* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Glaucoma Associated with Keratoprosthesis
Survey
Document related concepts
Blast-related ocular trauma wikipedia , lookup
Visual impairment wikipedia , lookup
Idiopathic intracranial hypertension wikipedia , lookup
Mitochondrial optic neuropathies wikipedia , lookup
Visual impairment due to intracranial pressure wikipedia , lookup
Transcript
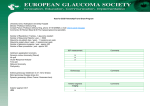
Glaucoma Peter A. Netland, Associated with Keratoprosthesis MD, PhD, Hisao Teruda, MD, Ches H. Dohlman, MD, PhD Objective: This study aimed to review the authors clinical experience with glaucoma associated with keratoprosthesis in patients with severe cornea1 disease. Design: The study design was a retrospective review of case series. Participants: The authors studied 55 eyes in 52 patients with keratoprostheses with follow-up of 21 ? 16 months (range, 3-77 months). Intervention: Glaucoma drainage devices were implanted in 36 eyes (35 Ahmed valves, 1 Krupin valve) with 21 ? 15 months’ follow-up (range, 3-64 months). Main Outcome Measures: Clinical outcome assessment included vision, intraocular pressure (IOP), visual fields, optic disc appearance, and identification of complications. Results: Glaucoma was found in the majority (64%) of eyes treated with keratoprostheses, identified in 20 eyes (36%) before surgery and an additional 15 eyes (28%) after surgery. Of the 36 eyes treated with glaucoma drainage devices, IOP was controlled in 29 eyes (81%), with 9 eyes (25%) requiring additional medications. Continued progression of glaucoma occurred in 5 (14%) of 36 eyes with keratoprostheses and glaucoma drainage implants (4 of these eyes had advanced glaucomatous optic nerve damage before surgery). There were nine nonvision-threatening complications due to drainage implants. Compared with the preoperative visual acuity, vision was markedly improved in 63%, unchanged in 17%, and worse in 20% of eyes after keratoprosthesis surgery. Conclusion: Elevation of IOP is common in patients with keratoprosthesis, and prevention or treatment with glaucoma drainage implants is effective. Ophthalmology 7998; 705757-757 Despite advances in transplantation techniques using human cornea, the prognosis for standard keratoplasty remains poor in patients with severe past or ongoing chronic inflammation of the ocular surface. This poor prognosis group includes patients with Stevens-Johnson syndrome, ocular cicatricial pemphigoid, end-stage dry eye, and severe chemical burns.‘,* In addition, some patients with repeated graft failures due to immune reaction have a poor prognosis for subsequent keratoplasty. Keratoprosthesis surgery is an alternative for visual rehabilitation of these patients. However, earlier attempts using keratoprosthesis in humans were plagued by precipitous and severe complications, usually related to necrosis of the tissue surrounding the prosthesis that could lead to leakage of aqueous, infection, or extrusion. Recent improvements of techniques and modification of the postoperative regimen have improved the prognosis after keratoprosthesis surgery.” Necrosis of the tissue around the device and extrusion are now less common because of temporary postoperative coverage of the de- Originally received: June 2, 1997. Revision accepted: September 18, 1997. From the Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, Massachusetts. Presented in part as a poster at the American Academy of Ophthalmology Annual Meeting, Chicago. Illinois, October, 1996. Supported by Mr. Sa’ad A. A. Al-Rashed, Kuwait. The authors have no propriety interest in the devices used In this study. Reprint requests to Peter A. Netland, MD, PhD, The University of Tennessee, Memphis, Department nue, Memphis, TN 38163. of Ophthalmology, 956 Court Ave- vice with conjunctiva or skin and topical administration of collagenase inhibitors.4 Postoperative uveitis has been minimized by use of moderate-dose steroid regimens. Retroprosthesis membranes that form despite steroid therapy generally are mild and may be opened with the neodymium:yttrium-aluminum-garnet laser.5 With reductions of these complications, other long-term visionthreatening problems have become more important, especially glaucoma.” The purpose of this study was to review our own clinical experience with glaucoma in patients with keratoprosthesesand to describe the useof glaucoma drainage implants in this setting. Methods Patients treated with keratoprosthesis and glaucoma drainage implant gave verbal consentand signedan informed consent form approvedby the Institutional Review Board. Eyes with keratoprostheses were from a consecutive series of cases per- formed from March 1990to June 1996.No eyes with keratoprosthesis implanted during this period were excluded from the analysis. Glaucoma drainage implants were performed in eyes with keratoprosthesis from February 1991 to June 1996. The surgical procedures have been described in detail elsewhere.’ The Dohlman-Doane polymethylmethacrylate keratoprosthesis type I or II was used in all patients.* The type I device was used except in extremely dry eyes, in which the longer nub in the type II design was used for a through-the-lid approach. If present, the lens was removed using extracapsular technique, and total iridectomy often was performed. In patients with preexisting glaucoma or those with chronic inflammation and a high risk of subsequently developing glaucoma, a glaucoma drainage implant was included at the time of keratoprosthesis Ophthalmology Volume 10.5, Number 4, April 1998 Table 1. Patient Characteristics Without Glaucoma Drainage Implant With Glaucoma Drainage Implant 19 18 36 No. of eyes No. of patients Race [N (%)I White Black Aslan Indian Arabic 24 (66) 5 (14) 1 (3) Sex [N (%)I Mean ? SD Range Follow-up (mos)* Mean ? SD Range Keratoprosthesls design [N (%)I? Type 1 Type II Lens status [N (%)I Pseudophakic Aphakic Adluncnve surgical procedures [N (%)I Vitrectomy lridectomy Lensectomy Diagnosis [N (%)I$ SD = standard 2 (4) 4 (7) (11) 21 (58) 15 (42) 28 (51) 27 (49) 64 + 22 24-93 63 + 18 26-91 64 i 19 24-93 t_ 17 t 15 21 4-77 ? 16 21 3-64 3-77 16 (84) 3 (16) 18 18 (50) (50) 34 (62) 21 (38) 1 (5) 18 (95) 4 (11) 32 (89) 5 (9) 50 (91) 18 (50) 21 (58) 27 (75) 24 (44) 27 (49) 37 (67) 15 (42) 18 7 13 3 14 6 (32) 6 (32) 10 (53) Pemphigoid 6 (11) 1 (2) 7 (37) 12 (63) 21 3 1 5 3 7 Stevens-Johnson Chemical burn Herpetic keratitis Graft failure 42 (76) 2 (6) 4 Age (yrs) 55 52 34 18 (95) 1 (5) - Male Female Total (16) (5) 6 (17) (26) 8 (22) 0 (0) (16) (37) 7 (19) (33) (13) (24) (5) (25) deviation. * Follow-up period was until the most recent appomtment, death (N = l), or keratoprosthesis removal (N = 6), mcludmg retmal detachment (N = 3) or enucleation (N = 2). Patients wieh and without glaucoma dratnage Implants were not slgmficantly different m their age or follow-up period (P = 0.88 and 0.99, respectively, unpaired t test). t Patients with and without glaucoma drainage implants were slgnlficantly dlfferent (P = 0.013, chi-square). $ Patients with and without glaucoma drainage Implants were significantly different (P = 0.027, chl-square). surgery. In other patients who subsequently developed glaucoma, the device was implanted at a later time. The drainage implant was preferentially positioned superotemporally or superonasally. In one patient, a second Ahmed drainage implant was positioned superotemporally when the patient developed progressive visual field changes after the keratoprosthesis procedure with the first drainage implant that had been positioned in the superonasal quadrant. The implant tube and, in many patients, the device plate were covered with eye bank sclera. The keratoprosthesis then was covered with conjunctiva (type I) or lid skin (type II). After surgery, a moderate-dose steroid regimen was used, including topical, systemic, and, in particular, peribulbar routes of administration.’ Eyes were imaged with B-mode ultrasound during the immediate postoperative period. The conjunctiva or skin was opened at approximately 2 months after surgery. Systemic oral antibiotics were administered during the immediate postoperative period, and topical prophylactic antibiotics were administered indefinitely after surgery. Anticollagenase medications, such as 1% medroxyprogesterone and 1% tetracycline, were used for months or years after surgery. 752 Visual Outcome Improved 83% Glaucoma Present 84% Figure 1. Summarv of visual outcome and glaucoma m eyes treated with keratoprosthesls. The visual ouecome was improved from hght perceptlon, hand movements, or finger counting to between 20/200 and 20/20 in the majority (63%) of eyes at the most recent follow-up exammatlon after keratoprosthesls surgery. Glaucoma, characterized by consistently elevated intraocular pressure or progressive glaucomatous changes of the vtsual field and optic nerve head, was found m the malorlty (64%) of eyes. (Values shown are the proportion of all eyes with keratoprosthests, n = 55.) Netland et al * Glaucoma Associated with Keratoprosthesis A appearance of the Dohlman-Deane