* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Methotrexate subcutaneous injection - airedale
Survey
Document related concepts
Transcript
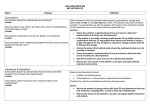
DOCUMENT TITLE: METHOTREXATE SUBCUTANEOUS INJECTION (LICENSED) RHEUMATOLOGY GUIDE FILENAME PHA_Medicines management_Shared Care Guideline_Methotrexate Subcutaneous injection (licensed) Rheumatology Shared Care Guideline VERSION № 6 DATE OF ISSUE 01/11/2007 REVIEW INTERVAL 2 Years AUTHORISED BY Drug and Therapeutics Committee AUTHOR Dr Shabina Sultan – Consultant Rheumatologist Linda Stewart – Pharmacist Linda Sigsworth – Rheumatology Nurse Specialist EMAIL ADDRESS OF AUTHOR [email protected] COPY № 2 LOCATION OF COPIES 1. SHAREPOINT 2. AIREDALE NHS FOUNDATION TRUST WEBSITE ASSOCIATED WORKING INSTRUCTIONS N/A LOCATION OF WORKING INSTRUCTIONS N/A TO BE VIEWED TRUST WIDE X PHARMACY ONLY DOCUMENT REVIEW HISTORY REVIEW DATE REVIEWED BY CHANGES October 2008 June 2008 Dr K. Lindsay – Locum Consultant Rheumatologist Linda Stewart - Pharmacist Sarah Redfern - Riley Locum Rheumatology Nurse 20/7/2009 Linda Stewart Expiry date extended as we are waiting for the New Yorkshire Guidelines to come out later this year 30/12/2009 Linda Stewart – Pharmacist Dr S Sultan – Consultant Rheumatologist Monitoring and live vaccine information updated 31/01/2011 Linda Stewart and Dr Sultan Expiry date extended whilst document being reformatted 31/5/2011 Linda Stewart – Pharmacist Dr Reddy – Consultant Rheumatologist Dr Sultan – Consultant Rheumatologist Document reformatted and responsibilities of GP and consultant added. May 2013 Linda Stewart – Pharmacist Dr Reddy – Consultant Rheumatologist Dr Sultan – Consultant Rheumatologist Document amended to take into account the change to licensed subcutaneous methotrexate and updated. September 2013 Linda Stewart – Pharmacist Dr Sultan – Consultant Rheumatologist Shingles vaccine added to ‘avoid live vaccines section’ July 2014 Linda Stewart – Pharmacist Dr Sultan – Consultant Rheumatologist Frequency of monitoring of U&Es amended September 2015 Linda Stewart – Pharmacist Dr Sultan – Consultant Rheumatologist Kelly Hayes-Head – CNS Rheumatology Removed contra-indication to shingles vaccine Blood cell ranges amended September 2017 NB: ONLY SHAREPOINT VERSION OR NUMBERED COPIES IN STATED LOCATIONS ARE VALID FOR OPERATIONAL USE In keeping with Yorkshire Rheumatology Guidelines June 2009 In accordance with BSR/BHPR guidelines 2008 Revised September 2015, Review date September 2017 Agreed by DTC May 2013 METHOTREXATE SUBCUTANEOUS INJECTION RHEUMATOLOGY GUIDE GENERAL STATEMENTS PHARMACOLOGICAL SUMMARY INDICATIONS FOR THERAPY CONTRAINDICATIONS Methotrexate should be initiated in secondary care under specialist supervision. Prescribing and monitoring will be carried out by the Rheumatology Department throughout the course of treatment. Patients receive supplies of drug from hospital via home delivery The full summary of product characteristics (SPC) should be read before prescribing. Methotrexate Subcutaneous Injection SPC Methotrexate is a competitive inhibitor of dihydrofolate reductase and thus interferes with the process of DNA synthesis and cell replication. This may not account for its full action in rheumatoid arthritis. N.B. at the doses used in rheumatology, methotrexate is classed as an immunosuppressive drug and not a cytotoxic agent. Active rheumatoid arthritis in adult patients Steroid sparing agent in Polymyalgia rheumatica, Temporal arteritis Immunosuppressant in vasculitis Known hypersensitivity to methotrexate Pregnancy or planned pregnancy (stop at least 6/12 before considering conception, for both male and female patients) Breastfeeding Severe immunodeficiency. Serious infection. Severe renal (CrCl <20ml/min) Severe