibiotic treatment) and severe nappy rash) Skin infections ie athlete’s foot, ringworm, dandruff, cradle cap, nappy rash and nail infections Invasive and life-threatening infection ie candidiasis (intensive care, prematurity, leukaemia, diabetes, dialysis), invasive aspergillosis (leukaemia, transplantation and steroid treatment) and cryptococcal meningitis (AIDS) Allergic fungal disease ie allergic fungal sinusitis (normal people with chronic sinusitis) and allergic bronchopulmonary aspergillosis (asthma and cystic fibrosis) and severe asthma with fungal sensitisation Common fungi Common fungi causing disease are: Candida albicans (thrush and invasive candidiasis) Aspergillus fumigatus (allergic fungal disease and invasive aspergillosis) Trichophyton interdigitale (athlete’s foot and nail infections) About 30 different species of fungi cause the vast majority of human fungal infection. In all about 600 species out of an estimated 1 million species worldwide cause human infection; others are implicated in allergic disease. Fungal Research Trust papers Efficacy of SCH-56592 (posaconazole) in a temporarily neutropenic murine model of invasive aspergillosis with an itraconazole-susceptible and an itraconazole-resistant isolate of Aspergillus fumigatus. Oakley KL, Morrissey G, Denning DW. Department of Medicine, Hope Hospital, Salford, and University of Manchester, United Kingdom. Antimicrob Agents Chemother. 1997 Jul;41(7):1504-7. SCH-56592 (SCH) is a novel triazole antifungal agent with excellent in vitro activity against Aspergillus. We compared three doses (5, 10, and 25 mg/kg of body weight) of SCH with itraconazole (ITZ; 25 mg/kg) and amphotericin B (AB; 5 mg/kg) in a temporarily neutropenic murine model of disseminated aspergillosis (lungs and kidneys) against one ITZsusceptible (AF71) and one ITZ-resistant (AF90) isolate of Aspergillus fumigatus. Treatment started 24 h after infection and lasted for 10 days. Dosing regimens for SCH were once daily for 10 days, those for ITZ were three times daily for 2 days and then twice daily for 3 to 10 days, and those for AB were once daily on days 1, 2, 4, and 7. Both isolates killed 90% of control mice. Kidneys and lungs from survivors were cultured on day 11. Against AF71, all three doses of SCH and ITZ yielded a 90 to 100% survival rate and AB yielded 40% survival (P < or = 0.01 to 0.0001 for all treatment groups compared with the controls). All three doses of SCH were superior to AB in cultures of lung and kidney tissue samples (P < or = 0.01 to 0.0002) and SCH at 25 mg/kg was superior to ITZ in cultures of kidneys (P = 0.01). Against AF90, the highest dose of SCH (25 mg/kg) resulted in a 100% survival rate, compared with 60 and 20% survival rates for the groups treated with SCH at 10 and 5 mg/kg, respectively. Treatment with ITZ yielded no survivors. AB therapy achieved a 50% survival rate. SCH at 25 mg/kg (P < 0.001), SCH at 10 mg/kg (P < or = 0.005), and AB (P < 0.05) were superior to ITZ in cultures of lungs and kidneys. There was a correlation between the MICs of SCH and quantitative organ culture results and between the minimum fungicidal concentration of AB with quantitative organ culture results. SCH appears to be a highly effective anti-Aspergillus compound in this model. There appears to be a degree of cross-resistance between itraconazole and SCH. PMID: 9210674 In vitro activity of SCH-56592 (Posaconzole) and comparison with activities of amphotericin B and itraconazole against Aspergillus spp. Oakley KL, Moore CB, Denning DW. Department of Medicine, Hope Hospital, Manchester, United Kingdom. Antimicrob Agents Chemother. 1997 May;41(5):1124-6. In this study, we investigated the in vitro activity of SCH-56592 (SCH), a new triazole antifungal agent. We compared the activity of SCH with those of itraconazole (ITZ) and amphotericin B (AB) against 60 clinical isolates of Aspergillus spp. by using a microtiter format. Incubation was done at 37 degrees C for 48 h, and MIC endpoints (no growth) were read visually. The medium used for all of the drugs was RPMI 1640 buffered with morpholinepropanesulfonic acid (MOPS) and supplemented with 2% glucose. MICs and minimum fungicidal concentrations (MFCs; killing of > or = 99.99%) were measured for all isolates. The geometric mean (GM) MICs and ranges (in micrograms per milliliter) were as follows: SCH, 0.09 and < or = 0.01 to 1; ITZ, 0.25 and 0.06 to 32; AB, 1.46 and 0.25 to 32. Aspergillus terreus (n = 7) was markedly more susceptible to SCH (GM, 0.05 microg/ml) and ITZ (GM, 0.07 microg/ml) than to AB (GM, 8.8 microg/ml). For all isolates, the GM MFCs and ranges (in micrograms per milliliter) were as follows: SCH, 3.64 and 0.125 to 16; ITZ, 15.09 and 0.125 to 32; AB, 10.3 and 1 to 32. In the drug concentration range tested, 71, 32, and 64% of the isolates against which SCH, ITZ, and AB, respectively, were tested were killed. A reproducibility study was performed with 20% of the isolates; for 11 of the 12 isolates retested, the MIC was the same or within 1 well of the original MIC of each drug. Therefore, in vitro mould testing of SCH is feasible and reproducible. SCH was found to be very active against all species of Aspergillus and at lower concentrations than either ITZ or AB. PMID: 9145880 -ends-