keraroprostheses. A, type I keratoprosthesls in the left eye of a patlent wth a history of repeated graft fadure and glaucoma. The scleral patch graft covermg the aqueous shunt tube 1s vwble through the conlunctwa In the superonasal area B, type II keratoprosthesls (through the hd) In a burn patlent. The aqueous shunt tube LSunder the hd skm and LSnot vwble. Figure 2. Examples of the postoperatwe The intraocular pressure (IOP) was assessed before surgery by tonopen, pneumotonometer, or tactile estimation, depending on the severity of the cornea1 disease. After surgery, IOP was assessed by tactile estimation by two independent observers (PAN and CHD). The IOP was characterized as low, normal, or elcvatcd (IOP > 21 mmHg was considcrcd elevated when measurement by tonopen or pneumotonometer was possible). Agreement between observers was found for all cases characterized as elevated. Visual fields were measured by automated perimetry or Goldmann perimetry (the visual field extends to up to 70” and 40” in eyes with keratoprosthesis type I and type II, respectively). The optic nerve was assessed by stereophotography or by clinical biomicroscopic examination, which can be performed through both the type I and type II keratoprostheses. Glaucoma was defined as elevated IOP on at least two visits or progressive glaucomatous changes of the visual field and optic nerve head. In addition, four eyes in four patients were found to have end-stage glaucomatous optic disc cupping and visual field loss after the tissue covering the keratoprosthesis was opened and were included in the glaucoma group. In some cases, the anterior segment was examined using the ultrasound biomicroscope (UBM, Humphrey Systems, San Leandro, CA). However, many cases could not be assessed by UBM because of the thickness of the overlying tissue. The vision was light perception (21 eyes), hand movements (24 eyes), or finger counting (10 eyes) in all patients before surgery. The postoperative vision was considered improved if the Snellen visual acuity was in the range between 201200 to 20120. The vision was considered the same if the vision was unchanged or did not improve to between 201200 and 2Of20. The vision was considered worse if there was any change in the following order: finger counting, to hand movements, to light perception, to no light perception. Patients with keratoprostheses with and without glaucoma drainage implants were compared using the unpaired t test and the chi-square test. Probability values less than 0.05 were considered statistically significant. Results The characteristics of the patients are listed in Table 1. A total of 55 keratoprostheses were implanted in 52 patients. The mean ? standard deviation age was 64 t 19 years, with a range of 24 to 93 years. The follow-up period was 21 2 16 months, with a range of 3 to 77 months. Glaucoma drainage devices were implanted in 36 eyes (65% of total) in 34 patients (65% of total). The type of keratoprosthesis was significantly different in the patients with and Table 2. Patients with Keratoprosthesls Treated with Glaucoma Draillage Implant No of eyes* No of patients Type of Implant [N (%)] Ahmed valve Krupm valve Locxlon of Implant [N (%)I Superotemporal Superonasdl lnferotemporal Tlmlng of Implant [N (%)I With keratoprostheala After keratoprosthesrs Antenor chamber dnglet [N (%)I Open Closed Unknown Postoperative IOP [N (%)I Low or nonet Normal Elevated Postoperatwe progressmn of glaucoma [N (%)I$ Postoperatwe medlcanona [N (%)I 36 34 35 (95) 1 (5) 16 (44) 19 (53) 1 (3) 29 (81) 7 (19) 5 (14) 3 (8) 28 (78) 5 (14) 29 (81) 2 (6) 5 (14) 9 (25) * One eye had a second Ahmed glaucoma dramage Implant poaltmned superotemporally for progressmn of glaucoma, which was not Included m the analysla m this table. t Includes preoperatwe assessment and postoperauve sound hmnucroscope (UAM). evaluation by ultra- $ Inrraocular pressure (IOP) at most recent follow-up “Low or none” Includes three patients who had keratoprosthesls removal due to ussue necroslb or mfectwn and two patwnts wth ret& detachment. § Progresswn of glaucoma by elevation of mtraocular pressure or changes of the waudl field and optic nerve head. The majority of these eyes (4 of 5, 80%) had pre-exlstmg glauconu wrth advanced optic nerve damage. 