hepatic impairment pre-existing blood dyscrasias, such as bone marrow hypoplasia, leukopenia, thrombocytopenia, or significant anaemia, AVOID LIVE VACCINATIONS (BCG, MMR, Poliomyelitis (live oral vaccine), Rotavirus (live oral vaccine), Typhoid (live oral vaccine), Varicella-Zoster vaccine (Zostavax@) and Yellow Fever) Zostavax® is a live attenuated vaccine. Caution needs to be exercised in the use of live vaccines in people who may be immunosuppressed. However the DH guidelines for the use of Zostavax® state: “Therapy with low-doses of methotrexate (<0.4 mg/Kg/week), for treatment of rheumatoid arthritis, psoriasis, polymyositis, sarcoidosis, inflammatory bowel disease, and other conditions are not considered sufficiently immunosuppressive and are not contraindications for administration of zoster vaccine”. For more detail see Vaccinations Rheumatology Shared Care Guideline In keeping with Yorkshire Rheumatology Guidelines June 2009 In accordance with BSR/BHPR guidelines 2008 Revised May 2013, Review date September 2015 Agreed by DTC May 2013 1 of 5 METHOTREXATE SUBCUTANEOUS INJECTION RHEUMATOLOGY GUIDE CAUTIONS Renal impairment: inform specialist if GFR falls below 30ml/min as increased risk of toxicity Alcohol consumption must not exceed national recommendations (BSR) Intercurrent infection: Methotrexate use is associated with a small increased risk of infection. Chicken pox/varicella zoster can be fatal in immunosuppresed patients: varicella zoster immunoglobulin should be given to susceptible patients (not known to be immune to chicken pox) where contact occurs, preferably within 3 days but up to 10 days after exposure. Systemic antivirals should be given if infection is suspected In the presence of significant infection requiring antibiotics DMARDs should be stopped . They can be restarted when clear of infection and /or the antibiotic course has been completed. POTENTIAL DRUG INTERACTIONS INITIAL SCREENING PRESCRIBING NSAID USE: May increase the bioavailability of methotrexate by slowing renal excretion. This is rarely of clinical significance and only very rarely causes toxicity. Folate antagonists e.g. phenytoin, trimethoprim, co-trimoxazole, penicillins tolbutamide See BNF for full list of interactions CXR in last 6 months, FBC, LFTs and U&E checked in rheumatology Clinic Pulmonary function tests in patients with RA and if underlying chest disease/ smoker . Hepatitis B and C serology If TLCO < 70% or clinical concern – HRCT lungs advisable If patient is unsure if they have had chicken pox need to check Varicella Zoster Virus IgGs Methotrexate subcutaneous injection should be given given ONCE weekly. The starting dose is usually 10mg but can vary. Increased as appropriate by 2.5- 5 mg every 2-4 weeks. Usual maximum dose 25mg/ week. Prescribe folic acid supplements - 5mg weekly the day after methotrexate to reduce toxicity. Analgesics and NSAIDs are not contra-indicated with methotrexate and are often needed. Pneumovax and annual ‘flu vaccine should be given In keeping with Yorkshire Rheumatology Guidelines June 2009 In accordance with BSR/BHPR guidelines 2008 Revised September 2015, Review date September 2017 Agreed by DTC May 2013 2 of 5 METHOTREXATE SUBCUTANEOUS INJECTION RHEUMATOLOGY GUIDE MONITORING FBC, LFTs: 2 weekly for 2 months, then monthly for 4 months, then 3 monthly (assuming dose stable). U&Es, ESR or CRP 3 monthly. If any increase in dose, monitor FBC, LFTs every 2 weeks for 2 months, then revert to patient’s usual monitoring arrangements If the bloods are abnormal BUT above the specified values below, consider the trend. If the patient is well, simply repeat count in one week but continue DMARD. If persistently low CONTACT AGH as dose adjustment may be required If any of the following apply