* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Drug Overdose
Drug discovery wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Electronic prescribing wikipedia , lookup
Drug interaction wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
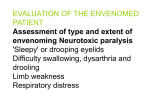
Pharmacokinetics wikipedia , lookup
Drug Overdose DRUG OVERDOSE Management Principles and Decontamination History Speak to: patient relatives ambulance officers Ask what drug was ingested when how much Examination LOC GCS uniformly used developed for prognosticating head injuries verbal and pain response most useful in DSPs • AVPU Vital signs Temp/PR/BP/RR/SpO2 Examination Mini-Neuro Pupil size and reaction Reflexes Gross assessment of muscle tone Chest/CVS as appropriate but low yield BS may be in anticholinergic toxidrome Investigation BSL mandatory if LOC ECG always done findings very specific QRS complex indicative of Na+ channel blockade if prolonged Investigation Normal QRS is < 100 ms QT interval <420 ms male <440 children <450 female may be prolonged in certain poisonings neuroleptics esp. thioridazine QT or QTc ? Standardises QT to a rate of 60 bpm only useful if heart rate <70 or >50 Investigation Concentrations are useful if suggestion of poisoning with salicylates paracetamol lithium valproate theophylline No use as a screening tool Investigation ABG Useful in assessing ventilatory status Useful if ingestion can cause metabolic upset: (VBG) salicylate metformin OR if patient needs serum or urinary alkalinisation Investigation Miscellaneous: CXR if aspiration suspected CT brain if story not c/w clinical findings CK if unconscious for some time K+ in digoxin poisoning Close attention to ABC and supportive care is all that is required to manage MOST drug overdoses GCS/vital signs/mini neuro and ECG are only tests/investigations likely to alter management with a few notable exceptions Treatment May be specific antidote NAC in paracetamol poisoning May be general/empiric decontamination coma cocktail generous IV fluid replacement Treatment Coma cocktail Dextrose/Thiamine/Naloxone/Flumazenil Problems hypoglycaemia can be assessed with BM stix Naloxone can precipitate acute withdrawal Flumazenil may complicate further seizure management Decontamination When should patient be decontaminated? risk of morbidity and/or mortality associated with ingestion What type of decontamination should be used? Depends on clinical circumstances and other treatment options Decontamination Syrup of Ipecac Gastric lavage Activated charcoal • multi dose • with cathartic Whole bowel irrigation Where is the Evidence ? Based on Animal studies Volunteer studies clinical studies Difficulty due to serious ingestions excluded conflicting results Where is the Evidence Position statements released in 1997 by AACT and EAPCCT “Overall the mortality from acute poisoning is less than 1 % and the challenge for clinicians is to identify promptly those who are at most risk of developing serious complications and who might potentially benefit, therefore, from gastrointestinal decontamination.” Syrup of Ipecac Plant extract previously abused by bullimics needs to be given EARLY induces vomiting by gastric and central mechanism Contraindicated in unprotected airway corrosive very little evidence for or against possible role in the home for children Gastric lavage No studies demonstate efficacy even < 60 min.s Studies exclude serious poisonings Contraindicated: dodgy airway reflexes corrosives hydrocarbon Gastric lavage May increase risk of aspiration May lead to pharyngeal injury alleged to increase absorption in some cases Has lead to significant return of ingestants up to 12 hours post ingestion(salicylates) Indication Serious life threatening poisoning with well protected airway (level IV evidence) Activated charcoal Will adsorb many toxins in GI tract BUT: • Alcohols • Li+, Fe 2+ (probably all alkali metals) Ratio should be 10:1 AC:toxin Evidence from volunteer studies that absorption will be if < 60 min.s Little to suggest benefits outcome clinically or absorption post 60 min.s DO NOT GIVE ROUTINELY Activated charcoal Beware the unprotected airway or aspiration risk dose is 50g adult, 1g/kg in a child Cathartics Alleged to increase bowel transit time of toxin Evidence only from animal and volunteer studies Unlikely to benefit Multi dose activated charcoal Works by • GI dialysis • drugs with significant enterohepatic circulation examples: • • • • theophylline anticonvulsants salicylates digoxin Multi dose activated charcoal Good, though indirect evidence of effect in digoxin poisoning 50g q 6 hrly OR by NG infusion if intubated up to 1g/kg suggested for serious theophylline poisonings Justifies “late” instigation of charcoal Whole bowel irrigation Used for SR/EC preparations when charcoal is ineffective No controlled clinical studies to back up use physically speeds up transit through GI tract single dose charcoal given prior to starting Whole bowel irrigation PEG ELS (“go-lytely”) is used does not cause significant water/electrolyte disturbance frequently causes vomiting, requires NGT airway must be protected ileus is CI but has been reversed with neostigmine dose is 15-20 mls/kg/hr endpoint is clear rectal effluent, median time to achieve this is 6 hours Duty of Care Ingestion of an overdose renders a patient incompetent If requires hospitalisation for physical effects of drug overdose • keep under duty of care If no medical issues and attempts to leave Schedule II Take home messages History, focused exam and a few tests, supportive care +/- period of observation is appropriate management for most DSPs Ipecac is never used, gastric lavage occasionally Charcoal is only given if likely to benefit Patients receiving decontamination must have airway protection