753 Ophthalmology Volume105,Number4, April 1998 Figure 3. Ultrasound biomicroscopy in a patient with keratoprosthesis and glaucoma. The anterior chamber anele (asterisk) is ooen. The iris and retroprosthesls membrane form a smgle sheet (arrow) that 1sadherent to the ciliary body (cb) at one end and the keratoprosthesis at the other. C = cornea; the central area of the cornea (not shown) contains the type I keratoprosthesis. without glaucoma drainage implants (P = 0.013, &i-square), with the type II through-the-lid keratoprosthesis used in a greater proportion of the patients with glaucoma drainage devices (50%) compared with those without such devices (16%). Comparison of the diagnoses between the patients with and without glaucoma drainage implants was significantly different (P = 0.027, chisquare). A greater proportion of patients with pemphigoid and Stevens-Johnson syndrome were treated with glaucoma drainage implants, whereas patients with herpetic keratitis or graft failure were more likely to have been treated without glaucoma drainage devices. The proportion of patients with chemical bums was similar in patients with and without glaucoma drainage implants (22% and 26%, respectively). As shown in Figure 1, the postoperative vision was improved to between 20/200 and 20120 from the preoperative vision (light perception, hand movements, finger counting) in the majority (63%) of the 55 eyes treated with keratoprosthesis. The postoperative vision was the same or only slightly improved in 17% and worse in 20%, including those eyes that developed vision-threatening postoperative complications. Glaucoma was found in the majority of eyes (64%) treated with keratoprosthesis, occurring before surgery in 36% of eyes and after surgery in another 28% of eyes (Fig 1). In a minority of eyes (36%), no evidence of glaucoma was found before surgery or during the postoperative follow-up period. Examples of the postoperative appearance of the type I and type II keratoprostheses are shown in Figure 2. Of the patients with keratoprosthesis and glaucoma drainage implant, the majority of implants were Ahmed valves (9.5%), and most (97%) were positioned in the superior quadrants (Table 2). The majority of patients (81%) had glaucoma drainage devices implanted at the same time as the keratoprosthesis; however, 19% of patients underwent two separate procedures, with later glaucoma drainage device implantation for the treatment of postkeratoprosthesis glaucoma. Although the angle was not examined in the majority of patients (78%), preoperative assessment and postoperative 754 evaluation by ultrasound biomicroscopy showed an open angle in 14% and a closed angle in 8% of eyes (Fig 3). In patients with functioning glaucoma drainage implants, B-mode ultrasound showed a collection of fluid (aqueous) in the pseudocyst around the drainage implant plate (Fig 4). The postoperative IOP by tactile estimation was normal in 81% and elevated in 6% of eyes (Table 2). The IOP was low or none in 14% (5 eyes), including three patients who had keratoprosthesis removal due to tissue necrosis or infection and two patients with retinal detachment. Postoperative antiglaucoma medications were used in 25% of eyes, usually systemic carbonic anhydrase inhibitors, for treatment of elevated IOP or progressive visual field or optic nerve changes in the eye with the keratoprosthesis or the fellow eye. Despite the use of drainage implants, postoperative elevation of IOP or progressive glaucomatous visual field and optic nerve head changes were observed in five eyes (14%). Most of these eyes (4 of 5, 80%) with progressive glaucoma after surgery had advanced glaucomatous optic nerve damage before placement of the glaucoma drainage implant (Fig 5). As listed in Table 3, there were nine complications attributable to the glaucoma drainage implants in five separate eyes (14% of eyes with drainage implants). The most common complication was obstruction of the tube, which occurred in four eyes (11%). Of the patients who developed blocked tubes, two tubes were repaired surgically and two were treated with antiglaucoma medications. Erosion of the conjunctiva and the scleral patch graft over the tube was found in one eye (3%). This required several revisions with scleral and pericardial patch grafts, which ultimately resulted in stable coverage of the tube. The B-mode ultrasound performed during the immediate postoperative period showed three eyes with anterior choroidal effusions and one eye with limited suprachoroida1 hemorrhage, all of which resolved without clinical sequelae. In the eyes with keratoprosthesis and drainage implant, several vision-threatening complications developed that were not attributed to the drainage implant. These included two eyes with retinal detachment, two eyes with retinal