please contact AGH urgently and withhold DMARDs WCC Neutrophils Platelets AST/ALT/AlkPhos <3.0 x 109/l <1.5 x 109/l <100 x 109/l >2 x upper limit of normal Unusual bruising, fever, sore throat (check FBC first and if the above apply: contact AGH) Breathlessness and/ or cough unexplained by infection or persistent despite antibiotics Unexplained fall in albumin (increased risk of methotrexate toxicity) Significant deterioration in renal function or if GFR falls below 30ml/min ADVERSE EVENTS Folic acid 5mg should be prescribed once a week the day after the methotrexate dose. However the rheumatology team may suggest increasing this dose to 5mg every day, except on the day of methotrexate, if significant side effects occur e.g. where mouth ulcers or hair loss become problematic. Common: Nausea, anorexia, oral ulcers, hair loss, abdominal pain, diarrhoea and headaches, drowsiness, blurred vision Uncommon: Rash, thrombocytopenia, and neutropenia. Rare: Hepatotoxicity, Pulmonary toxicity (acute pneumonitis or chronic pulmonary fibrosis). See BNF for full list of adverse events In keeping with Yorkshire Rheumatology Guidelines June 2009 In accordance with BSR/BHPR guidelines 2008 Revised September 2015, Review date September 2017 Agreed by DTC May 2013 3 of 5 METHOTREXATE SUBCUTANEOUS INJECTION RHEUMATOLOGY GUIDE RESPONSIBILITY OF THE SPECIALIST INITIATING TREATMENT SUMMARY RESPONSIBILITY OF OTHER PRESCRIBERS To assess the suitability of the patient for this treatment To perform the baseline tests To inform the patient of the side effects of methotrexate and long term monitoring required before initiating treatment To ensure that the patient is aware that they must use reliable contraception To initiate treatment and supply a METHOTREXATE monitoring booklet and patient information leaflet To assess and monitor the patient’s response to treatment To adjust treatment as clinically necessary. Supporting and advising GPs To monitor the patient for adverse events and report to the GP, and where appropriate, the Commission on Human Medicines / MHRA (Yellow card scheme). SUMMARY The General Practitioner: To monitor the patient’s overall health and wellbeing. Monitor the patient for adverse drug reactions and remain vigilant to the risk of potential drug interaction. To ensure that the patient is using reliable contraception Prescribe folic acid therapy as recommended by the hospital specialist. Ensure methotrexate is included on the electronic patient record in order to minimise the chances of prescribing other drugs that would interact with methotrexate. Report adverse events to the specialist service, and where appropriate, the Commission on Human Medicines / MHRA (Yellow card scheme). To stop treatment on the advice of the hospital specialist or if the GP feels it is clinically indicated (If in doubt STOP the treatment and contact the Specialist as soon as possible). In keeping with Yorkshire Rheumatology Guidelines June 2009 In accordance with BSR/BHPR guidelines 2008 Revised September 2015, Review date September 2017 Agreed by DTC May 2013 4 of 5 METHOTREXATE SUBCUTANEOUS INJECTION RHEUMATOLOGY GUIDE CONTACTS A patient information leaflet has been issued to your patient If any problems occur please contact: Dr Sultan, Consultant rheumatologist’s 01535 292067 secretary: Dr Reddy, Consultant rheumatologist’s 01535 292080 secretary: Rheumatology Nurse specialist/ advice line: 01535 292084 Pharmacy: 01535 293503 Access to shared care guidelines is available via the internet at Airedale NHS Trust: http://www.airedale-trustformulary.nhs.uk/default.asp In keeping with Yorkshire Rheumatology Guidelines June 2009 In accordance with BSR/BHPR guidelines 2008 Revised September 2015, Review date September 2017 Agreed by DTC May 2013 5 of 5