detachment and infection, and one eye with infection, which required removal of the keratoprosthesis in three eyes. Discussion Keratoprosthesis may be the only option for visual rehabilitation of certain patients with severe ocular surface Figure 4. A B-mode ultrasound m a patlent wth keratoprosthesls and glaucoma dramage Implant. A collectmn of low-echogemc flutd (aqueous) IS present wthm the pseudocyst around the glaucoma dramage Implant plate (arrow). Netland et al * Glaucoma Associated with Keratoprosthesis Intermittent responses to V&E disease, including those with ocular cicatricial pemphigoid, Stevens-Johnson syndrome, end-stage dry eye, severe chemical burns, and repeated failure of penetrating keratoplasty. However, these patients may have a high incidence of glaucoma even before keratoprosthesis implantation. In a series of 111 patients (none with keratoprosthesis) with ocular cicatricial pemphigoid, 29 patients (26%) were found to have glaucoma, mostly in the ad- & SC Figure 5. Progressive visual field loss in a patient with keratoprosthesis and glaucoma drainage implant. A 61-yearold man with bilateral blmdness due to chemical burn and elevated mtraocular pressure was treated with type I keratoprosthesis and an Ahmed valve placed m the superonasal area. After surgery, the tactile estimation of the intraocular pressure was Judged to be 15 to 20 mmHg. After opening the conlunctiva over the keratoprosthesis optic, Goldmann perimetry showed advanced glaucomatom vrsual field loss (A). Six months later, the visual field had worsened despite treatment with systemic carbonic anhydrase inhibitors (B). A second Ahmed glaucoma valve was implanted supertemporally, and 6 months later, the field had not worsened. vanced stage.” We found glaucoma before surgery in 36% of eyes in our patient population. The long-term problem of glaucoma after keratoprosthesis implantation is becoming increasingly recognized. At a meeting of the Keratoprosthesis Study Group in 1992, the moderator expressed the general consensus that “a major disappointment was the frequency of intractable glaucoma, resulting in loss of vision after prelimi- 755 Ophthalmology Table 3. Complications Associated Implant in Patients with with Glaucoma Keratoprosthesis* Volume 10.5, Number 4, A@ Drainage No. (%) Blocked tube? Erosion of conjunctiva over tube and aqueous leak Choroidal effusion$ Suprachoroidal hemorrhage+ 4 1 3 1 Total 9 (25) complications (11) (3) (8) (3) * Total N = 36. Complications in this group that were not attributable to the glaucoma drainage implant included three patients with removal of keratoprosthesis (one retinal detachment, one infection with retinal detachment, and one Infection) and two others with retmal detachment (one following infecnon). t Of the patients with obstructed tubes postoperanvely, two were repaired surgically and two were treated with antiglaucoma medications. $ Observed by B-mode period; resolved without ultrasound sequelae. during the immediate postoperative nary success with a keratoprosthesis.“” In a series of osteo-odontokeratoprostheses, 41% of the patients had glaucoma before surgery and another 33% developed it after surgery.” Other investigators have discussed the problem of glaucoma in eyes with keratoprosthesis.12.‘3 One report mentions the use of a small silicone tube for treatment of intractable glaucoma.14 Without treatment of postoperative glaucoma, the long-term prognosis for preservation of vision is poor for many patients with keratoprosthesis. In addition to the eyes with glaucoma before keratoprosthesis, we also observed the postoperative appearance of glaucoma in another 28% of eyes, bringing the prevalence of glaucoma to approximately two thirds in eyes with keratoprosthesis. In our clinical experience, we found that a glaucoma drainage device can be readily implanted together with a keratoprosthesis or at a later date. Glaucoma drainage implants prevent the severe elevation of IOP that occurs in some patients treated with keratoprosthesis alone. Postoperative complications attributable to glaucoma drainage implants have not been common in our patients with keratoprosthesis. Although progression of end-stage glaucoma can occur despite use of glaucoma drainage implants, these implants are effective in reducing the IOP and preventing glaucomatous optic nerve or visual field changes in the majority of patients. In eyes with keratoprosthesis and glaucoma, we observed both open angles and angles closed due to formation of peripheral anterior synechiae by preoperative assessment using biomicroscopy and postoperative evaluation using ultrasound biomicroscopy. Total removal of the iris during keratoprosthesis surgery was intended to decrease the likelihood of subsequent secondary angleclosure glaucoma. However, glaucoma was not eliminated in 21 (58%) of the 36 eyes treated with total removal of the iris during the surgical procedure. It is likely that multiple mechanisms of glaucoma, including both openand closed-angle mechanisms, can occur in glaucoma as756 1998 sociated with keratoprosthesis, which may be comparable to the heterogeneous causes of glaucoma associated with penetrating keratoplasty.” In our patients with keratoprosthesis and glaucoma, treatment with glaucoma drainage implants effectively reduced the IOP in nearly all patients, some requiring additional antiglaucoma medications. Because topical antiglaucoma medications are of little or no use in these patients, systemic carbonic anhydrase inhibitors were preferentially used when medical therapy was required to further reduce the IOP. Cyclodestructive procedures have been recommended in the past for patients with keratoprosthesis and elevated IOP, and pars plana filter has been recommended for select patients.6 In our patients, however, filtration surgery usually was not possible because of complete removal of conjunctiva in type II through-the-lid keratoprosthesis or severely scarred conjunctiva in type I keratoprosthesis procedures. Complications directly attributable to the glaucoma drainage implant developed in nine eyes (25%) in patients with keratoprosthesis and drainage implant. The majority of patients were treated with the Ahmed valve, in which a tapered chamber valve provides resistance to aqueous flow. This implant is associated with fewer complications of overfiltration in the immediate postoperative period compared with other drainage devices.16 The complications in our patients were repaired surgically or treated medically. Our complication rate may have been relatively low because of the aqueous flow-resistance of the Ahmed valve, adequate coverage of the drainage devices with sclera and in many instances skin, and the removal of intraocular contents (lens, vitreous, and iris) that could potentially block the tube. We did not assess these patients for motility disturbances, which, if found, could be caused by multiple factors and would be of little or no functional significance for the patient. Focal or diffuse cornea1 edema, which can account for nearly one fifth of the complications after glaucoma drainage implants,17 cannot occur after replacement of the cornea with the polymethylmethacrylate keratoprosthesis. We observed continued progression of glaucoma in 5 (14%) of 36 eyes with keratoprosthesis and glaucoma drainage implant. The majority of these eyes (4 of 5) with progressive postkeratoprosthesis glaucoma had preexisting glaucoma with advanced glaucomatous optic nerve damage, which had been obscured from view before surgery. In the eyes with elevation of IOP despite drainage device implantation (2 of 5), this may have been caused by increased resistance to aqueous flow through the pseudocapsule around the drainage implant plate, unrecognized blocked tube, or other failures of the drainage implant procedure. In eyes with continued optic nerve or visual field changes and apparently normal IOP (3 of 5), there may have been unrecognized elevation of the IOP or intermittent elevation of the IOP, which could occur with episodes of uveitis. In addition, the eyes with preexisting glaucomatous damage may have been abnormally sensitive to otherwise normal levels of IOP, which has been termed “low-tension glaucoma equivalent.” ‘* A limitation of our study was that IOP was difficult Netland et al * Glaucoma Associated with Keratoprosthesis to measure, particularly in those patients with type II through-the-lid keratoprosthesis. Although the McKayMarg tonometer used on the sclera has been suggested,6 we have found use of tonometers of little value after type I keratoprosthesis and of no value after type II keratoprosthesis. Attempts to use the pneumotonometer and the tonopen on the sclera of our patients with type I keratoprosthesis showed considerable overestimation of the IOP. In our patients with keratoprosthesis, digital palpation of the globe was the most practical available method for assessment of IOP. Despite its uncertainties, digital palpation of the globe is useful for identifying a marked increase of the IOP. In a study of tactile assessment of 138 eyes, palpation did not indicate an IOP greater than 30 mmHg for any eye in which the applanation pressure was below 30 mmHg.lg However, palpation did not identify two (29%) of seven of eyes with an applanation pressure greater than 30 mmHg.lg This degree of failure to detect elevated IOP by digital palpation could have influenced the success rate after glaucoma drainage implant determined in our study of eyes with keratoprosthesis. Up to 8 (29%) of 29 “successes” in our study of eyes with keratoprosthesis and drainage implants actually may have had elevated IOP, which would decrease the success rate from 81% (29 of 36 eyes) to 58% (21 of 36 eyes). In conclusion, preoperative elevation of IOP is common in patients who are candidates for keratoprosthesis. Many additional patients develop glaucoma after keratoprosthesis surgery. With improvements in management of inflammatory and infectious complications of keratoprosthesis, glaucoma emerges as an important long-term complication of this procedure. Glaucoma associated with keratoprosthesis is treated effectively with glaucoma drainage implants, which can control the IOP in most patients, with some requiring additional antiglaucoma medications. Progression of glaucoma can occur despite use of glaucoma drainage implants, usually in patients with advanced glaucomatous optic nerve damage. Postoperative monitoring of the optic nerve and visual field is, therefore, recommended even in those patients with keratoprosthesis who have been treated with glaucoma drainage implants. Acknowledgment. The authors thank Dr. C. Stephen Foster for patient referrals. References 1. Tugal-Tutkun I, Akova YA, Foster CS. Penetrating keratoplasty in cicatrizing conjunctival diseases. Ophthalmology 1995; 102576-85. 2. Soong HK. In: Krachmer JH, Mannis MJ, Holland EJ, eds. 3. 4. 5. 6. 7. 8. 9. 10. Il. 12. 13. 14. 15. 16. 17. 18. 19. Cornea: Surgery of the Cornea and Conjunctiva. St. Louis, Missouri: Mosby-Year Book, Inc, 1997; chap. 145, pp. 1781-8. Dohlman CH. Keratoprosthesis. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea: Surgery of the Cornea and Conjunctiva. St. Louis, Missouri: Mosby-Year Book, Inc, 1997; chap. 151, pp. 1855-63. Dohlman CH, Doane MG. Some factors influencing outcome after keratoprosthesis surgery. Cornea 1994; 13:2148. Bath PE, McCord RC, Cox KC. Nd:YAG laser discission of retroprosthetic membrane: a preliminary report. Cornea 1983;2:225-8. Girard LJ. Keratoprosthesis. Cornea 1983;2:207-24. Dohlman CH, Waller SG, Netland PA. Keratoprosthesis surgery. In: Lindquist TD, Lindstrom RL, eds. Ophthalmic Surgery: Looseleaf and Update Service. St. Louis, Missouri: Mosby-Year Book, Inc, 1996; update 4, pp. VLl24. Doane MG, Dohlman CH, Bearse G. Fabrication of a keratoprosthesis. Cornea 1996; 15:179-84. Tauber J, Melamed S, Foster CS. Glaucoma in patients with ocular cicatricial pemphigoid. Ophthalmology 1989; 96:33-7. Roper-Hall MJ. Foreword to the Proceedings of the First Keratoprosthesis Study Group Meeting, Miami. Refract Cornea1 Surg 1993;9:185. Marchi V, Ricci R, Pecorella I, et al. Osteo-odonto-keratoprosthesis. Description of surgical technique with results in 85 patients. Cornea 1994; 13: 125-30. Legeais JM, Renard G, Pare1 JM, et al. Keratoprosthesis with biocolonizable microporous fluorocarbon haptic. Preliminary results in a 24-patient study. Arch Ophthalmol 1995; 113:757-63. Kozarsky AM, Knight SH, Waring GO III. Clinical results with a ceramic keratoprosthesis placed through the eyelid. Ophthalmology 1987;94:904- 11. Falcinelli GC, Barogi G, Colliardo P, Taloni M, Graziani L. New possibilities in the field of OOKP. Contribution to glaucoma surgery. First Congress Biomaterials in Ophthalmology. An Interdisciplinary Approach. Proceedings of the University of Bologna 1990; 13l-5. Sugar A, Higginbotham EJ, Glaucoma associated with penetrating keratoplasty. In: Ritch R, Shields MB, Krupin T, eds. The Glaucomas, 2nd ed. St. Louis: Mosby, 1996; v. 2, chap. 63. Coleman AL, Hill R, Wilson MR, et al. Initial clinical experience with the Ahmed Glaucoma Valve implant. Am J Ophthalmol 1995; 120:23-31. Siegner SW, Netland PA, Urban RC Jr, et al. Clinical experience with the Baerveldt glaucoma drainage implant. Ophthalmology 1995; 102:1298-307. Epstein DL. Low tension glaucoma. In: Epstein DL, ed, with Allingham RR. Schuman JS, eds. Chandler and Grant’s Glaucoma, 4th ed. Baltimore: Williams & Wilkins, 1997; 199-211. Baum J, Chaturvedi N, Netland PA, Dreyer EB. Assessment of intraocular pressure by palpation. Am J Ophthalmol 1995;119:650-1. 757